La gammagrafía y la cola ngiorresonancia de hígado y vías biliares (CRMN) desplazaron la prueba de la sonda duodenal (PSD) en el estudio de ictericia colestásica por atresia de las vías biliares extrahepáticas (AVBE). Demostrar utilidad de la PSD asociada a ultrasonido de abdomen (USA), en el diagnóstico de AVBE. Cuatro casos con ictericia colestásica se sometieron a PSD y USA; uno de ellos, a CRMN. La PSD fue negativa para bilis en los 4; el USA no demostró vesícula, o la demostró pequeña o irregular, o detectó cordón fibroso; la CRMN mostró quiste de colédoco, pero no AVBE asociada; cirugía y patología documentaron AVBE en los 4. La PSD asociada a USA demuestra ausencia de bilis en el duodeno y anormalidad de la vesícula, respectivamente, lo que conduce a exploración quirúrgica en 24 a 48 h.
Liver and b iliary tree scintigraphy and magnetic resonance cholangiography (MRC) have taken the place of the duodenal tube test (DTT) in the study of cholestatic jaundice due to extrahepatic biliary atresia (EBA). The usefulness of DTT associated with abdominal ultrasound (AUS) in the diagnosis of EBA was demonstrated in 4 patients presenting with cholestatic jaundice that underwent DTT and AUS; one of them also had MRC. DTT was negative for bile in the 4 patients; AUS did not identify the gallbladder or showed it as small and irregular, or detected a fibrous cord; MRC identified a choledochal cyst but no associated EBA; surgery and pathology study documented EBA in all 4 patients. DTT associated with AUS demonstrated the absence of bile in the duodenum and gallbladder abnormality, respectively, leading to surgical exploration within 24 to 48 hours.
Introduction
Two female infants, 64 and 89 days old, and 2 male infants, 61 and 52 days old, were products of uncomplicated natural eutrophic births. They weighed between 3 and 3.7 Kg and developed jaundice at the first 2 weeks of life, along with hard, nodular hepatomegaly with a well-defined edge, splenomegaly, and abdominal distension. One of the patients had choluria from the first week of life. Duodenal tube test (DTT) and abdominal ultrasound (AUS) were done on all 4 patients and one had magnetic resonance cholangiography (MRC).
The mean age at the time of diagnosis with DTT was 73 days. None of the patients showed an interruption in growth velocity at the time of diagnosis. All 4 infants had generalized jaundice with a dark green hue, hard hepatomegaly with an irregular surface, and splenomegaly. Three of the patients presented with dark urine, one of them presented with choluria, and one with distension.
Direct bilirubin (DB) varied from 3.9 to 13.9 mg/dL, representing from 32.2 to 97.2% of the total. In the case 3 patient, MRC identified a type 1 choledochal cyst and a left duplex collecting system; no extrahepatic biliary tract obstruction was demonstrated in the surgical specimen (a blind pouch at one of its ends) and the histology study reported complete obstruction of the porta hepatis due to fibrosis; this patient had the best DB percentage (97.2%) of the total. Case 4 developed cholestatic jaundice on the third day of life and had a DB of 3.9, representing 32.2% of the total. Ultrasound study described a fibrous cord at 52 days of life.
Figure 1 shows the DTT. Panel A: catheter in the small bowel; the angle of Treitz can be seen in the left upper quadrant. Panel B: duodenal fluid that was collected over a period of 24 h. Each tube contained fluid collected in a period of 2 h. There was an absence of macroscopic bile in all 4 patients.
Figure 1. Panel A. Duodenal tube test. The catheter tip is in the jejunum and the angle of Treitz can be seen in the left upper quadrant. Panel B. At 24 h, there was no bile visible to the naked eye. Twelve tubes containing duodenal fluid with no bile were collected over a 24-h period. The 4 cases were identical.
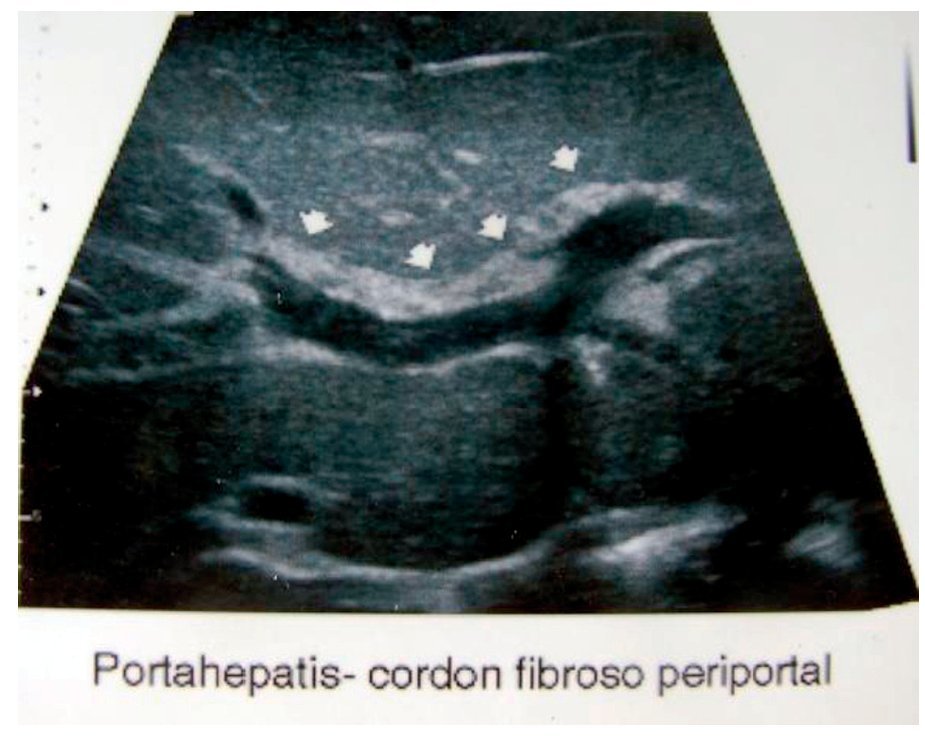
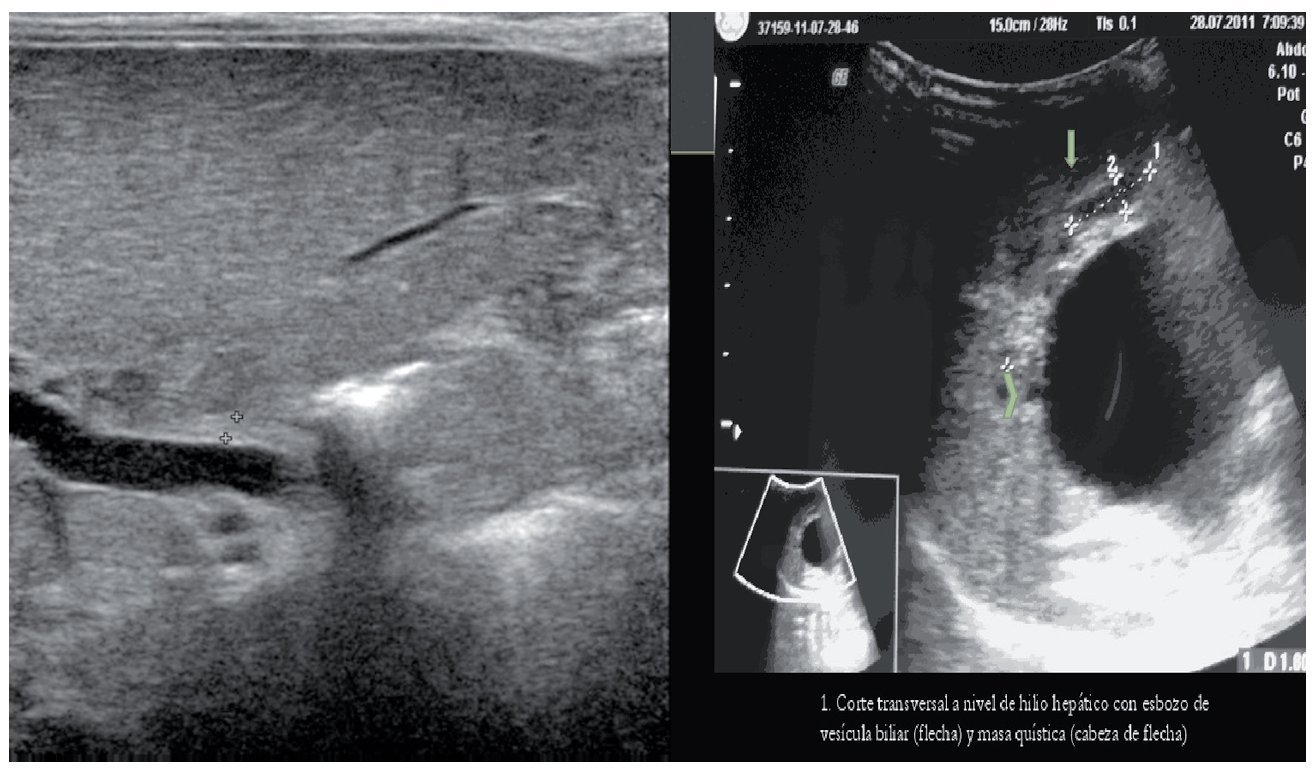
The AUS showed morphologic alterations in the extrahepatic biliary tract: case 4, fibrous cord replacing the bile duct (Fig. 2); neither the gallbladder nor the bile duct were detected in case 1 (Fig. 3); case 3 presented with a choledochal cyst and a suggestion of a gallbladder, and the histopathologic study showed fibrosis at the level of the porta hepatis, where there should be a lumen at the origin of the common bile duct. Intraoperative cholangiography was carried out in 3 of the 4 patients and there was contrast medium extravasation when it was injected into the remnant of the extrahepatic biliary tract. Intraoperative cholangiography was not done in the patient presenting with the choledochal cyst; diagnosis was established by the macroscopic study of the biliary tract that revealed the pouch and microscopic study showed it was associated with hepatitis.
Figure 2. Case 4 at 19 days of life. Liver and biliary tree ultrasound taken in the city of birth, identifying a fibrous cord above the porta hepatis that would normally correspond to the common bile duct with an interior lumen.
Figure 3. Panel A. Case 1. Absence of the gallbladder and bile duct. Panel B. Case 3. Transversal view at the level of the hepatic hilum. The gallbladder and a cystic mass are suggested (arrowhead).
The DTT was proposed in 19791 and its validity was demonstrated by Larrosa in 2001 in a series of 254 cases with a sensitivity of 97.3% and a specificity of 93.7%2; it has since fallen into disuse.3-5 The aim of our study was to show its usefulness when associated with AUS in the diagnosis of extrahepatic biliary atresia (EBA). It consists of placing the distal end of a nasoduodenal catheter distal to the second portion of the duodenum, where the biliary and pancreatic ducts come together, for the purpose of collecting duodenal fluid. The proximal end is placed in a test tube; the catheter is washed every 2 h with saline solution and then placed in the next tube for a total of 12 tubes (24 h); the test is suspended at the moment bile (strong yellow) is visible to the naked eye or when, after 24 h, no bile has been observed in the fluid collected (almost transparent to transparent fluid). When it is positive for bile, communication between the liver and the duodenal lumen is inferred; when it is negative for bile, the opposite is concluded.
This review shows that the DTT associated with AUS is a useful approach for diagnosing EBA in cholestatic jaundice, reducing the time and cost of its diagnosis and surgical correction. The DTT has greater sensitivity and specificity than scintigraphy, thus eliminating the need for its use1; MRC and liver biopsy in cholestatic jaundice diagnosis that are used to demonstrate EBA before undertaking a surgical approach are also unnecessary. We disagree with the diagnostic algorithms of Brady4 and Russo5 because they do not include the DTT in the diagnostic procedures.
The North American Society for Pediatric Gastro enterology, Hepatology, and Nutrition (NASPGHAN) recom mends initiating the diagnostic approach at 15 days.6 However, case 4 had hyperbilirubinemia of 3.9 mg/dL that was documented on the fifth day (30% of the total); the neonate was not pre-term and there was no systemic infection, congenital cardiopathy, or parenteral nutrition. Given such a setting, we feel that cholestatic jaundice study is justified in infants under this age; these figures are not very elevated but their percentage is greater than 15%, suggesting cholestatic jaundice whose origin could be EBA.7 In other words, rather than taking the cut-off point of 4 mg/dL as the value for determining cholestasis, it is preferable to establish the DB percentage in relation to the total bilirubin (TB), regardless of the patient's age.
The clinical data, with DTT and AUS, enable the diagnosis of EBA to be made and can constitute a useful diagnostic approach. In addition, when choluria and DB percentages above 15% are present, even with a TB under 4 mg/dL, it is advantageous to carry out DTT and AUS in neonates.
Financial disclosure
No financial support was received in relation to this article.
Conflict of interests
The authors declare that there is no conflict of interest.
Received 13 August 2012;
accepted 24 October 2012
* Correspo nding author at:
Calle Reforma 355, Colonia Ley 57, Hermosillo, Sonora, Mexico CP 83100.
Tel.: +662 2890 600; Celular phone: 662 1900 947.
E-mail address: jelizondovazquez@gmail.com (J.B. Elizondo-Vázquez).