Due to its different clinical manifestations, gastroesophageal reflux disease (GERD) requires diverse diagnostic and therapeutic interventions. The aim of the study was to evaluate the degree of agreement among Latin American specialists, with respect to the management of GERD.
Materials and methodsA cross-sectional study was conducted through a survey with 42 statements (22 related to diagnosis and 20 to treatment) applied to 56 specialists from Latin America. There were 4 possible statement responses: in complete agreement, in partial agreement, in partial disagreement, and in complete disagreement. Reproducibility, level of agreement, and concordance were measured through the Kappa statistic.
ResultsThe response rate was 81% (47/56). General concordance was low, given that there was complete concordance in only 12 statements (28.6%). There was partial concordance in 22 statements (52.4%) and no concordance in 8 (19%). The following themes had the most disagreement: the performance of endoscopy before beginning treatment, the use of proton pump inhibitors (PPIs) in patients with extraesophageal symptoms and with no typical symptoms, and the combined use of PPIs and prokinetics.
ConclusionsIn the present study, we found that there was agreement among the Latin American specialists for the diagnosis and management of GERD in less than one-third of the recommendations considered standard. The low concordance could be related to the fact that the availability of diagnostic tools and medications, as well as the prevalence of GERD phenotypes, is different in each country.
Debido a sus diferentes manifestaciones clínicas, la enfermedad por reflujo gastroesofágico (ERGE) requiere de diversas intervenciones diagnósticas y terapéuticas. El objetivo del estudio fue evaluar el grado de acuerdo entre especialistas de Latinoamérica con respecto al manejo de la ERGE.
Material y MétodosSe realizó un estudio transversal mediante la aplicación de un cuestionario con 42 enunciados (22 respecto a diagnóstico y 20 al tratamiento) a 56 médicos especialistas en Latinoamérica. Los enunciados se contestaron de acuerdo con 4 posibles respuestas: totalmente de acuerdo, parcialmente de acuerdo, parcialmente en desacuerdo y totalmente en desacuerdo. Se evalúo la reproducibilidad, el grado de acuerdo y concordancia mediante el índice de Kappa.
ResultadosLa tasa de respuesta fue del 81% (47/56). La concordancia en general fue baja, ya que en sólo 12 enunciados (28.6%) se obtuvo un acuerdo completo. En 22 enunciados el acuerdo fue parcial (52.4%) y en 8 no hubo acuerdo (19%). Los mayores desacuerdos fueron en los siguientes temas: realizar endoscopia antes de comenzar el tratamiento, uso de inhibidor de bomba de protones (IBP) en pacientes con síntomas extraesofágicos y sin síntomas típicos, uso combinado de IBP y procinéticos.
ConclusionesEn este estudio encontramos que existe acuerdo entre médicos especialistas latinoamericanos para el diagnóstico y manejo de la ERGE en menos de una tercera parte de las recomendaciones consideradas como estándares. La baja concordancia puede estar relacionada con que la disponibilidad de herramientas diagnósticas, medicamentos y prevalencias de los fenotipos de la ERGE en cada país son diferentes.
Gastroesophageal reflux disease (GERD) is one of the first reasons patients consult a primary care physician or gastroenterologist, worldwide. GERD is currently recognized as a very heterogeneous entity, obliging treating physicians to employ different diagnostic and therapeutic approaches. In an effort to provide a homogeneous approach, different international guidelines for the management of GERD have been developed1–5. Importantly, the majority of those guidelines are designed for patients from Europe, the United States, and Canada, and the sociocultural factors regarding GERD, such as mealtimes, diet, and associated comorbidities, are different in every country. Even though there are Latin American guidelines on the management of GERD that have come out of Mexico, Central America, and the Caribbean6,7, the heterogeneity in the region, with respect to habits and customs, as well as availability of resources and diagnostic tests, makes the applicability of said guidelines quite variable.
In addition, many gastroenterologists commonly adopt measures in their clinical practice based on their personal experience acquired over the course of treating many patients with GERD, and do not follow the guidelines or established recommendations.
The aim of the present study was to determine the degree of concordance (agreement or disagreement) among a selected group of specialists from Latin America on a series of diagnostic and therapeutic postulates, in accordance with their personal management of patients with GERD.
Materials and methodsStudy design and population analyzedA descriptive, cross-sectional study was conducted, in which 56 gastroenterologists from Latin America, belonging to the Sociedad Latinoamericana de Neurogastroenterología (SLNG), were invited to answer a survey, within the time frame of May 15 and June 30, 2020, that evaluated how they individually carried out the diagnosis and treatment of GERD. A personalized email invitation was sent to invitees possessing the following characteristics: a) theoretic and practical experience in the management of patients with GERD (degrees, research, published articles, position, experience, and awards, among others), b) availability and motivation to participate, and c) employment in services (public or private), in which patients with GERD are routinely treated.
MethodologyWithin the time frame of April and May, 2020, five representatives (LS, JT, JMRT, MAV, MS) of the working group, all of them members of the SLNG, designed a survey, taking into account the main international guidelines, the availability of resources in Latin America, and points of debate in clinical practice1–5. In a first round, all the participants were asked to formulate statements, using international guidelines as references 2–4, 6–7, that in their judgement and experience could represent the most common practices in the management of GERD. The resulting 37 statements were reviewed by two of the experts, and if there were discrepancies or confusion, a third expert aided in their resolution. Proceeding in that manner, the final survey consisted of 42 statements, 19 of which were related to diagnosis and 23 to treatment (Tables 1 and 2). The topics covered in the statements were:
- •
Initial course of action in patients with typical symptoms of GERD and good progression (statements 1–5).
- •
Conduct in patients with extraesophageal symptoms (statements 9, 10, 11, 13, 14).
- •
Conduct regarding refractoriness to proton pump inhibitor (PPI) therapy (statements 6, 8, 12).
- •
Use of manometry, pH study, and pH-impedance monitoring (statements 5, 7, 12, 15, 19).
- •
Importance given to diet and overweight (statements 24 and 25).
- •
Prokinetic use (statements 26 and 27).
- •
Alginate use (statement 28).
- •
Conduct regarding the diagnosis of reflux hypersensitivity (statements 29, 30, 31, 40, and 41).
- •
Conduct regarding the diagnosis of functional heartburn (statements 32–41).
- •
Conduct regarding Helicobacter pylori (H. pylori) eradication (statement 42).
Response percentage for each of the 19 statements regarding the diagnosis of GERD.
| Statements | In complete agreement | In partial agreement | In partial disagreement | In complete disagreement |
|---|---|---|---|---|
| 1) In patients with typical symptoms, no alarm signs or symptoms, and good PPI response, I never order upper gastrointestinal endoscopy, esophageal manometry, or reflux monitoring, regardless of GERD duration | 11 (24.4) | 19 (42.2) * | 8 (17.8) | 7(15.6) |
| 2) For all patients with typical symptoms of chronic GERD (more than 6 months) and no alarm signs or symptoms, I order upper gastrointestinal endoscopy (UGIE), before starting treatment | 10 (22.7) | 17 (38.6)* | 10(22.7) | 7 (15.9) |
| 3) In patients with a history of GERD and no alarm signs or symptoms, I indicate recent UGIE if the disease has a duration of more than 5 years | 25 (54.3)* | 8 (17.4) | 7 (15.2) | 6 (13.1) |
| 4) For all patients with typical chronic GERD symptoms and good treatment response, if a UGIE has been performed, I take biopsies, even if there are no endoscopic signs. | 3 (6.5) | 11 (24.4) | 9 (20) | 22 (48.9)* |
| 5) In patients with typical symptoms for more than 6 months, I always order reflux monitoring, preceded by esophageal manometry, regardless of response to PPIs | 1(2.2) | 5(11.1) | 15(33.3) | 24(53.3)* |
| 6) In patients with typical reflux symptoms and a lack of response to a standard-dose PPI, my first step is to evaluate if the medication administration time and dose are correct | 43 (93.5)* | 3(6.5)* | 0 | 0 |
| 7) In patients with typical symptoms and a lack of response to PPIs, my next step is to order pH study or pH impedance. | 15(32.6) | 25(54.3)* | 5(10.9) | 1(2.2) |
| 8) In patients with typical symptoms and a lack of response to PPIs, my next step is to order a UGIE (adding biopsies if there are no signs of GERD, to rule out EoE) | 32 (69.6)* | 10(21.7) | 1(2.2) | 3 (6.5) |
| 9) In patients with extraesophageal symptoms (cough, dysphony) and no typical symptoms, the therapeutic double-dose PPI trial is my first choice | 11 (23.9) | 16 (34.8)* | 7 (15.2) | 12 (26) |
| 10) In patients with extraesophageal symptoms, no typical symptoms, and no previous history of GER, referral to an ORL is my first choice | 23 (10.9)* | 12 (26.1) | 6 (13) | 5(10.9) |
| 11) In patients with ENT symptoms, no typical symptoms, and no history of GER, a pH study or pH impedance monitoring with no PPI is my first choice | 16 (34.8)* | 15 (32.6) | 7 (15.2) | 8 (17.4) |
| 12) In patients with a history of GERD (UGIE and/or monitoring), typical symptoms, and a lack of response to PPIs, I perform pH impedance under medication | 35 (76.1)* | 4 (8.7) | 3 (6.5) | 4 (8.7) |
| 13) In patients with extraesophageal symptoms and typical symptoms or a prior history of GERD, UGIE is the first-choice diagnostic test | 21 (45.7)* | 14 (30.4) | 5 (10.9) | 6 (13) |
| 14) In patients with extraesophageal symptoms and typical symptoms or a prior history of GERD, I order a reflux monitoring study (pH or pH impedance) as a first measure | 12 (26.1) | 15 (32.6)* | 7 (15.2) | 12 (26.1) |
| 15) Esophageal pH probe positioning should always be guided by esophageal manometry | 39 (84.8)* | 5 (10.9) | 1 (2.2) | 1 (2.2) |
| 16) Baseline impedance and the PSPW index are useful parameters for supporting the diagnosis of GERD | 36 (78.3)* | 7 (15.2) | 3 (6.5) | 0 |
| 17) Symptom correlation indexes, such as the symptom index and the symptom association probability, define phenotypes and therapeutic conducts | 37 (80.4)* | 6 (13) | 3 (6.5) | 0 |
| 18) Esophageal exposure to acid (%pH < 4) is a useful parameter for diagnosing GERD | 38 (82.6)* | 6 (13) | 1 (2.2) | 1 (2.2) |
| 19) The presence of weakly alkaline reflux is useful because it modifies my therapeutic conduct | 13 (28.3) | 19 (41.3)* | 12 (26.1) | 2 (4.3) |
ENT: ear, nose, and throat; EoE: eosinophilic esophagitis; GER: gastroesophageal reflux; GERD: gastroesophageal reflux disease; ORL: otorhinolaryngologist; PPI: proton pump inhibitor; PSPW: post-swallow peristaltic wave; UGIE: upper gastrointestinal endoscopy.
Results expressed in n (%). The asterisk signals the category that received the majority of responses.
Response percentage for each of the 23 statements regarding the treatment of GERD.
| Statements | In complete agreement | In partial agreement | In partial disagreement | In complete disagreement |
|---|---|---|---|---|
| 20) In patients with typical symptoms, lack of response to a standard-dose PPI is due to nonadherence and inadequate administration time of PPI, in relation to meals | 9 (19.6) | 29 (63)* | 7(15.2) | 1(2.2) |
| 21) In patients with typical symptoms but a lack of response to a standard-dose PPI, after optimizing the medication, the next step is to double the dose (before breakfast and before dinner) | 34 (73.9)* | 9 (19.6) | 2 (4.3) | 1(2.2) |
| 22) In patients with typical symptoms but a lack of response to a standard-dose PPI, after confirming correct medication application time and dose, the next step is to change the PPI | 14 (30.4) | 22 (47.8)* | 9 (19.6) | 1 (2.2) |
| 23) In patients with extraesophageal symptoms, with typical symptoms or a prior history of GERD, as a first measure, I begin treatment with a double-dose PPI | 26 (56.5)* | 18 (40) | 0 | 2(2.2) |
| 24) Dietary modifications (reducing fats, coffee, alcohol, carbonated drinks) have a poor impact on treatment of patients with GERD | 9 (19.6) | 22 (47.8)* | 10 (21.7) | 5 (10.9) |
| 25) Weight loss is one of the most effective lifestyle modifications for controlling GERD, in patients with overweight or obesity | 38 (82.6)* | 7 (15.2) | 0 | 1 (2.2) |
| 26) In the treatment of GERD with typical symptoms, the concomitant use of PPIs and prokinetics improves the therapeutic response | 1 (2.2) | 20 (43.5) | 12 (26.1) | 13 28.2) |
| 27) In the treatment of GERD with typical symptoms, I routinely add a prokinetic to the PPIs only if there is coexisting delayed gastric emptying | 31 (67.4)* | 14 (30.4) | 1 (2.2) | 0 |
| 28) In the treatment of GERD, adding alginates increases the therapeutic gain of PPIs | 15 (32.6) | 25 (54.3)* | 4 (8.7) | 2 (4.3) |
| 29) I avoid surgery in patients with reflux hypersensitivity | 32 (69.6)* | 11 (23.9) | 1 (2.2) | 2 (4.3) |
| 30) I do not use PPIs in patients with reflux hypersensitivity | 4 (8.7) | 7 (15.2) | 14 (30.4) | 21 (45.6)* |
| 31) I combine PPIs and neuromodulators in patients with reflux hypersensitivity | 34 (73.9)* | 11 (23.9) | 1 (2.2) | 0 |
| 32) In patients with functional heartburn, I avoid PPIs and use anxiolytics | 2 (4.3) | 12 (26.1) | 15 (32.6) | 17 (36.9)* |
| 33) In patients with functional heartburn, I avoid PPIs and use neuromodulators | 28 (60.9)* | 9 (19.6) | 4 (8.7) | 5 (10.9) |
| 34) In patients with functional heartburn, I combine PPIs and neuromodulators | 11 (23.9) | 9 (19.6) | 9 (19.6) | 17 (36.9)* |
| 35) In patients with functional heartburn, I combine antidepressants and anxiolytics | 5 (10.9) | 20 (43.5)* | 10 (21.7) | 11 (6.5) |
| 36) In patients with functional heartburn, I avoid PPIs and utilize psychologic therapies | 8 (17.4) | 25 (54.3)* | 10 (21.7) | 3 (6.5) |
| 37) In patients with functional heartburn, I avoid PPIs and utilize acupuncture over other therapies | 1 (2.2) | 4 (8.7) | 15 (32.6) | 26 (56.5)* |
| 38) In patients with functional heartburn, I avoid PPIs and utilize relaxation techniques/hypnotherapy | 4 (8.7) | 18 (40)* | 15 (32.6) | 9 (19.6) |
| 39) In patients with functional heartburn, I combine neuromodulators and psychotherapy | 19 (41.3)* | 16 (34.8) | 9 (19.6) | 2 (6.5) |
| 40) If neuromodulators are indicated for functional heartburn or reflux hypersensitivity, I prefer selective serotonin reuptake inhibitors and norepinephrine reuptake inhibitors | 10 (21.8) | 17 (36.9)* | 16 (34.78) | 3 (6.5) |
| 41) If neuromodulators are indicated for functional heartburn or reflux hypersensitivity, I prefer tricyclic antidepressants | 27 (58.7)* | 16 (31.8) | 3 (6.5) | 0 |
| 42) I consider that the eradication of Helicobacter pylori, present in the gastric mucosa, with no intestinal metaplasia, is important in the treatment of GERD | 0 | 4 (8.7) | 13 (28.3) | 29 (63)* |
GERD: gastroesophageal reflux disease; PPI: proton pump inhibitor.
Results expressed in n (%). The asterisk signals the category that received the majority of responses.
Each statement was answered by choosing only one response from the following 4 categories: in complete agreement, in partial agreement, in partial disagreement, and in complete disagreement. The survey was sent by email and the participants were asked to answer according to their actions in daily practice, regardless of the international guidelines. Once they answered the survey, the participants sent it back, and one week later, they received the same survey and answered it again, to evaluate its reproducibility.
Statistical analysisIn an effort to establish response consistency, the survey was replicated on two occasions and its reproducibility, between the first and second evaluation, was analyzed through the weighted Kappa index8, employing the Landis and Koch classification technique9 (kappa <0.4: poor concordance; 0.41–0.60: moderate concordance; 0.61–0.80: good concordance; and 0.81–1: very good concordance).
The degree of agreement among the survey participants was considered: a) complete concordance, when for each statement, two-thirds (>66.6%) of those surveyed agreed on one of the four response categories and b) partial concordance, when two-thirds (>66.6%) of those surveyed agreed on two of the response categories (in complete agreement, in partial agreement, in partial disagreement, or in complete disagreement).
Because 23 of the survey statements coincided with recommendations in some of the guidelines (from the United States, Europe, Mexico, Central America, and the Caribbean),2–4,6,7 considered reference patterns, we compared the survey responses with those guidelines. To establish the degree of concordance, we utilized the Landis and Koch classification9 previously described.
Ethical considerationsGiven the observational nature of the study, according to the legal exceptions, informed consent was not requested of the participating colleagues. Nevertheless, the survey was totally voluntary, the colleagues were informed of its aims, their authorization to participate, if feasible, in the publication of the results was requested, completely adhering to the norms of personal data protection. The authors declare that the present article contains no personal information that could identify the participants in the survey.
ResultsOverall responseThe response rate was 81% (47/56) and the participants per country were: 12 out of 15 (80%) in Argentina, 11 out of 13 in Mexico (84%), 6 out of 10 (60%) in Brazil, 4 out of 4 (100%) in Chile, 3 out of 3 (100%) in Colombia, 3 out of 3 (100%) in Ecuador, 3 out of 3 (100%) in Guatemala, 2 out of 2 (100%) in Peru, 2 out of 2 (100%) in Uruguay, and 1 out of 1 (100%) in Nicaragua. One applied survey was excluded due to incomplete information, resulting in a total of 1926 answers analyzed from 46 applied surveys. Tables 1 and 2 show the response percentage for each statement, according to the 4 categories.
ReproducibilityRegarding overall reproducibility, the weighted Kappa value for the four response categories was 0.71 (good), and it was 0.98 (very good) for only two categories (a: in complete agreement + in partial agreement and b: in partial disagreement + in complete disagreement).
Concordance with and adherence to the international guidelinesWhen concordance among the participants was evaluated, there was complete concordance in 12 (28.6%) of the statements, partial concordance in 22 (52.4%) of the statements, and neither complete nor partial concordance in 8 (19%) of the statements (Table 3). Table 4 shows the statements with much concordance and little concordance, respectively. When the degree of adherence to or conformity with the international guidelines was evaluated (23 statements, Table 5), agreement in 11 statements was very good (47.8%), in 5 (17.8%) was good, in 3 (13%) was moderate, and in 4 (17.4%) was poor.
Agreement percentage among the participants.
| Statement | Complete concordance/% | Partial concordance/% | Level of agreement |
|---|---|---|---|
| 1 | PA 42.2 | CA + PA 66.7 | Partial agreement |
| 2 | PA 36.9 | CA + PA 58.7 | No agreement |
| 3 | CA 55.5 | CA + PA 73.3 | Partial agreement |
| 4 | CD 48.8 | PD + CD 68.8 | Partial agreement |
| 5 | CD 53.3 | PD + CD 86.6 | Partial agreement |
| 6 | CA 93.5 | CA + PA 100 | Complete agreement |
| 7 | PA 54.3 | CA + PA 86.9 | Partial agreement |
| 8 | CA 69.6 | CA + PA 91.3 | Complete agreement |
| 9 | PA 34.8 | CA + PA 58.6 | No agreement |
| 10 | CA 50 | CA + PA 76.08 | Partial agreement |
| 11 | CA 34.8 | CA + PA 67.3 | Partial agreement |
| 12 | CA 76.1 | CA + PA 84.8 | Complete agreement |
| 13 | CA 46.5 | CA + PA 77.7 | Partial agreement |
| 14 | PA 32.6 | CA + PA 58.7 | No agreement |
| 15 | CA 84.8 | CA + PA 95.6 | Complete agreement |
| 16 | CA 78.2 | CA + PA 93.5 | Complete agreement |
| 17 | CA 80.4 | CA + PA 93.5 | Complete agreement |
| 18 | CA 82.6 | CA + PA 95.6 | Complete agreement |
| 19 | PA 41.3 | CA + PA 69.6 | Partial agreement |
| 20 | PA 63 | CA + PA 82.6 | Partial agreement |
| 21 | CA 73.9 | CA + PA 93.5 | Complete agreement |
| 22 | PA 47.8 | CA + PA 78.3 | Partial agreement |
| 23 | CA 56.5 | CA + PA 95.6 | Partial agreement |
| 24 | PA 47.8 | CA + PA 67.4 | Partial agreement |
| 25 | CA 82.6 | CA + PA 97.8 | Complete agreement |
| 26 | AP 43.5 | CA + PA 54.3 | No agreement |
| 27 | CA 67.3 | CA + PA 97.8 | Complete agreement |
| 28 | PA 54.3 | CA + PA 86.9 | Partial agreement |
| 29 | CA 69.5 | CA + PA 93.5 | Complete agreement |
| 30 | CD 45.6 | PD + CD 76.1 | Partial agreement |
| 31 | CA 73.9 | CA + PA 97.8 | Complete agreement |
| 32 | CD 36.9 | PD + CD 69.5 | Partial agreement |
| 33 | CA 60.8 | CA + PA 80.4 | Partial agreement |
| 34 | CD 36.9 | PD + CD 56.5 | No agreement |
| 35 | PA 43.5 | CA + PA 54.3 | No agreement |
| 36 | PA 54.3 | CA + PA 71.7 | Partial agreement |
| 37 | CD 56.5 | PD + CD 89.1 | Partial agreement |
| 38 | PD 39.1 | PD + CD 52.1 | No agreement |
| 39 | CA 41.3 | CA + PA 76.1 | Partial agreement |
| 40 | PA 41.3 | CA + PA 58.7 | No agreement |
| 41 | CA 58.6 | CA + PA 93.5 | Partial agreement |
| 42 | CD 63 | PD + CD 91.3 | Partial agreement |
CA: in complete agreement; CD: in complete disagreement; PA: in partial agreement; PD: in partial disagreement.
The resulting majority level of agreement for each of the statements (complete concordance) and the resulting percentage of the sum of the majority responses: in complete agreement (CA) + in partial agreement (PA) or in partial disagreement (PD) + in complete disagreement (CD) (partial concordance) are shown for each of the statements. Complete or partial agreement was considered when the percentage of responses was above 66.6% (2/3).
Statements with much concordance or little concordance among those surveyed.
| Much concordance | Little concordance |
|---|---|
| In patients with typical reflux symptoms and lack of response to a standard-dose PPI, my first step is to evaluate if the medication administration time and dose are correct | For all patients with typical symptoms of chronic GERD (more than 6 months) and no alarm signs or symptoms, I order upper gastrointestinal endoscopy (UGIE), before starting treatment |
| In patients with a history of GERD (UGIE and/or monitoring), typical symptoms, and lack of response to PPIs, I perform pH impedance under medication | In patients with extraesophageal symptoms (cough, dysphonia) and no typical symptoms, the therapeutic double-dose PPI trial is my first choice |
| Baseline impedance and the PSPW index are useful parameters for supporting the diagnosis of GERD | In patients with extraesophageal symptoms and typical symptoms or a prior history of GERD, I order a reflux monitoring study (pH or pH impedance) as a first measure |
| Symptom correlation indexes, such as the symptom index and the symptom association probability, define phenotypes and therapeutic conducts | In the treatment of GERD with typical symptoms, the concomitant use of PPIs and prokinetics improves the therapeutic response |
| Esophageal exposure to acid (%pH < 4) is a useful parameter for diagnosing GERD | In patients with functional heartburn, I combine PPIs and neuromodulators |
| In patients with typical symptoms but a lack of response to a standard-dose PPI, after optimizing the medication, the next step is to double the dose (before breakfast and before dinner) | In patients with functional heartburn, I combine antidepressants and anxiolytics |
| Weight loss is one of the most effective lifestyle modifications for controlling GERD, in patients with overweight and obesity | In patients with functional heartburn, I avoid PPIs and utilize relaxation techniques/hypnotherapy |
| In the treatment of GERD with typical symptoms, I routinely add a prokinetic to the PPIs only if there is coexisting delayed gastric emptying | If neuromodulators are indicated for functional heartburn or reflux hypersensitivity, I prefer selective serotonin reuptake inhibitors and norepinephrine reuptake inhibitors |
| Esophageal pH probe positioning should always be guided by esophageal manometry | |
| I avoid surgery in patients with reflux hypersensitivity | |
| I combine PPIs and neuromodulators in patients with reflux hypersensitivity |
Comparison of conducts in Latin America with those of the international guidelines (The United States, Europe, Mexico, and Central America)1–7.
| Statement | Guidelines | Survey | Kappa-95% CI | Agreement |
|---|---|---|---|---|
| 1 | In agreement | In agreement | 0.65/0.50−0.81 | Good |
| 2 | In disagreement | In agreement | 0.36/0.17−0.55 | Poor |
| 3 | In agreement | In agreement | 0.71/0.57−0.86 | Good |
| 4 | In disagreement | In disagreement | 0.67/0.52−0.82 | Good |
| 5 | In disagreement | In disagreement | 0.85/0.15−0.74 | Very good |
| 6 | In agreement | In agreement | 0.93/0.86−1 | Very good |
| 7 | In disagreement | In agreement | 0.13/0−0.30 | Poor |
| 8 | In agreement | In agreement | 0.91/0.82−0.99 | Very good |
| 9 | In disagreement | In agreement | 0.43/0.2−0.60 | Moderate |
| 10 | In agreement | In agreement | 0.76/0.62−0.89 | Good |
| 11 | In disagreement | In agreement | 0.32/0.13−0.52 | Poor |
| 12 | In agreement | In agreement | 0.85/00.74−0.96 | Very good |
| 13 | In disagreement | In agreement | 0.22/0.01−0.42 | Poor |
| 14 | In disagreement | In agreement | 0.43/0.20−0.60 | Moderate |
| 16 | In agreement | In agreement | 0.93/0.86−1 | Very good |
| 17 | In agreement | In agreement | 0.93/0.86−1 | Very good |
| 18 | In agreement | In agreement | 0.98/0.94−1 | Very good |
| 19 | In agreement | In agreement | 0.70/0.55−0.84 | Good |
| 20 | In agreement | In agreement | 0.85/0.74−0.96 | Very good |
| 21 | In agreement | In agreement | 0.93/0.86−1 | Very good |
| 23 | In agreement | In agreement | 0.95/0.89−1 | Very good |
| 25 | In agreement | In agreement | 0.98/0.94−1 | Very good |
| 26 | In disagreement | In agreement | 0.55/0.38−0.72 | Moderate |
In the present study, we showed that even though close to 70% of the Latin American specialists surveyed followed international recommendations, with respect to the diagnostic and therapeutic approach to GERD, there was concordance in less than one-third of them (28%). Given our survey results, the low concordance among the participants in the majority of the statements is most likely influenced by the place of work, personal experience with different diagnostic methods, the available resources, and of course, by each specialist’s professional experience, which does not necessarily coincide with recommendations of the international guidelines. In the majority of cases, the approach of the participants was based on published evidence or their expert opinion.
Making the appropriate diagnosis is essential for the management of GERD, given that an accurate diagnosis guides the treatment and has cost-benefit implications. The variability found in the responses to those corresponding statements was very heterogeneous and striking. Whereas only 22% of the participants completely agreed that no diagnostic test was required in patients with no alarm symptoms and good response to treatment (statement 1), 69% responded that at least one endoscopy should be performed in nonresponders to treatment (statement 8). Regarding the approach variability, certainly the availability of and access to diagnostic tests varies throughout the continent10,11. Our results suggest that conducts cannot always be the same in all cases, and even though the guidelines provide orientation, they cannot always be uniformly applied to all patients or all countries.
Extraesophageal manifestations are one of the most controversial areas in GERD. According to the guidelines3 and published studies12–15, in patients with no symptoms or history of GERD, the causes that are unrelated to GERD (postnasal syndrome, allergies, allergic laryngitis, angiotensin-converting enzyme (ACE) inhibitor use, sinus disorders) must first be ruled out, and indicating PPIs or carrying out reflux monitoring should not be the first course of action.3 In the opinion of the specialists surveyed, the first step would be to begin with double-dose PPI (58.7%, agreement of 23.9%) or carry out reflux monitoring (67.4%, agreement of 34.8%), whereas only 37% (agreement of 11%) would refer patients to rule out causes unrelated to gastroesophageal reflux. Even though the initial approach varied, it should be underlined that 76% of the survey participants agreed that when symptoms of GERD persisted in patients with extraesophageal symptoms, they should be evaluated through pH study with impedance monitoring under treatment. That could reflect the fact that the majority of the participants surveyed follow the international recommendations or that they are a group of specialists with a high level of knowledge of how and when to utilize diagnostic tests, which is also supported by the fact that the statements related to the technical questions of pH-study with impedance monitoring (statements 15–18) had high concordance (above 75%).
Likewise, with respect to treatment, there was heterogeneous variability among the survey participants. A high percentage (83%) were of the opinion that weight loss is one of the most effective lifestyle modifications for reducing symptoms of GERD,16 and very few (20%) did not consider dietary recommendations useful.
The lack of treatment response is currently 40% in patients that take a standard-dose PPI once a day. It is more frequent in patients with nonerosive reflux17,18, and is currently considered multifactorial19–25. In general, the responses of the survey participants coincided with the suggestions in the guidelines and articles3,18, that when there is a lack of response to treatment, correct medication administration should first be verified, and if adequate, the dose should be doubled (statement 21, agreement of 73%)3. Nevertheless, there was lower complete agreement (30%), with respect to changing the PPI. Again, those findings can be influenced by drug availability and cost, which vary in Latin America. The international guidelines recommend that prokinetics not be used in patients with GERD that have not undergone a diagnostic test and advise their indication only in the presence of gastroparesis3. However, in our study, 45.7% of the gastroenterologists stated that prokinetics improved the symptoms of gastroesophageal reflux when they were combined with a PPI, even though agreement was partial in 43.5%. Hypothetically, we believe that said conduct could be influenced by the wide availability of prokinetics in Latin America. Another course of action that is not supported in the guidelines, but was a frequent survey response (87%), was the combination of PPIs and alginates.
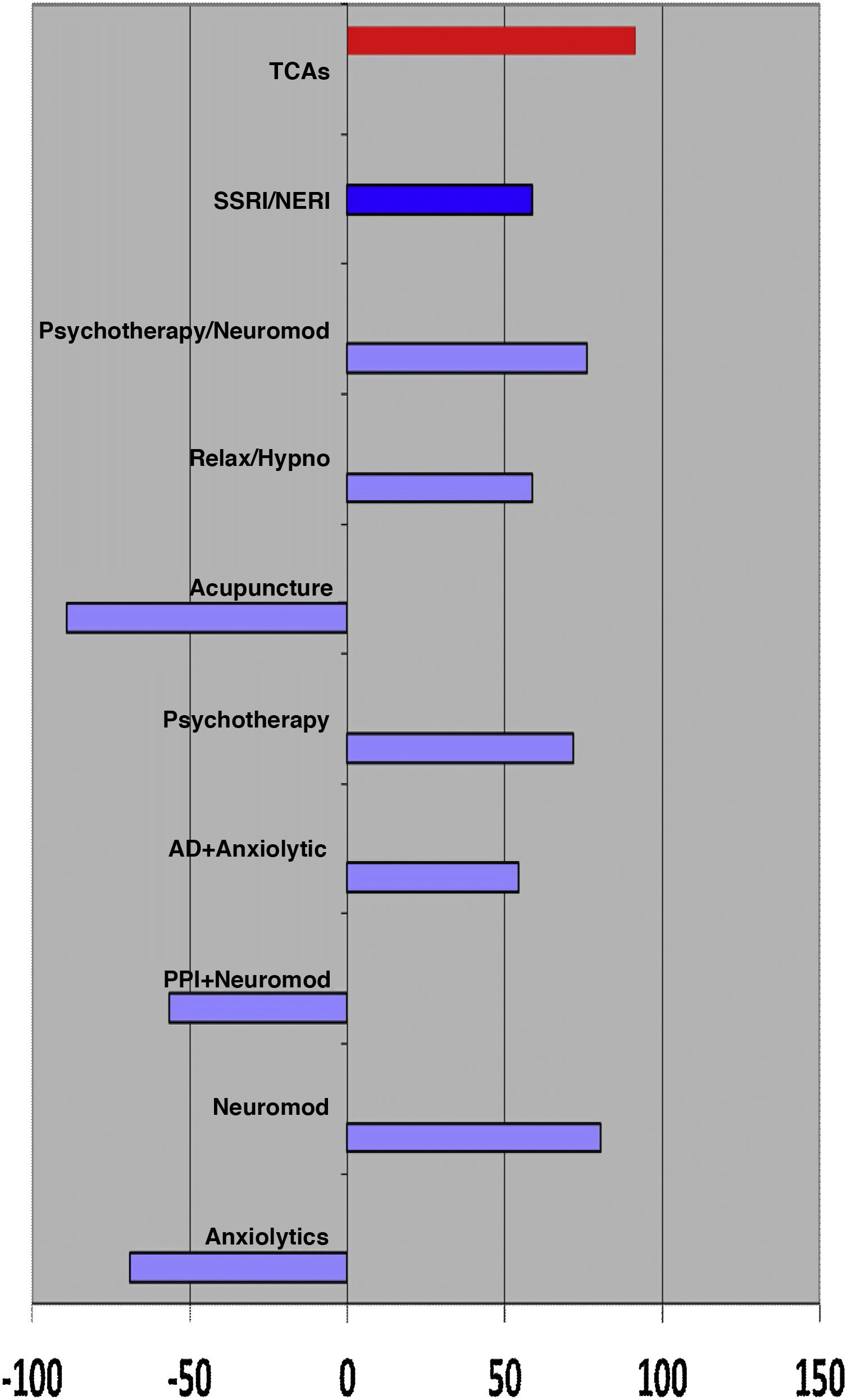
On the other hand, the majority of specialists surveyed agreed with the recommendations regarding the differentiation of GERD, esophageal hypersensitivity (EH), and functional heartburn (FH)26, reaffirming the fact that the survey participants were made up of specialists that continuously keep up-to-date on the topic. The majority of the participants (97.8%) were in agreement that adding neuromodulators (tricyclic antidepressants, selective serotonin reuptake inhibitors, etc.) to acid secretion inhibiting therapy was the best management for patients with EH, as recommended in the literature27,28. They also agreed about not using anxiolytics or PPIs in FH (80.4%), again choosing the use of neuromodulators (preferably tricyclic antidepressants, psychotherapy, and relaxation techniques and hypnotherapy) (Fig. 1).
At present, although some studies consider that the presence of H. pylori can have a beneficial or protective role in GERD29,30, others have shown the opposite31. The bacterium has even been associated with Barrett’s esophagus, as well as adenocarcinoma of the esophagus32. In the present survey, the gastroenterologists were asked if they considered H. pylori eradication useful in patients with GERD, and 91.3% answered in the negative (agreement of 63%).
Importantly, the primary aim of the present study was not to determine whether the approaches adopted by the specialists were the correct ones, but rather to know the “real world” manner of working of a selected group of gastroenterologists in Latin America. We also took into account the fact that in some cases, the international guidelines are based on scenarios that are not precisely the same as those in developing countries, which are the majority of Latin American countries.
Among the limitations of the present study was the survey design of statements with four possible response categories that could be perceived as unclear and produce doubts. That could possibly explain the poor agreement among the survey participants, indicating a marked dispersion in the responses. Twenty-three of the survey statements were based on international guidelines, whereas, although it could appear arbitrary, the authors of the survey statements agreed that the other 19 statements were conducts frequently seen in their clinical experience. An effort was made to represent all Latin American countries but not all survey invitations were accepted. In addition, whether the survey participants were all gastroenterologists, neurogastroenterologists, or surgeons, was not determined. Our study is not exempt from bias, specifically in the statements that are expressed subjectively that describe two conditional interventions (e.g., statements 36, 37, and 38). Other factors unrelated to the disease can also explain the different responses of the participants, such as the cost-effectiveness of endoscopy and functional studies in each country or region and the manner in which the physicians are paid (by private patients, determined by a healthcare system, as capitation, or as a fixed salary). Those considerations are also reflected in the observations in the World Gastroenterology Organisation (WGO) guidelines2 that differ from those in the American Gastroenterological Association (AGA) guidelines3.
The main strength of the present study is that it is a Latin American study that reflects reality in the management of a disease as complex as GERD. The majority of management guidelines on the disease come from the medical societies of developed countries, and so whether the same recommendations are applied by neurogastroenterologists in Latin America is not known. Even though our findings are important, their validation through similar studies conducted by associations and colleges involved in the management of GERD in Latin America would be very beneficial. Such further study would enable guidelines and/or consensuses to be developed that can be applied to the Latin American reality and said information could be conveyed through various strategies of continuing medical education.
ConclusionsThe present study revealed that the diagnostic and therapeutic approach to GERD in Latin America is highly variable and concordance between conducts is low. That poor agreement may be linked to the availability of diagnostic tools and medications, as well as to the different prevalence of the GERD phenotypes in each country.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestLuis Oscar Soifer, has been a consultant for AstraZeneca, Bayer, Bagó, Roemmers, and Novartis and has given talks for Biofarma, Novartis, Sanofi, and Domínguez.
José Tawil is a member of the advisory board of Takeda and has given talks for the Craveri, Temis Lostalo, and Eczane laboratories.
Jose María Remes Troche is a member of the advisory board of Takeda, Asofarma, and Biocodex and has given talks for Takeda, Asofarma, Medtronic, Carnot, and Alfasigma.
Miguel Ángel Valdovinos Díaz is a member of the advisory board of Takeda and has given talks for Takeda, Asofarma, Medtronic, Carnot, and Grünenthal.
Max Julio Schmulson is a research consultant for Alfasigma, a consultant for Gemelli Biotech, and gives talks for Takeda México.
The GERD Collaboration Group of the Sociedad Latinoamericana de Neurogastroenterologia: Soto JC, Sobrino S, Abreu AT, Coss-Adame E, Gomez Escudero O, Amieva Balmori M, Huerta F, Teramoto M (México), Hanna I, Coello Jaramillo R, Montalvo R (Ecuador), Rosas E, Vesco E, Monge V (Peru), Francisconi C, Bievig R, Prado de Moraes Filho J, Resende Neto J, Carvalho P, Bravim M (Brazil), Defilippi C, Monrroy H, Cisternas D, Madrid AM (Chile), Leguisamon AM, Ardila AF, Costa V, Hani A (Colombia), Cohen H, Dacoll C (Uruguay), Aguilar Paiz L, Garcia Martinez I, Jerez González L (Guatemala), Mejía M (Nicaragua), Solé L, Bustos Fernández LM, Ramos RM, Pascual A, Peralta DA, Alach J, Rodriguez S, Defagó MR, Arguero J, Guzmán JM, Ventura A, Salis G (Argentina), with the special collaboration of Sifrim D (Belgium)
Please cite this article as: Soifer L, Tawil J, Remes-Troche JM, Valdovinos MA, Schmulson M, grupo de colaboración de ERGE de la Sociedad Latinoamericana de Neurogastroenterología. Grado de acuerdo en el manejo de pacientes con enfermedad por reflujo gastroesofágico. Un estudio entre especialistas miembros de la Sociedad Latinoamericana de Neurogastroenterología (SLNG). Revista de Gastroenterología de México. 2022;87:420–431.