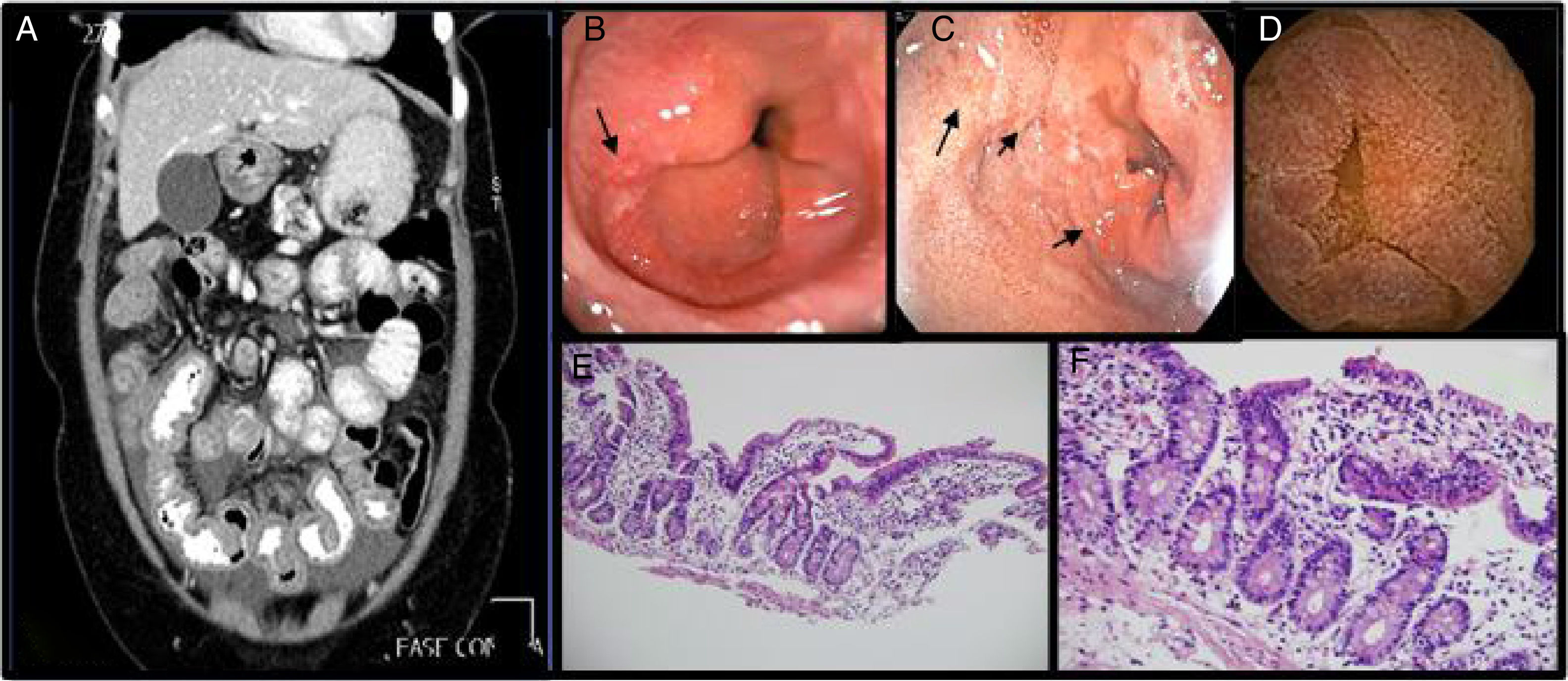
Eosinophilic gastroenteritis is a rare and under-diagnosed disease that is a great diagnostic challenge. We present herein the case of a 40-year-old woman with a past medical history of asthma and dyspepsia, whose present illness began with symptoms of colicky abdominal pain in the epigastrium for 10 days that radiated to the entire abdomen, with an intensity of 6/10 on the analogue scale for pain. She had postprandial worsening, no nausea or vomiting, and no improvement with analgesics taken at home. Upon hospital admission, the patient's vital signs were stable, and physical examination revealed pain in the mesogastrium and hypogastrium upon palpation, with no peritoneal irritation, and ascites. Leukogram showed leukocytes at 10,800 cells/mm3 and eosinophils at 21.4% (absolute count: 2,311 cells/mm3). Abdominal computed tomography scan identified diffuse and concentric thickening of the small bowel segments and a moderate quantity of abdominopelvic fluid (fig. 1A). Diagnostic paracentesis was carried out, obtaining 65 cc of slightly turbid fluid. Cytochemical results were 2,600 leukocytes with 95% eosinophils.
A. Ascites, diffuse and concentric thickening of the small bowel. 1B and 1C. UGIE with changes suggestive of eosinophilic esophagitis and duodenitis. 1D. Capsule endoscopy: mucosa with edema and erythema that produces thickening of the villi. 1E Ileum (H&E-x100). Preserved ileal mucosa with slightly enlarged and flattened villi with lymphocytic inflammatory infiltrate, the presence of a greater number of eosinophils and crypts with some branches. 1F. Ileum (H&E-x400). Ileal mucosa at a greater magnification showing a larger number of lymphocytes and eosinophils than usual in the lamina propria, which carry out exocytosis into the superficial epithelium and crypts.
Upper gastrointestinal endoscopy revealed linear grooves, a crackled aspect suggestive of eosinophilic esophagitis, and other inflammatory gastrointestinal changes (fig. 1B and 1C). However, there was an insignificant eosinophilic count in the esophageal biopsy: 1-10 per high power field (hpf). Capsule endoscopy was indicated for the complete evaluation of the small bowel and it identified marked edema, congestion, and erosions with scant bleeding (fig. 1D). Biopsies of the jejunum were taken, using anterograde double-balloon enteroscopy, and the pathology study reported mononuclear inflammatory activity, an increased number of eosinophils in accumulations (28-30 per hpf), with exocytosis in the crypts and perivascular accumulations (figs. 1E and 1F).
Because there were no extraintestinal symptoms and echocardiography was normal, infiltrative involvement in other organs was ruled out. No parasitic or bacterial infectious pathology was identified in serial stool samples or stool cultures, there were no symptoms of autoimmune disease, and the antibody profile was negative. The patient did not complain of B-symptoms, biopsy revealed no susceptible adenopathies, tryptase measurement was negative, and bone marrow studies were performed, and the FLIPI index was calculated, to rule out hematologic disease, including hypereosinophilic syndrome. All the studies were negative.
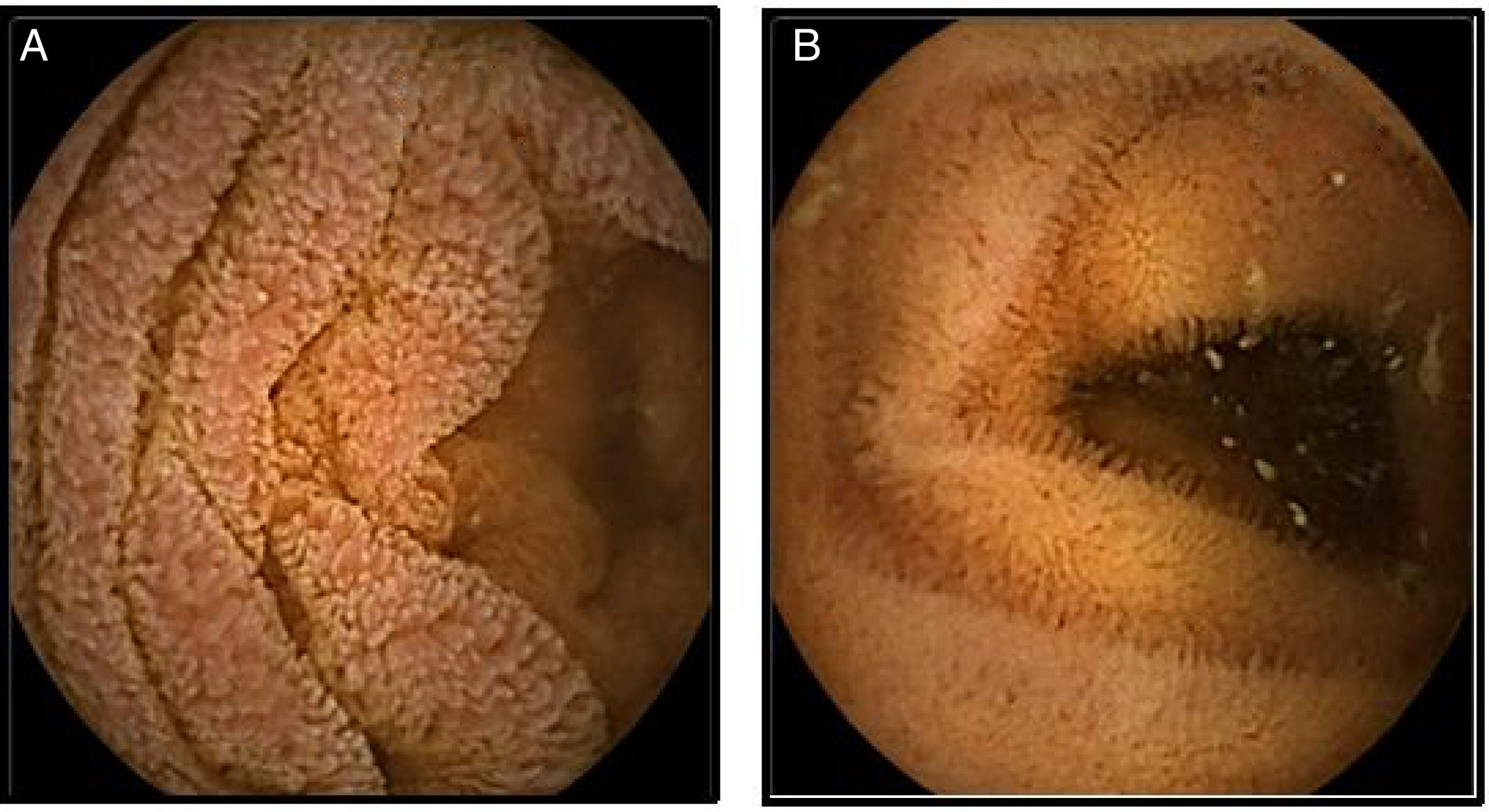
The patient was managed with 50mg/day of prednisolone for one month. Gradual clearance was begun, receiving a total of 13 weeks of treatment and indications for a low-antigen diet. The patient had great symptom improvement and the peripheral eosinophilia and endoscopic and imaging findings were resolved (figs. 2A and 2B).
Eosinophils are part of the innate immune system and are essential as defense: they are found in the entire gastrointestinal tract, except the esophagus, and can increase in number, not just under infectious conditions, but also in relation to connective tissue diseases, myeloproliferative diseases, inflammatory bowel disease, hypereosinophilic syndrome, and hypersensitivity due to medications or toxic substances.
Gastrointestinal eosinophilia is recognized when eosinophils infiltrate tissues and there is no clear triggering cause,1,2 and can present in esophagitis, gastritis, gastroenteritis, enteritis, and colitis, and is named according to the compromised area.2
Incidence is difficult to estimate, given that it is an uncommon, and most certainly under-diagnosed, disease. There are approximately 1 to 20 cases for every 100,000 patients. According to the classic description by Talley et al.,3 eosinophilic gastroenteritis has three predominant presentation forms: the first is in the mucosa, the second is in the muscle layer, and the third is in the subserosa. In our patient, there was evidence of mucosal and serosal involvement, identified through endoscopic and histopathologic studies. In addition, the diseases in the very thorough differential diagnosis were ruled out.
Little is known of its pathophysiology, but it is thought to be part of the allergic alterations mediated by immunoglobulin E (IgE), apparently secondary to a CD4Th2 immune response, regardless of the presence or absence of eosinophilia in blood.4,5 It has been clearly demonstrated that the infiltration of eosinophils into tissue and their degranulation lead to fibrosis of the tissue, thrombosis, small vessel vasculitis, and persistent inflammation.5 In eosinophilic gastroenteritis, interleukin (IL)-3, IL-5 and granulocyte-macrophage colony-stimulating factor may be responsible for eosinophil recruitment and activation.4
Symptoms are nonspecific and depend on the segment involved, disease extension, and the degree of depth that is compromised. In cases of superficial involvement, there is often abdominal pain, nausea, vomiting, or diarrhea, but malabsorption syndromes, protein-losing enteropathy, and weight loss can also present. Infiltration of the deep layers of the wall result in thickening and altered motility, which is why bowel obstruction can develop. When the subserosa is compromised, which is very uncommon, eosinophilic ascites presents,6 as occurred in our patient.2,4,7
The four diagnostic criteria are: symptoms, eosinophilic infiltration of the gastrointestinal tract, exclusion of other causes of eosinophilia, and no involvement of other organs.1,4
Peripheral eosinophilia is found in 20 to 80% of cases.1,4 Imaging study findings are nonspecific and can be absent in 40% of the patients. Irregular nodular thickening at the level of the folds in the distal part of the stomach and the proximal part of the small bowel can be seen through abdominal computed tomography. Nodular, friable, erythematous, and occasionally ulcerative mucosa can be seen at endoscopy. Biopsies of both the visually healthy and unhealthy mucosa should always be taken.1,4,7
The exact number of eosinophils in tissue for making the diagnosis of eosinophilia is not clear, but > 20 eosinophils per hpf in the majority of the gastrointestinal tract, with the exception of the colon (> 50 eosinophils per hpf in the right colon, > 35 in the transverse colon and > 25 in the left colon) are considered necessary.8
Treatment includes restrictive or elemental diets 2,9 and steroids. Even though there are no randomized clinical trials on steroid effectiveness, case reports have shown response rates of up to 90%, utilizing different doses, administration routes, and treatment duration.4 The use of mast cell stabilizers (sodium cromoglicate, leukotriene receptor antagonists, antihistamines such as ketotifen), biologic drugs such as anti-interleukin-5 (mepolizumab, reslizumab), anti-Ig-E (omalizumab), and tumor necrosis factor-alpha inhibitors (infliximab, adalimumab, and etanercept) have also been described. Randomized controlled trials are required to clarify their efficacy and safety in the management of those patients.1
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Sylva D, Tamayo L, Mosquera-Klinger G, Carvajal JJ, Pérez JC. Gastroenteritis eosinofílica: presentación inusual de una enfermedad poco común. Revista de Gastroenterología de México. 2019;84:116–118.