Cow's milk protein allergy (CMPA) is being seen more frequently on a daily basis in pediatric consultations. It shares symptoms with gastroesophageal reflux (GER), which can complicate the differential diagnosis.
AimsTo attempt to corroborate the presence of acid GER in children with CMPA, as well as to find a characteristic profile through the 24-hour pH monitoring study in children with GER and CMPA
MethodsThe intraesophageal pH monitoring studies performed on 47 children with CMPA were reviewed. The measurements in all the studies were carried out within a 24-hour period using Digitrapper® equipment with a multi-use GeroFlex® catheter, after calibration with pH 7 and pH 1 buffer solutions.
ResultsOf the 47 children, 23 were boys (32.4%) and 24 were girls (33.8%) and the mean age was 5±3.7 years. Fourteen of the 47 children (29%) presented with GER, according to the result of the 24-hour intraesophageal measurement. Only 2 of the 47 patients studied fit the phasic profile.
ConclusionsThe findings show the existing relation between the two pathologies. Nevertheless, it is important to determine the presence of non-acid or weak acid reflux, because their existence can increase this association.
La alergia a las proteínas de la leche de vaca (APLV) es una entidad que se ve día a día con mayor frecuencia en la consulta pediátrica. Comparte síntomas con el reflujo gastroesofágico (RGE), lo que en un momento podría dificultar el diagnóstico diferencial.
El objetivo del presente trabajo fue tratar de corroborar la presencia de RGE ácido en niños con APLV, así como encontrar un perfil característico a través del estudio de monitorización de pH de 24 h en niños con RGE y APLV.
Material y métodosSe revisaron los estudios de monitorización de pH intraesofágico en 47 niños con RGE y APLV. En todos ellos se realizó la medición de 24 h, con equipo Diggitrraper, con catéter Gero Flex Multiusos, previa calibración con soluciones buffer pH de 7 y pH de 1. De los 47 niños, 23 fueron masculinos (32.4%) y 24 femeninos (33.8%), la media de edad fue de 5±3.7 años, 14 de 47 (29%) niños presentaron RGE de acuerdo con el resultado de la medición intraesofágica de pH de 24h, solo se encontró el perfil fásico en 2 pacientes de los 47 estudiados. Los hallazgos demuestran la relación que existe entre ambas afecciones, aunque es importante determinar la presencia de reflujo no ácido o débilmente ácido lo cual podría incrementar esta asociación.
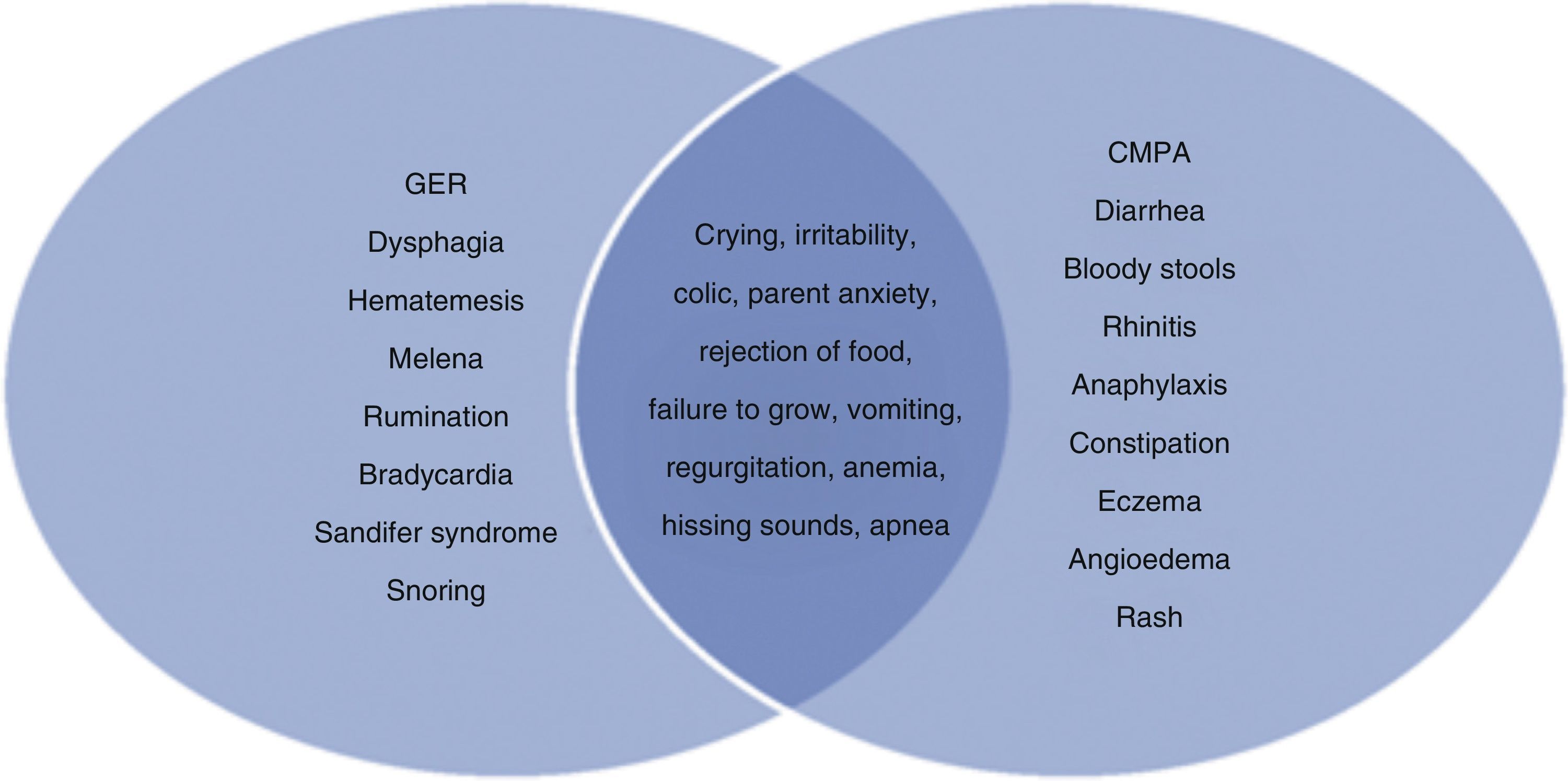
Cow's milk protein allergy (CMPA) is an entity that is being seen more and more in the daily pediatric practice and its prevalence is from 2.2 to 2.8%.1,2 Real prevalence in Mexico is not exactly known but is assumed to be approximately 5 to 7%3. CMPA is defined as an immunologic reaction to proteins in cow's milk that is accompanied with signs and symptoms. The clinical manifestations are many and include gastrointestinal, respiratory, dermatologic, neurologic, and systemic presentations.3,4 Crying, irritability, colic, regurgitation and/or vomiting, constipation, and dyschezia are among its gastrointestinal manifestations. These same manifestations can also be found in children with gastroesophageal reflux (GER) often making the differential diagnosis between the 2 entities difficult5–7 (fig. 1). GER is defined as the passage of the gastric content toward the esophagus, with or without regurgitation or vomiting. It is a physiologic process that presents in lactating infants and in children. Episodes last<3minutes and generally occur in the postprandial period.8 GER is one of the main motives for medical consultation in Pediatrics. The prevalence of regurgitation in lactating infants of 0 months of age is 34.4%, at 2 months of age it is 19.1%, at 4 months of age it decreases to 13.3%, and at 6 months of age it is only 2.9%.9 Different studies point out the association of GER in children with CMPA and refer to the fact that this association can be found in up to 66% of cases.10–12 The determination of intraesophageal pH during a 24-hour period is currently the criterion standard in the diagnosis of acid GER. It precisely identifies each episode of GER in the esophagus and distinguishes between physiologic and pathologic GER.8,9 It has also been stated that the image of 24-hour intraesophageal pH determination that presents in children with CMPA is in a certain way characteristic, illustrating a phasic curve. Salvatore and Vandenplas describe this pattern as a slow and progressive lowering of intraesophageal pH between feedings.7
The aim of the present study was to determine the frequency of acid GER in children with CMPA, as well as to attempt to find a characteristic profile through the 24-hour intraesophageal pH test in children with GER and CMPA.
MethodsA review was carried out of the 24-hour intraesophageal pH studies of 47 children presenting with CMPA that were seen at the Gastroenterology and Nutrition Service of the Instituto Nacional de Pediatría. Their diagnoses were confirmed through the suppression and challenge test performed according to the recommendations of the European Academy of Allergy and Clinical Immunology.13 The test was performed once the symptomatology had remitted with the exclusion diet. It began with 1ml of first formula and every 20minutes was increased by the amounts of 5ml, 10ml, 20ml, 40ml, 50ml, and 100ml. If any symptoms presented during this period (2h 20minutes) the procedure was suspended and the test was regarded as positive. If no symptoms presented during the procedure and the child was released, but any symptom presented within a period of 2 weeks, the test was also considered positive. In the children that received treatment with prokinetics and/or proton pump inhibitors, these agents were suspended 7 days prior to the study. Twenty-four hour intraesophageal pH measurement was carried out on all the patients using Digitrapper equipment and the external reference GeroFlex multiuse catheter after calibration with pH 7 and pH 1 buffer solutions. The catheter was placed intranasally with the Ströbel formula, always corroborating through chest x-ray that it was in place 3cm above the gastroesophageal junction.
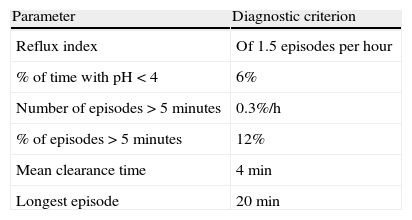
The following variables were analyzed in all the cases: age, sex, reflux index, total number of reflux episodes, number of preprandial reflux episodes, and number of postprandial reflux episodes. The intraesophageal pH measuring study was regarded as positive when there were 2 or more Boyle criteria (see Table 1) and the phasic pattern described by Salvatore and Vandenplas was intentionally looked for.7
The statistical analysis was carried out with the SPSS 16.0 program, using descriptive statistics, means ± standard deviation for the quantitative variables, and frequencies for the qualitative variables.
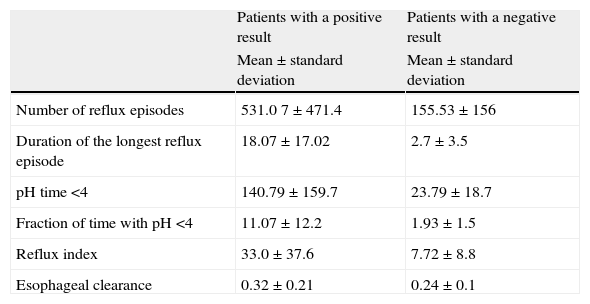
ResultsOf the 47 children, 23 were boys (32.4%) and 24 were girls (33.8%) and the mean age was 5 ± 3.7 years. Fourteen of the 47 (29%) children presented with GER according to the results of the 24-hour intraesophageal pH monitoring test. Table 2 shows the variables analyzed in the 47 children, as well as the results of the patients that had positive and negative intraesophageal pH determination. The mean time with a pH under 4 was 140.79 s and a reflux that could be considered severe was found, given that the mean reflux index was 33±37.6.
Intraesophageal pH characteristics in the patients with positive and negative results.
| Patients with a positive result | Patients with a negative result | |
| Mean±standard deviation | Mean±standard deviation | |
| Number of reflux episodes | 531.0 7±471.4 | 155.53±156 |
| Duration of the longest reflux episode | 18.07±17.02 | 2.7±3.5 |
| pH time <4 | 140.79±159.7 | 23.79±18.7 |
| Fraction of time with pH <4 | 11.07±12.2 | 1.93±1.5 |
| Reflux index | 33.0±37.6 | 7.72±8.8 |
| Esophageal clearance | 0.32±0.21 | 0.24±0.1 |
There was a clear predominance in relation to the number of postprandial reflux episodes.
Only 2 of the 14 patients (14%) fit the phasic pattern.
DiscussionBoth CMPA and GER are the 2 main pathologies that are seen most frequently in children under one year of age.
Acid GER frequency in our children was 29%, compared with that reported in the literature. Iacono et al. described a GER frequency of 41.8% in patients with GER mediated by IgE;10 Semeniuk and Kaczmarski found an association of 49% between GER and CMPA.11
Farahmand et al. conducted a study on 81 children with GER. They were studied for CMPA, and 54 of the patients (66.7%) were found to present the signs and symptoms of CMPA.12
Perhaps the frequency variability of GER in children with CMPA is due to the diagnostic methods used for determining this pathology. Iacono et al. used IgE-mediated tests, whereas Farahmand et al. used the suppression and challenge test. Nevertheless, such a high frequency was due to the fact that first the GER diagnosis was made and then the diagnostic evaluation for CMPA was made.10–12It is important to mention that in our study, there was an improvement in both GER and CMPA symptoms after beginning CMPA treatment with hydrolyzed proteins. This suggests that GER is a manifestation of CMPA.
The findings of our study can explain the main clinical manifestations of these children characterized by irritability, crying, colic, and regurgitation.
Starting from the impedance monitoring studies, patients with CMPA have been seen to have acid as well as nonacid GER. In our study, we did not carry out impedance monitoring to corroborate the presence of non-acid reflux. Borreli et al. conducted a study on children with CMPA and GER diagnosed through impedance-pH monitoring and found a higher frequency of weak acid reflux episodes (105) as opposed to total acid reflux episodes (65) with a p<0.001.14 This fact makes it necessary to conduct more studies in this sense, given that there is probably a greater prevalence of GER secondary to CMPA.
There are hypotheses that explain the relation CMPA has to gastrointestinal tract motility. The allergic reaction conditions inflammation, which in turn causes histamine and serotonin secretion. In other words, the gastrointestinal tract reacts to the inflammation by altering motility.15 In addition to this association having been demonstrated by GER, it has also been demonstrated by altered gastric emptying. Ravelli et al. conducted a study on electrogastrography in children with CMPA and found a pattern of delayed gastric emptying.16
And even though the phasic pattern is described in the literature, we could not regard it as a constant finding in gastroesophageal reflux.
ConclusionsFinally, our study showed that CMPA had a 29% association with GER. We did not find a direct relation with the clinical manifestations - crying and irritability, especially, can be explained by this association - because there can be children presenting with a hypersensitive esophagus. In relation to the phasic pattern described by Salvatore and Vandenplas, we found only 2 patients; perhaps it is not a constant finding and does not necessarily indicate the presence of CMPA in children with GER. In the long run, if these children do not receive adequate treatment, CMPA will produce esophagitis, which in turn reduces lower esophageal sphincter pressure. It is important to conduct future impedance-pH monitoring studies to corroborate the presence of non-acid reflux in patients presenting with CMPA.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ramírez-Mayans JA, Toro-Monjaraz EM, Romero-Trujillo J, et al. Determinación de pH intraesofágico de 24 h en niños con alergia a las proteínas de la leche de vaca en un hospital de tercer nivel. Revista de Gastroenterología de México. 2014;79:3–6.