A 31-year-old woman, whose only relevant past medical history was scoliosis, treated with meloxicam, carisoprodol, and dexamethasone for 15 years, was admitted to the emergency room due to 16 episodes of hematochezia in 24h, asthenia, adynamia, and generalized weakness. Upon admission, her vital signs were normal, except for tachycardia of 100 bpm. Physical examination revealed skin pallor, uncompromised cardiopulmonary function, and abdomen with no signs of peritoneal irritation. The rectal examination identified no active bleeding, hemorrhoids, or palpable tumor; remnants of blood were on the examination glove when exiting the rectum; and there was immediate capillary refill. Laboratory study results were hemoglobin 8.9g/dl, hematocrit 28.8%, mean erythrocyte volume 77.6fl, platelets 259103/μl, leukocytes 4.69103/μl, INR 1.02, creatinine 0.7mg/dl, sodium 143, potassium 4.2, and chloride 109.
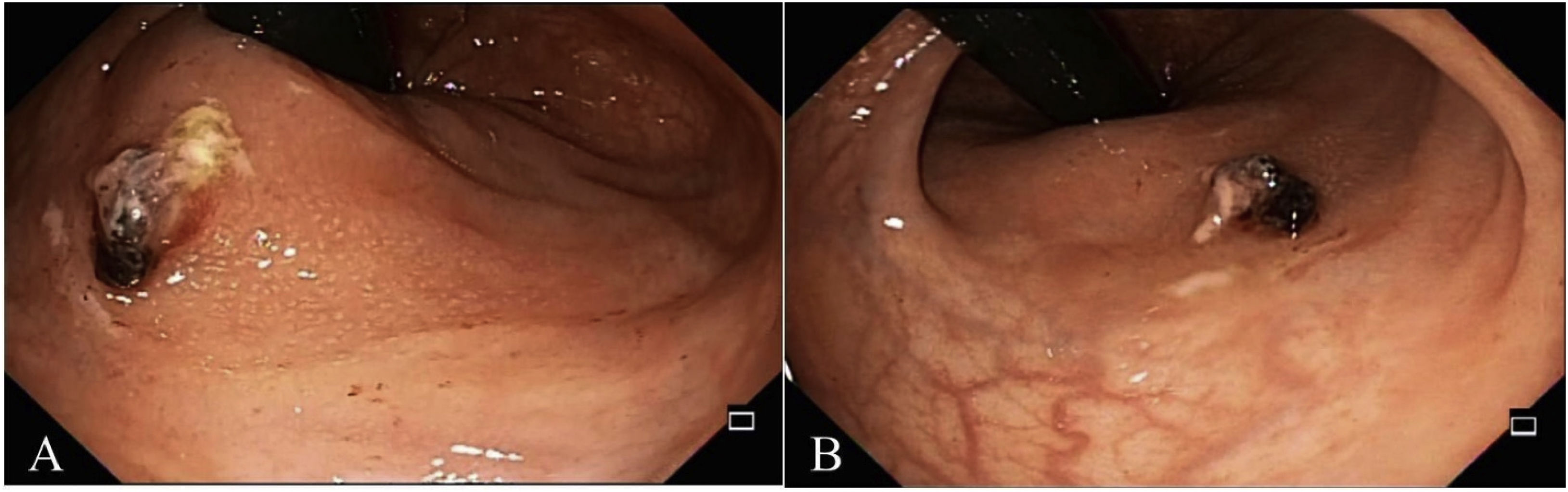
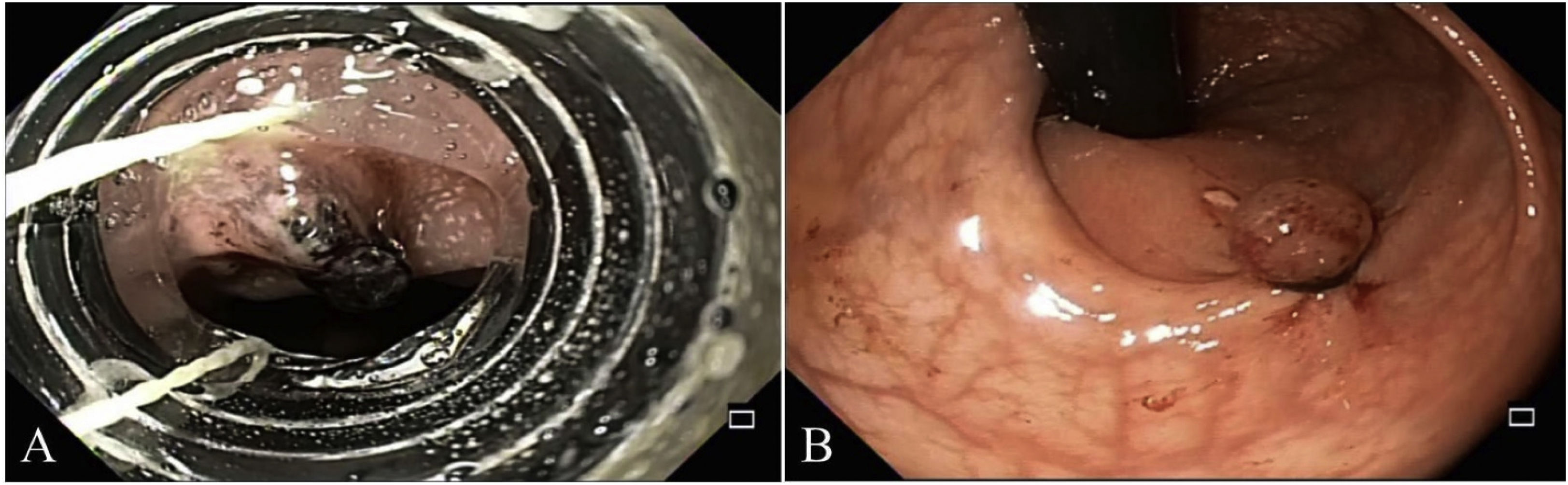
Colonoscopy revealed a protruding 4-5mm vascular lesion that was 5cm from the anal verge, in the region of the rectum, normal mucosa, and no ulcerations (Fig. 1A and B). No hemorrhoidal disease was viewed during retroflexion. The examination reached the transverse colon, showing no other alterations. Band ligation was applied on the Dieulafoy’s lesion with no complications (Fig. 2A and B). The day after the procedure, the patient’s progression was adequate, she was hemodynamically and clinically stable, and her vital signs were within normal limits. Upon physical examination, there were no remnants of blood on the examining glove when removed from the rectum after the digital rectal exam. The patient was discharged to her home with an open emergency room appointment in case of any alarm symptoms. The patient presented with no rebleeding at follow-up.
Dieulafoy’s lesion was first described by Gallard in 1884 and then defined by the French surgeon, Paul Georges Dieulafoy, in 1898, naming it “exulceratio simplex”.1 It is a vascular anomaly of the gastrointestinal tract that consists of the presence of a submucosal vessel, with an abnormally dilated diameter of up to 3mm that erodes into the mucosa, in the absence of a previous ulcer, causing a small defect in the wall, with fibrinoid necrosis at the base; the rest of the mucosa is intact.2
Dieulafoy’s lesion is a rare cause of gastrointestinal bleeding, with an incidence of up to 5%. Given its arterial nature, it can be life-threatening. In a Mexican case series, 50% of patients presented with hemodynamic instability.3,4
The etiology and pathophysiology of Dieulafoy’s lesion are not well understood. The most widely accepted theory is that an ischemic lesion caused by atrophy and a tear in the mucosa leads to disruption of the overlying epithelium, with the subsequent exposure of a submucosal vessel to the intestinal content that results in mechanical and chemical erosion, causing bleeding.5 A theory of spontaneous bleeding underlines the possibility of shear stress caused by compressive arterial pulsations that end in ischemia of the mucosa and subsequent erosion.5,6 Another theory suggests that arterial thrombosis is the cause of the ischemia and bleeding.7 Patient’s with Dieulafoy’s lesion tend to be asymptomatic before presenting with gastrointestinal bleeding.8 Rectal Dieulafoy’s lesion shares pathologic and macroscopic histologic peculiarities with lesions located at other segments of the gastrointestinal tract. However, the regional, anatomic, and functional differences between the upper and lower gastrointestinal segments can play a role in the origin of the lesion or the exacerbation of the existing lesion. Stercoral damage due to constipation, inspissated fecal matter, chronic immobilization, cancer, and senile degenerative changes in the vascular and submucosal beds can be mechanical inciting factors for the mechanisms of erosion that are behind bleeding rectal lesions.6 In addition, atrophy of the mucosa attributed to the senile changes may also contribute to that process.9 Regarding rectal Dieulafoy’s lesion, receptive anal intercourse can also be considered a potential pathogenic factor, especially in relatively young patients with no significant medical conditions.10
The clinical presentation is varied and can include iron deficiency anemia, rectorrhagia and/or hematochezia. Bleeding episodes are generally intermittent and self-limited but can progress to profuse bleeding that culminates in hypovolemic shock, with such cases reaching an 80% mortality rate.11–13 In one review, patients were reported to commonly present with massive and sudden rectal bleeding with bright red blood (47%), hematochezia (36%), nonpainful rectorrhagia (11%), and melena (4%). Among the other notable clinical characteristics were sudden hemodynamic involvement, lower abdominal pain, loss of consciousness, cerebrovascular accident, and iron-deficiency anemia.6
Patients with bleeding from a Dieulafoy’s lesion are usually men, at a male-to-female ratio of 2:1, between the fifth and sixth decades of life, and with comorbidities, such as hypertension, heart disease, kidney disease, or diabetes. Factors, such as alcohol abuse, smoking, nonsteroidal anti-inflammatory drug and anticoagulant use, and peptic acid disease, have been considered possible triggers, but any such associations have yet to be confirmed.4,5,8
Seventy percent of the cases are located in the lesser curvature of the stomach, but the lesion can present throughout the gastrointestinal tract.5,8 Dieulafoy’s lesion in the rectum corresponds to 2% of the reported cases.12,14
In the cases with no active bleeding, endoscopic evaluation can show the lesion to be a nipple-like protrusion, a polyp, or an exposed vessel, with no overlying ulceration or erosion.15,16 Nevertheless, aberrant arteries are predominantly visualized only during active bleeding. The lesion can also be covered by a blood clot, after a previous bleeding event.6 Endoscopic diagnosis is based on the presence of several factors: an arterial vessel that actively bleeds through normal surrounding mucosa; a fresh clot adhered to a tiny mucosal defect or normal-appearing mucosa; or a vessel that protrudes from a tiny mucosal defect or normal-appearing mucosa, with or without active bleeding. However, endoscopic diagnosis tends to be difficult in a colorectal lesion, due to the limited visibility caused by massive bleeding or lack of bowel preparation, conditions under which angiography can be useful.3 The mean number of colonoscopies needed to detect rectal Dieulafoy’s lesion is 1.5±0.7.6
Up to 1990, surgical intervention was the cornerstone of treatment of Dieulafoy’s lesion and was associated with a mortality rate of up to 80%. Therapeutic endoscopy has evolved to become a safe, feasible, and efficacious modality, with a reported hemostatic success rate of 75 to 100%.17 Surgery has currently been replaced by endoscopic and angiographic techniques, utilizing therapies, such as epinephrine/norepinephrine injection, sclerotherapy, thermocoagulation, electrocautery, argon coagulation, or the application of bands or hemoclips. Hemostasis can be achieved through endoscopic treatment in 90% of cases.3,5
Thermocoagulation is associated with a greater risk for perforation due to the thinness of the colorectal wall, compared with the stomach, and so a mechanical method tends to be safer and more efficacious.5,14 For that reason, we chose band ligation in the management of our patient.
With respect to the different mechanical methods, a meta-analysis of 5 studies found no statistically significant difference in the primary hemostasis success rate and bleeding recurrence rate between band ligation and hemoclip placement.18 Selective embolization is indicated when endoscopic treatment fails.12
Due to its rareness, there is no consensus on the optimal endoscopic hemostatic technique for rectal Dieulafoy’s lesion. The reports on thermocoagulation methods are mainly from the past century and few studies have been reported in recent years. Thus, the mechanical endoscopic techniques appear to be more feasible, and have been used in the majority of patients with rectal disease.19
Despite the undeniable benefits of endoscopic therapy, there is scant long-term follow-up information, in cases of rectal Dieulafoy’s lesion. In a review of the literature that identified 101 patients, 13 had recurrent bleeding. The patients that experienced rebleeding achieved hemostasis with repeat treatment. Therefore, it can be speculated that rectal Dieulafoy’s lesion has a relatively good prognosis and a low recurrence rate, assuming adequate treatment at the first stages of bleeding is carried out.6
Ethical considerationsAuthorization by the institutional ethics committee was not required, given that no patient anonymity norms were violated at any time. The authors declare that this article contains no personal information that could identify the patient.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Martínez-Ortiz CA, Alvarez-Sores ED, Lara-Orozco U, Murcio-Pérez E. Lesión de Dieulafoy en el recto: reporte de un caso. Rev Gastroenterol Méx. 2023;88:301–304.