There is currently more evidence suggesting that early surgery should be the treatment of choice for acute calculous cholecystitis, although initial conservative treatment is also reported to be safe. Treatment decision depends on the conditions of the patient, surgical experience, and hospital infrastructure, given that early surgery cannot always be carried out. The aim of the present study was to correlate C-reactive protein values with other variables to determine those situations in which surgery cannot be delayed.
Materials and methodsA retrospective study was conducted on patients admitted to the hospital from the emergency service with the diagnosis of acute calculous cholecystitis. The patients were divided into 2groups: 1) patients that required urgent cholecystectomy and 2) patients that responded well to conservative medical treatment and later underwent deferred cholecystectomy.
ResultsA total of 238 patients (♂ 54.6%, ♀ 45.4%) were analyzed. Urgent surgery was performed on 158 patients, whereas the remaining 80 patients were released from the hospital following conservative treatment. The odds ratio of gangrenous cholecystitis presenting in acute cholecystitis for C-reactive protein was calculated in the logistic regression analysis, obtaining an OR of 1.088 and a 95% CI of 1.031-1.121.
ConclusionIn patients diagnosed with acute calculous cholecystitis, the combination of elevated values of C-reactive protein levels, gallbladder wall thickness, and number of leukocytes was correlated with less favorable clinical and gallbladder histologic states, resulting in a greater need for urgent surgical treatment.
Actualmente existe más evidencia de que la cirugía precoz debe ser el tratamiento de elección en la colecistitis aguda litiásica, aunque también es seguro llevar a cabo un tratamiento conservador de inicio. La decisión dependerá de las condiciones del paciente, la experiencia quirúrgica y la infraestructura hospitalaria, puesto que no siempre puede llevarse a cabo la cirugía en las primeras horas. El objetivo del estudio es correlacionar los valores de la proteína C reactiva junto con otras variables para determinar aquellas situaciones en las que no pueda demorarse la cirugía.
Material y métodosEstudio retrospectivo que incluyó a los pacientes ingresados desde el servicio de urgencias del hospital con diagnóstico de colecistitis aguda litiásica. Se dividieron en 2grupos: 1) pacientes que precisaron colecistectomía urgente y 2) pacientes con buena respuesta al tratamiento médico-conservador y realización posterior de la colecistectomía de forma diferida.
ResultadosSe analizó a un total de 238 pacientes (♂ 54,6%, ♀ 45,4%). Se llevó a cabo una cirugía de urgencias en 158 pacientes, mientras que los 80 pacientes restantes fueron dados de alta tras el tratamiento conservador. En el análisis de regresión logística, se calculó la razón de probabilidades de la colecistitis gangrenosa frente a la colecistitis aguda y se obtuvo para proteína C reactiva un OR=1.088 (IC 95%: 1.031-1.121).
ConclusiónEn pacientes con diagnóstico de colecistitis aguda litiásica, las cifras elevadas de forma conjunta de la proteína C reactiva, el espesor de la pared vesicular y los leucocitos se correlacionan con estados clínicos e histologías más desfavorables, lo que conlleva una mayor necesidad de tratamiento quirúrgico urgente.
Acute cholecystitis presents in 3 to 10% of all patients that present with abdominal pain, and gallstones are its most frequent cause (90-95%).1 There is great treatment variability with respect to cholecystitis in the medical literature, whether it be urgent surgical intervention or antibiotic treatment and deferred elective surgery.2 The stage of progression of cholecystitis influences the decision for surgical treatment, justified in cases of pathologic progression of acute cholecystitis: edematous cholecystitis encompasses the first 2-4 days and is the time when early surgery is considered the most adequate for surgical treatment. Cholecystitis then progresses to the necrotizing stage (3-5 days) and the suppurative stage (7-10 days), in which the wall thickening is chronologically due to hemorrhage, necrosis, thrombosis, and fibrous proliferation.1
Cholecystitis severity is classified into 3 grades: mild (grade I), moderate (grade II), and severe (grade III). Grade III cholecystitis is associated with organ dysfunction; in grade II, the degree of inflammation is most likely associated with greater surgical difficulty; grade I cholecystitis is associated with slight involvement of the gallbladder, in which cholecystectomy is a safe and low-risk procedure.3
The proposed hypothesis is that the combination of high levels of C-reactive protein (CRP), gallbladder wall thickness, and number of leukocytes in patients diagnosed with acute calculous cholecystitis is correlated with less favorable clinical state and gallbladder histology. There is a greater need for urgent surgery in the patients presenting with those conditions. In contrast, in the absence of that combination of events, together with a stable clinical state, the resolution of acute symptoms is more likely, as well as the possibility of deferred elective surgery. The aim of the present study was to evaluate the correlation of CRP, gallbladder wall thickening, leukocyte levels, and gallbladder histology with the need for urgent or delayed surgery in patients with acute calculous cholecystitis.
Materials and methodsThe retrospective study included patients admitted to the hospital from the emergency service diagnosed with acute calculous cholecystitis within the time frame of January 2011 to December 2015.
Patient data were obtained through a review of the case histories. The inclusion criteria were: patients older than 18 years of age seen at the emergency service and admitted to the hospital with the diagnosis of acute calculous cholecystitis, determination of CRP upon admission, abdominal ultrasound study consistent with acute calculous cholecystitis, and histologic diagnosis of calculous cholecystitis (acute or gangrenous). The exclusion criteria were: no CRP determination upon admission, patients with concomitant gallstones, no radiologic signs consistent with cholecystitis, or other histologic diagnoses (adenocarcinoma of the gallbladder).
In relation to medical progression, the patients were divided into 2 groups: 1) patients that required initial urgent cholecystectomy or surgical intervention for little or no response to conservative medical treatment (absolute diet, fluid therapy, and antibiotic therapy) and 2) patients that had a good response to conservative medical treatment, with acute episode resolution, and then deferred elective cholecystectomy. The variables included were age (years), sex, gallbladder wall thickness (mm), leukocytes (103/ul), bilirubin (mg/dl), GOT (IU/l), GPT (IU/l), CRP (mg/dl), type of surgery (urgent or deferred), and gallbladder histology.
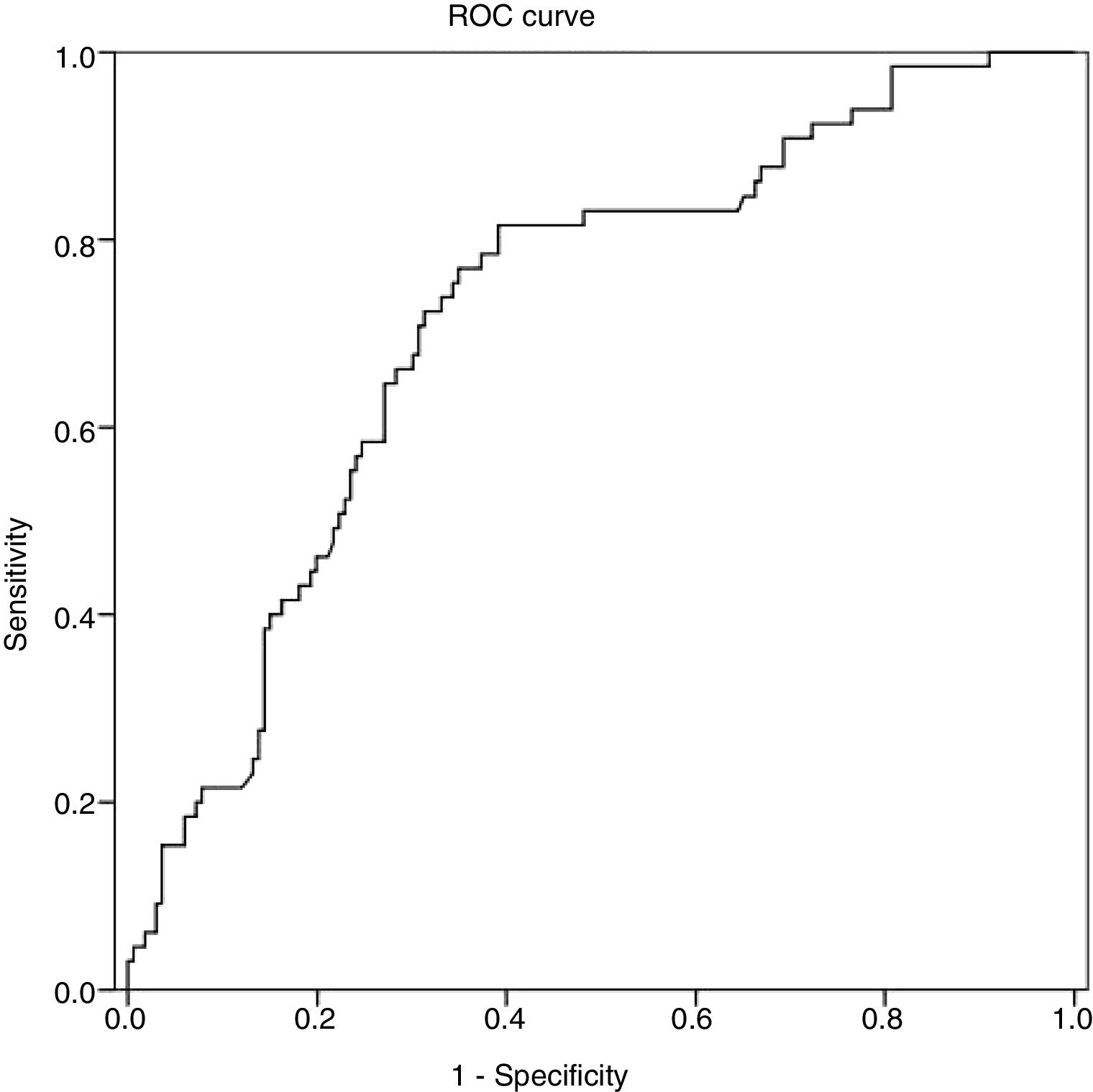
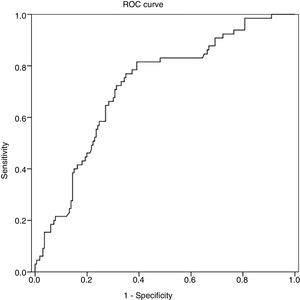
The statistical analysis was carried out using the SPSS v. 19 program. In the descriptive analysis, mean and standard deviation were employed for the quantitative variables and the categorical variables were described through absolute and relative frequencies. Normality was analyzed using the Kolmogorov-Smirnov test, which showed that the quantitative variables did not have a normal distribution. Thus, nonparametric contrasts were employed. The Spearman coefficient (rho) was used to analyze the correlation between the quantitative variables (correlation of the laboratory values and the radiologic values). The Kruskal-Wallis test was employed for the mean comparison contrasts (laboratory values and radiologic values in relation to gallbladder histology). Comparisons with paired variables were carried out with the Mann-Whitney U test. Successive step logistic regression was performed to analyze the joint relation of each qualitative variable of interest to the set of quantitative variables, including age and sex. To determine the prognostic capacity of CRP to detect gangrenous cholecystitis, ROC curves were developed, describing the area under the curve (AUC) with its corresponding 95% CI. The best cutoff points were determined through the Youden index, presenting the diagnostic test indicators: sensitivity and specificity. A significance level of 5% (p < 0.05) was selected in all the contrasts.
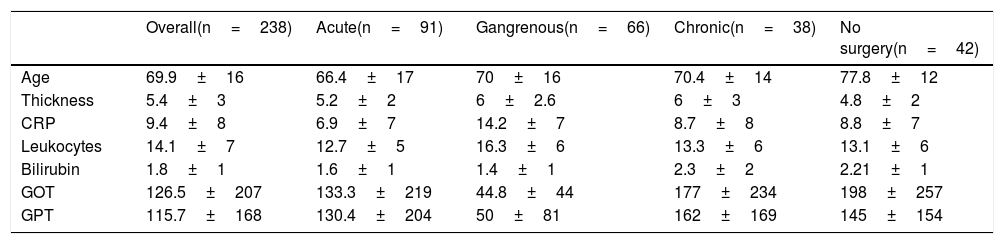
ResultsA total of 238 patients (♂ 54.6%, ♀ 45.4%) were analyzed that met the inclusion criteria. The values of the quantitative variables are shown in Table 1 (mean±standard deviation). Urgent surgery was performed on 158 patients (66.4%), whereas the remaining 80 patients (33.6%) were released from the hospital, following conservative treatment. Deferred surgery was later performed on 38 of those patients. Forty-two patients did not undergo deferred surgery, either because they had an associated comorbidity that required a hospital center offering more complex treatment or because the patient refused it. All of those patients were released to their homes with dietary recommendations.
Quantitative variables.
| Overall(n=238) | Acute(n=91) | Gangrenous(n=66) | Chronic(n=38) | No surgery(n=42) | |
|---|---|---|---|---|---|
| Age | 69.9±16 | 66.4±17 | 70±16 | 70.4±14 | 77.8±12 |
| Thickness | 5.4±3 | 5.2±2 | 6±2.6 | 6±3 | 4.8±2 |
| CRP | 9.4±8 | 6.9±7 | 14.2±7 | 8.7±8 | 8.8±7 |
| Leukocytes | 14.1±7 | 12.7±5 | 16.3±6 | 13.3±6 | 13.1±6 |
| Bilirubin | 1.8±1 | 1.6±1 | 1.4±1 | 2.3±2 | 2.21±1 |
| GOT | 126.5±207 | 133.3±219 | 44.8±44 | 177±234 | 198±257 |
| GPT | 115.7±168 | 130.4±204 | 50±81 | 162±169 | 145±154 |
The gallbladder histology of the patients that underwent urgent surgery was: acute cholecystitis in 38.2% of the patients (n=90) and gangrenous cholecystitis in 27.7% (n=66). In all the patients that underwent deferred procedures, the anatomopathologic result was chronic cholecystitis.
In the correlation analysis of the quantitative variables, statistically significant relations were observed between age and CRP values (p=0.013), gallbladder wall thickness and CRP values (p <0.001), gallbladder wall thickness and leukocyte levels (p=0.001), and CRP values and leukocyte levels (p <0.001).
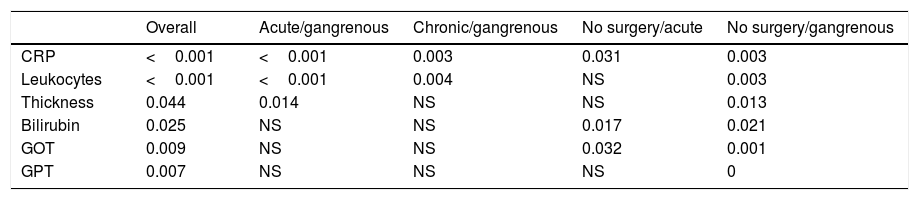
With respect to gallbladder histology, statistically significant correlations were observed in relation to CRP levels (p <0.001), leukocytes (p <0.001), gallbladder wall thickness (p=0.044), bilirubin (p=0.025), GOT (p=0.009), and GPT (p=0.007). The comparisons of paired variables with gallbladder histology showed significant differences in the means of acute cholecystitis in the presence of gangrenous cholecystitis for CRP (p <0.001), leukocytes (p <0.001), and gallbladder wall thickness (p=0.014). Likewise, significance was reached in the contrasts with respect to gallbladder histology (chronic cholecystitis in the presence of gangrenous cholecystitis) for CRP (p=0.003) and leukocytes (p=0.004). In the contrast between unoperated cholecystitis and acute cholecystitis, there was statistical significance for CRP (p=0.031), bilirubin (p=0.017), and GOT (p=0.032). In the contrast between unoperated cholecystitis and gangrenous cholecystitis, there was statistical significance for CRP (p=0.003), leukocytes (p=0.003), gallbladder wall thickness (p=0.013), bilirubin (p=0.021), GOT (p=0.001), and GPT (p=0.002) (Table 2).
p values obtained in the contrasts of the mean comparisons.
| Overall | Acute/gangrenous | Chronic/gangrenous | No surgery/acute | No surgery/gangrenous | |
|---|---|---|---|---|---|
| CRP | <0.001 | <0.001 | 0.003 | 0.031 | 0.003 |
| Leukocytes | <0.001 | <0.001 | 0.004 | NS | 0.003 |
| Thickness | 0.044 | 0.014 | NS | NS | 0.013 |
| Bilirubin | 0.025 | NS | NS | 0.017 | 0.021 |
| GOT | 0.009 | NS | NS | 0.032 | 0.001 |
| GPT | 0.007 | NS | NS | NS | 0 |
In the multivariate analysis, the gallbladder histologic grade was the dependent variable, and gangrenous cholecystitis was the reference category because it was the more severe. In the logistic regression analysis, the odds ratio of gangrenous cholecystitis in the presence of acute cholecystitis was calculated for CRP and produced an OR of 1.088 and 95% CI of 1.031-1.121 and for each unit of increase in CRP, the risk for gangrenous cholecystitis increased 8.8%. Likewise, there was statistical significance in the leukocyte values (p=0.017, OR=0.921, 95% CI: 0.861-0.985). Therefore, an increase in leukocyte levels increased the risk for gangrenous cholecystitis by 8.5%. In the logistic regression analysis, in the comparison of gangrenous cholecystitis with unoperated patients after conservative treatment, leukocyte values were statistically significant (p=0.021, OR=1.085, 95% CI: 1.021-1.152). In contrast, CRP showed a trend toward significance (p=0.055, OR=0.944, 95% CI: 0.889-1.001).
ROC curves were calculated to establish a relation between CRP values and gallbladder histology. From the AUC of the ROC curves for CRP, the cutoff points were calculated for predicting gangrenous cholecystitis. That analysis was statistically significant (p <0.01), with an AUC of 0.72 with a 95% CI (0.648-0.719). The resulting CRP values were 10.73mg/dl as the appropriate cutoff point, sensitivity of 70.8%, and specificity of 69.3% (fig. 1).
Discussion and conclusionsApproximately 10-15% of adults in industrialized countries present with gallstones and 20% will develop clinical symptoms related to them. Pain is the primary indication for surgery,2 and it is sometimes difficult to differentiate between biliary colic and acute cholecystitis. The most appropriate time to perform cholecystectomy in patients with acute cholecystitis is currently a subject of debate: early surgery can be performed within the first 72h of symptom onset, but it is also safe to provide conservative treatment and deferred surgery. The decision will depend on the conditions of the patient, surgical experience, and hospital infrastructure.4,5
Prospective and randomized studies have been conducted that show the benefits of early cholecystectomy within the first 24h, compared with elective surgery, in terms of hospital stay and costs.6–8 That was especially demonstrated in the study by Gutt et al., in which patients with an American Society of Anesthesiologists (ASA) classification of IV and V, septic shock, or perforation/abscess of the gallbladder were excluded from the analysis.6 Urgent surgery, even 3 days after symptom onset, has recently been shown to result in less morbidity, shorter hospital stay, and lower cost, with similar figures in relation to postoperative complications.9 In contrast, studies have also shown early cholecystectomy, as definitive treatment, to have a higher number of intraoperative and postoperative complications, as well as a higher rate of conversion to laparotomy 4,7 and a greater risk for hospital readmission due to symptom relapse.8
Leukocytosis, older age, diabetes, or late hospital admission, among others, have been established as poor prognosis factors for acute cholecystitis.3 Despite the fact that the recommendations of several studies support early cholecystectomy for the treatment of acute cholecystitis,6–10 surgery cannot always be performed within the first 24h, or even within the first few days due to: delayed consultation in the emergency service, abdominal pain screening by other specialists, or the absence of imaging studies when symptoms are unclear or laboratory tests are mildly altered. Those situations can result in late surgical consultation, enabling the gallbladder histology to progress to a classification of grade II cholecystitis, which is associated with greater surgical difficulty.3
In those late situations, more criteria are needed to safely indicate urgent surgery. Preoperative risk scales have been developed for the purpose of individualizing treatment and discerning patients with complicated cholecystitis (grade II and grade III), in which gallbladder wall thickness, leukocytosis, and CRP levels are significantly related, not only with the risk for surgical conversion, but also with the different levels of preoperative severity.11,12
As shown in other studies,13 our analysis resulted in statistically significant relations between gallbladder wall thickness and CRP values (p <0.001), gallbladder wall thickness and leukocyte levels (p=0.001), and CRP values and leukocyte levels (p <0.001). And in accordance with reports by other authors, gallbladder wall thickness greater than 4.5mm was associated with a higher probability of gangrenous cholecystitis.11–14 Likewise, in the comparisons of the paired variables with respect to gallbladder histology, there were significant differences between the means of acute cholecystitis in the presence of gangrenous cholecystitis for CRP (p <0.001), leukocytes (p <0.001), and gallbladder wall thickness (p=0.014).
In the logistic regression analysis, upon comparing gangrenous cholecystitis with acute cholecystitis, there was an 8.8% increase in risk for gangrenous cholecystitis with each CRP unit increase. There was also an 8.5% increased risk for gangrenous cholecystitis when there was an increase in leukocyte levels. Studies have reported that there is 100% sensitivity and 88% specificity in the diagnosis of gangrenous cholecystitis when the CRP value is 20mg/dl.13 In our study, sensitivity was 70.8% and specificity was 69.3% with a CRP value of 10.73mg/dl, in accordance with the theory that CRP has a higher discriminatory power in the diagnosis of severe acute cholecystitis.15
The main limitation of the present study was that the results were based on a retrospective study, and thus must be confirmed by prospective studies. Nevertheless, we believe that our combined results are a useful tool in the preoperative differentiation of the stage of progression of acute cholecystitis, albeit with the limitations inherent in a retrospective study. Definitive validation requires prospective studies with a larger number of patients.
In conclusion, in patients diagnosed with acute calculous cholecystitis, the combination of elevated figures of CRP, gallbladder wall thickness, and leukocytes correlated with more unfavorable clinical states and gallbladder histology, resulting in a greater need for urgent surgical treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Menéndez-Sánchez P, León-Salinas C, Amo-Salas M, et al. Asociación de parámetros analíticos y radiológicos en el diagnóstico de la colecistitis aguda. Revista de Gastroenterología de México. 2019;84:449–454.