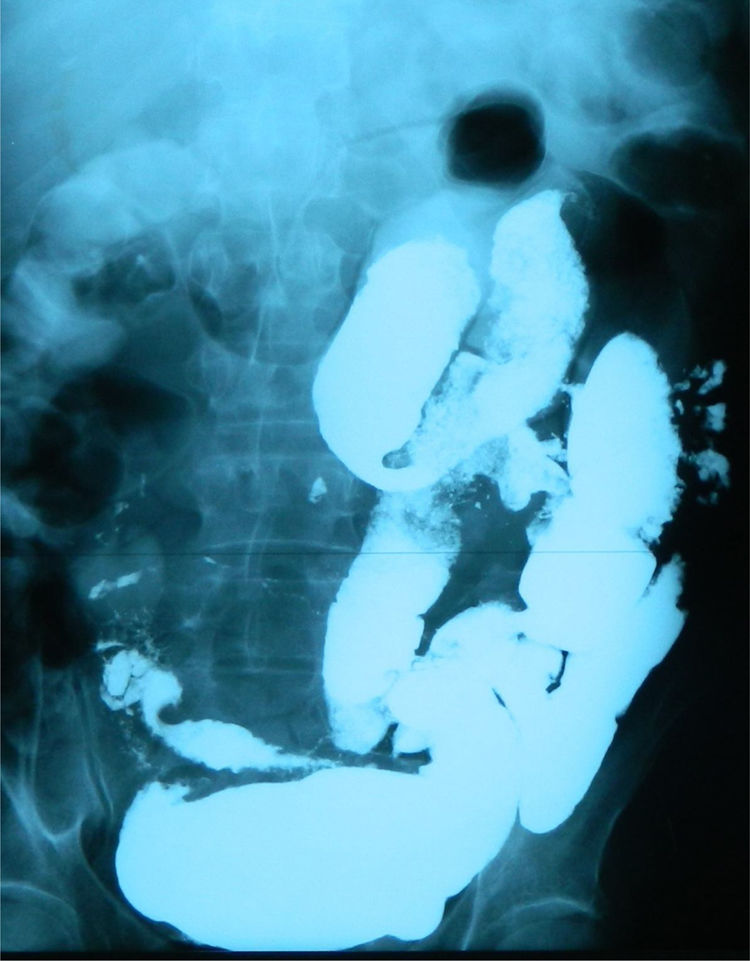
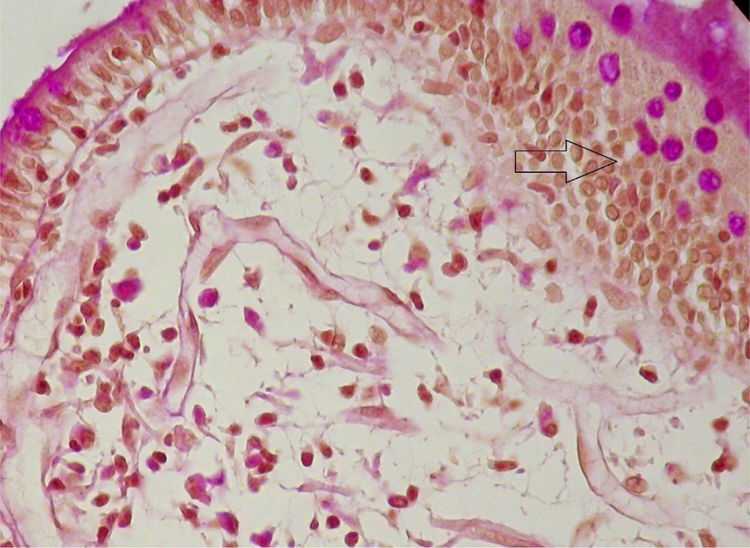
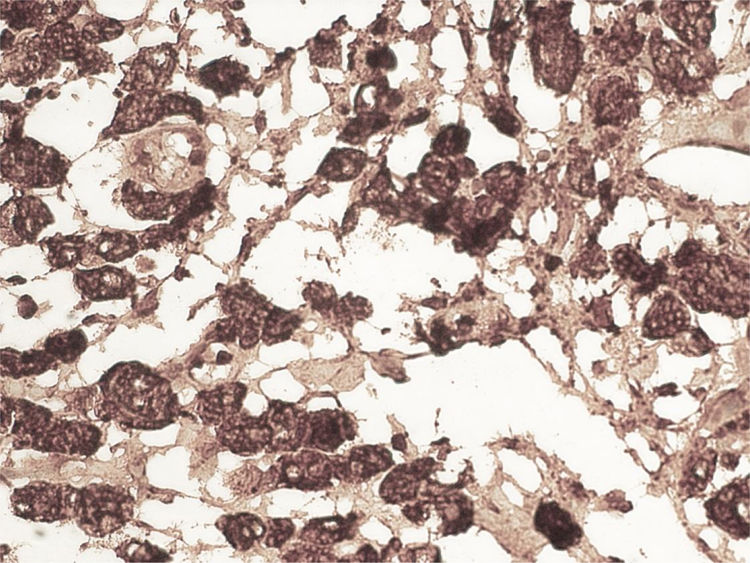
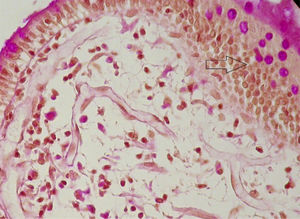
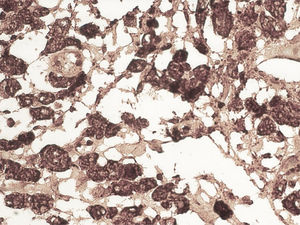
A 59-year-old man was admitted to the hospital, presenting with asthenia, morning nausea, lack of appetite, weight loss, diarrhea, lower limb paresthesia, and psychotic disorders with non-systematized delusions of persecution, hallucinations, and self-harm for the past 6 months. The patient had an unremarkable past medical history, and reduced adipose tissue was the only clinical observation. Biochemically, test results showed normocytic normochromic anemia, accelerated erythrocyte sedimentation rate (ESR), hepatic cytolysis and cholestasis syndrome, hypoalbuminemia, and hypergammaglobulinemia. He was tested for HIV 1 and 2 and the serum serotonin (5-hydroxytryptamine) level was determined. Gastrointestinal endoscopy identified an atrophied duodenal epithelium with a diffuse enanthem, which was biopsied (Fig. 1). An enteroclysis catheter was placed and showed moderate dilation of the enteral segments with flocculation of the barium suspension at the level of the ileum (Fig. 2). The duodenal biopsies revealed focal lymphangiectasias, with periodic acid-Schiff (PAS)-positive infiltrate in the lamina propria, suggesting Whipple’s disease (Fig. 3). At the same time, biopsies of the peri-duodenal adenopathy were taken that showed the presence of macrophages (Fig. 4). We made the following concomitant diagnoses: hepatic hemangiomas, nonalcoholic steatohepatitis, right renal cyst, aortic atheromatosis, hypomagnesemia, hypocalcemia, hypertriglyceridemia, and hyperuricemia. After treatment with ceftriaxone 2 g/day for 7 days, followed by sulfamethoxazole and trimethoprim 2 × 800/160 mg/day, progression was favorable. Whipple’s disease is a multiorgan infectious disease caused by the Gram positive commensal bacterium, Tropheryma whipplei, affecting middle-aged men,1 with the resulting immune system changes.2,3 Diagnosis generally is made showing the presence of PAS-positive macrophages with bacilli in the lamina propria of the small bowel or utilizing genetic techniques, such as PCR, for detecting bacterial DNA.4
No financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Saraci G. Enfoque diagnóstico de una condición rara: la enfermedad de Whipple. Revista de Gastroenterología de México. 2020;85:477–478.