Endoscopic mucosal resection (EMR) was developed for the purpose of preserving complete gastrointestinal function after the resection of a lesion limited to the mucosa of the digestive tract, as well as for obtaining larger specimens that would enable a precise histopathologic diagnosis.1
In Japan, different techniques were developed for EMR that were divided into three modalities: EMR with a double-channel endoscope, aspiration EMR, and endoscopic submucosal dissection (ESD).2
EMR is typically used for removing lesions smaller than 2cm or removal by sections in large lesions. ESD was developed for en bloc resection (EBR), regardless of the size of the lesion.3
There are important ethical considerations in the formation process of this new technique. Up to the present, the results have been promising. Nevertheless, the lack of training centers, together with potential complications (perforation, bleeding), has limited the expansion of its use in Mexico.
The basic requirements suggested for surgeons and gastroenterologists that wish to perform this technique are: a) certification in gastrointestinal endoscopy, b) training in the use of the devices, techniques, and technologies for identifying and treating premalignant conditions and incipient cancer in the esophagus, stomach, small bowel, and colon, c) experience in hemostasis, and d) training in ESD. A proposed training model encompasses: a first phase in which the procedure performed by qualified specialists is observed; a second phase of practice using inanimate and animate models; a third phase of training in humans under the supervision of qualified specialists; and finally, performing the procedure in humans.4
The aim of this letter was to present the case of a patient with a histologic diagnosis of low-grade intraepithelial gastric neoplasia (low-grade dysplasia) and to provide a literature-based analysis of the role of endoscopic resection in this premalignant condition.
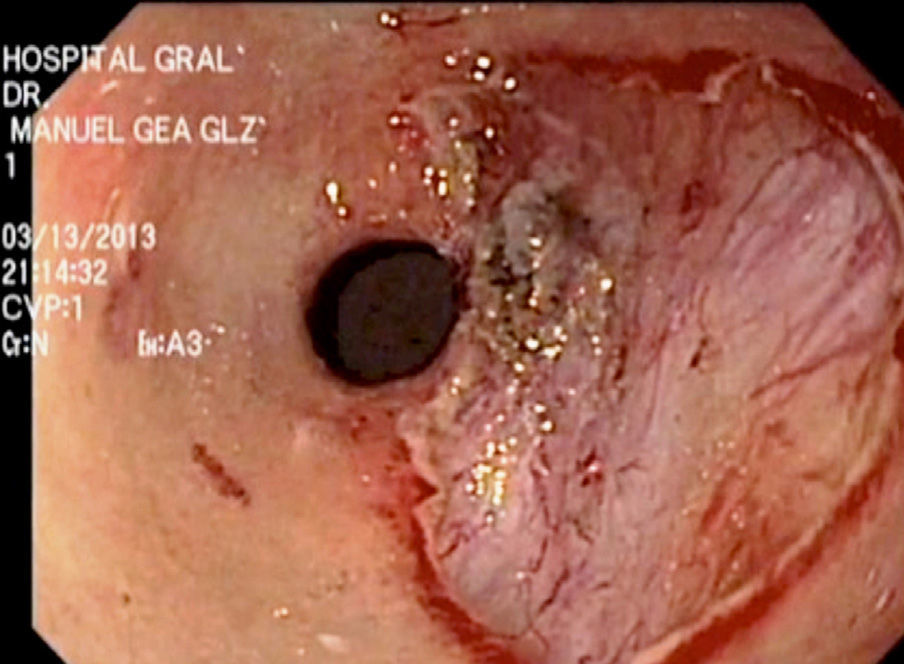
An 81-year-old woman sought medical attention complaining of weight loss of 10kg in 3 months. As part of her evaluation protocol an abdominal computerized axial tomography scan with double contrast was taken that reported probable thickening of the esophageal mucosa (0.8mm). Upper gastrointestinal endoscopy was performed, identifying erosive gastropathy in the fundus and a slightly elevated non-polypoid superficial prepyloric lesion (Paris Classification 0-IIa) that measured 2cm in diameter. Digital chromoendoscopy showed follicular changes in the mucosa with no vascular irregularities.
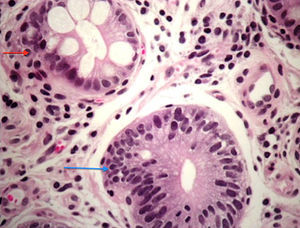
The histopathologic report of the biopsies described low-grade intraepithelial neoplasia / dysplasia (World Health Organization Classification) in the antral mucosa (Fig. 1) and mild focal atrophy that was negative for Helicobacter pylori. Preoperative laboratory study results were within normal parameters.
For the purpose of obtaining a precise histologic diagnosis of a well-defined lesion, 2 endoscopists skilled in the ESD technique (MR and JH) performed the procedure after receiving the informed consent of the patient.
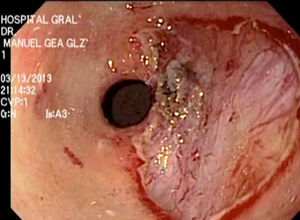
An Olympus GIF-180 gastroscope was employed. Indigo carmine at 5% was applied to define the margins of the lesion by contrast. An endoscopic Flex Knife® was used to mark the circumference of the lesion with monopolar energy (cut 70/coagulation 30); the submucosa was infiltrated with 3 cc of saline solution at 0.9% and 1.5 cc of hyaluronic acid using an injector (Olympus NM-200U0423). The circumferential cut of the lesion was made with the endoscopic Flex Knife and the submucosa was dissected with the IT Knife2®, until the lesion was completely resected (Fig. 2).
Hemostasis was verified and the operative field was irrigated with saline solution after resection. Surgery duration was 65minutes and there were no complications. The previous diagnosis was confirmed by histopathology.
Intraepithelial neoplasia of the gastric mucosa is the penultimate stage of carcinogenesis. It is defined as a non-invasive gastric neoplasia, characterized by cellular atypia and by abnormal differentiation and disorganization of the glandular architecture.5
The correct diagnosis and grade classification of intraepithelial neoplasia is crucial because it predicts the risk for malignant transformation. You et al. conducted a prospective study on 546 patients with dysplasia during the 5-year follow-up and found that gastric cancer progression was 0.6% per year for low-grade dysplasia and 1.4% for high-grade dysplasia.6
De Vries et al. included 7,616 patients with low-grade dysplasia and 562 with high-grade dysplasia during a 5-year follow-up. The annual incidence of gastric cancer was 0.6% for low-grade dysplasia and 6% for high-grade dysplasia.7
The European Society of Gastrointestinal Endoscopy (ESGE) recommends endoscopic resection for the purpose of obtaining a precise histologic diagnosis in patients presenting with low-grade dysplasia in whom a well defined lesion has been identified during the endoscopy.8 Kim et al. evaluated the discrepancy in the diagnosis of low-grade dysplastic lesions obtained with biopsy forceps or EMR in 273 patients and found histologic concordance in 73%; 19% of the cases presented with higher-grade dysplastic lesions, and even adenocarcinoma, after resection.9
In a case series of 41 patients, Hull et al. found discordance in 39% of the cases regarding diagnoses obtained with biopsy forceps and EMR. The authors concluded that EMR was superior in diagnosing superficial lesions, particularly those that are larger than 10mm.10
Further studies are needed that evaluate the risk / benefit of endoscopic resection of the gastric mucosa in patients diagnosed with low-grade intraepithelial neoplasia.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Quiroz-Guadarrama CD, Herrera-Esquivel JJ, Rojano-Rodríguez M, Del Rio-Suarez I, Morales-Vargas JM, Mucio M. Disección endoscópica de la submucosa gástrica en neoplasia intraepitelial de bajo grado. Revista de Gastroenterología de México. 2014;79:149–151.