Antecedentes: Existen pocos estudios que analicen las complicaciones de la yeyunostomía y los factores asociados a aquellas.
Objetivo: Describir la tasa de complicaciones y analizar los factores asociados al desarrollo de las mismas en un centro de referencia de tercer nivel de México.
Métodos: Se realizó un estudio retrospectivo de pacientes sometidos a yeyunostomía tipo Witzel desde enero del 2002 hasta diciembre del 2011. Se recabaron los datos demográficos, clínicos y de laboratorio a su ingreso y durante su seguimiento. Se analizaron los factores asociados al desarrollo de complicaciones, utilizando las pruebas de la chi al cuadrado para variables categóricas y de la t de Student para variables continuas. Se consideró significativa a una p < 0.05.
Resultados: Se incluyó a 112 pacientes (57 hombres), con una media de edad de 54,2 años; 48 pacientes (42.9%) tuvieron complicaciones postoperatorias. Las complicaciones quirúrgicas más frecuentes fueron sepsis grave (11.6%) y el choque séptico (7.14%). Las complicaciones médicas más frecuentes fueron el derrame pleural (7.14%) y la neumonía por broncoaspiración (6.25%). Los factores asociados significativamente con el desarrollo de complicaciones fueron obesidad, linfopenia e hipoalbuminemia.
Conclusiones: La yeyunostomía se asocia a una elevada frecuencia de complicaciones, tanto médicas como quirúrgicas. Si bien se ha establecido como una mejor alternativa a nutrición parenteral, deberá tomarse en cuenta la morbilidad asociada a la misma antes de establecer su utilización rutinaria como medio de aporte nutricional, particularmente en pacientes con factores asociados al desarrollo de las mismas.
Background: There are few studies in the literature that analyze jejunostomy complications and their associated factors.
Aims: To describe the rate of complications and analyze the factors associated with their development in a tertiary reference center in Mexico.
Methods: A retrospective study was carried out on patients that underwent Witzel jejunostomy within the time frame of January 2002 to December 2011. Patient demographic, clinical, and laboratory data were collected at the time of hospital admission and during follow-up. The factors associated with the development of complications were analyzed using the chi square test for categorical variables and the Student's t test for the continuous variables. Statistical significance was considered with a p<.05.
Results: One hundred and twelve patients (57 men) with a mean age of 54.2 years were included in the study. Forty-eight patients (42.9%) presented with postoperative complications. The most frequent surgical complications were severe sepsis (11.6%) and septic shock (7.14%) and the most frequent medical complications were pleural effusion (7.14%) and aspiration pneumonia (6.25%). The factors that were significantly associated with the development of complications were obesity, lymphocytopenia, and hypoalbuminemia.
Conclusions: Jejunostomy is associated with an elevated medical, as well as surgical, complication frequency. Even though it has been established as a better alternative to parenteral nutrition, its associated morbidity should be taken into consideration before establishing its routine use as a means of nutritional support, especially in patients with factors associated with the development of complications.
Introduction
Jejunostomy is a surgical procedure in which a tube is introduced into the proximal jejunal lumen for the fundamental purpose of providing nutrition.1 There are different techniques2,3: the longitudinal Witzel, transverse Witzel, Roux-en-Y, open gastrojejunostomy, needle catheter, the percutaneous endoscopic technique, and the laparoscopic method. The main indication for jejunostomy is as an additional procedure in the course of a major intervention in the upper gastrointestinal tract.
Jejunostomy enables the initiation of enteral feeding in the first 24 postoperative hours, especially in patients at high risk for complications (anastomosis leak, cicatrization delay), prolonged postoperative venti lation, polytrauma, pre-existing malnutrition, gastroparesis (diabetes), post-pyloric obstruction, cranial trauma, and patients receiving chemotherapy and radiotherapy.4 Contraindications may be:
— Local: inflammatory bowel disease; plastic peritonitis; enteritis from radiation; the potential risk for enterolysis; and the danger of enterocutaneous fistula.
— Systemic: severe immunosuppression; the risk for necrotizing fasciitis; coagulopathy from the possibility of a hematoma in the intestinal wall, obstruction, and ascites; and the risk for leaks and infection.
Like all surgical procedures, jejunostomy presents a risk for both medical and surgical complications. The principal secondary complications of a jejunostomy for enteral nutrition can be classified as mechanical, infectious, gastrointestinal, and metabolic.1,4 In our environment there are very few studies that have analyzed the factors related to these complications. Knowledge of the factors associated with the development of these pathologic events will enable the pursuit of other feeding alternatives, such as a nasoenteral catheter or total parenteral nutrition, in at-risk patients. The aim of the present study was to describe the complication rate of jejunostomy using the longitudinal Witzel technique performed at a tertiary referral center in Mexico and to analyze the factors associated with their development.
Methods
A retrospective cross-sectional study was conducted on patients that underwent Witzel jejunostomy at a referral center in Mexico City within the time frame of January 2002 and December 2011. This type of jejunostomy was chosen for review because it is the technique most commonly employed in our institution; other jejunostomy methods are rarely used. All the clinical case records involving this procedure were examined, regardless of the patient's age, sex, underlying disease, and comorbidities. The demographic, clinical, and laboratory data were collected upon hospital admission and during outpatient follow-up. Patients that were admitted to our hospital due to jejunostomy complications were excluded from the study if their operation had been performed at another hospital. The complications associated with the jejunostomy and the factors involved in that event were the primary outcome of the study.
The complications were those that occurred no longer than 30 days after surger y or release from medical care. The variables were defined as follows: patients over 65 years of age were regarded as the elderly, a body mass index (BMI) above 30 was associated with obesity, and malnutrition was an index under 18. All patients with hemoglobin under 12 mg/dL were considered as presenting with anemia, regardless of their sex. The normal lymphocyte range employed was from 20 to 40%, and hypoalbuminemia was an albumin value under 3.5 g/dL. Septic shock was defined as the association between infection and hemodynamic failure, and in some cases, with visceral failure. Sepsis was described as the presence of an inflammatory response (leukocytosis, fever and/or tachycardia and tachypnea) in the presence of a focus of infection, whereas septic shock was regarded as these same data together with hemodynamic involvement.
The SPSS version 19 program was used for the descriptive statistics with measures of central tendency and dispersion, in accordance with the distribution of the variables. The Student's t test was employed for the continuous variables and the chi-square test for the categorical variables. The odds ratio with a 95% confidence interval (CI) was analyzed for the factors associated with the development of complications. Statistical significance was considered with a p < 0.05.
Results
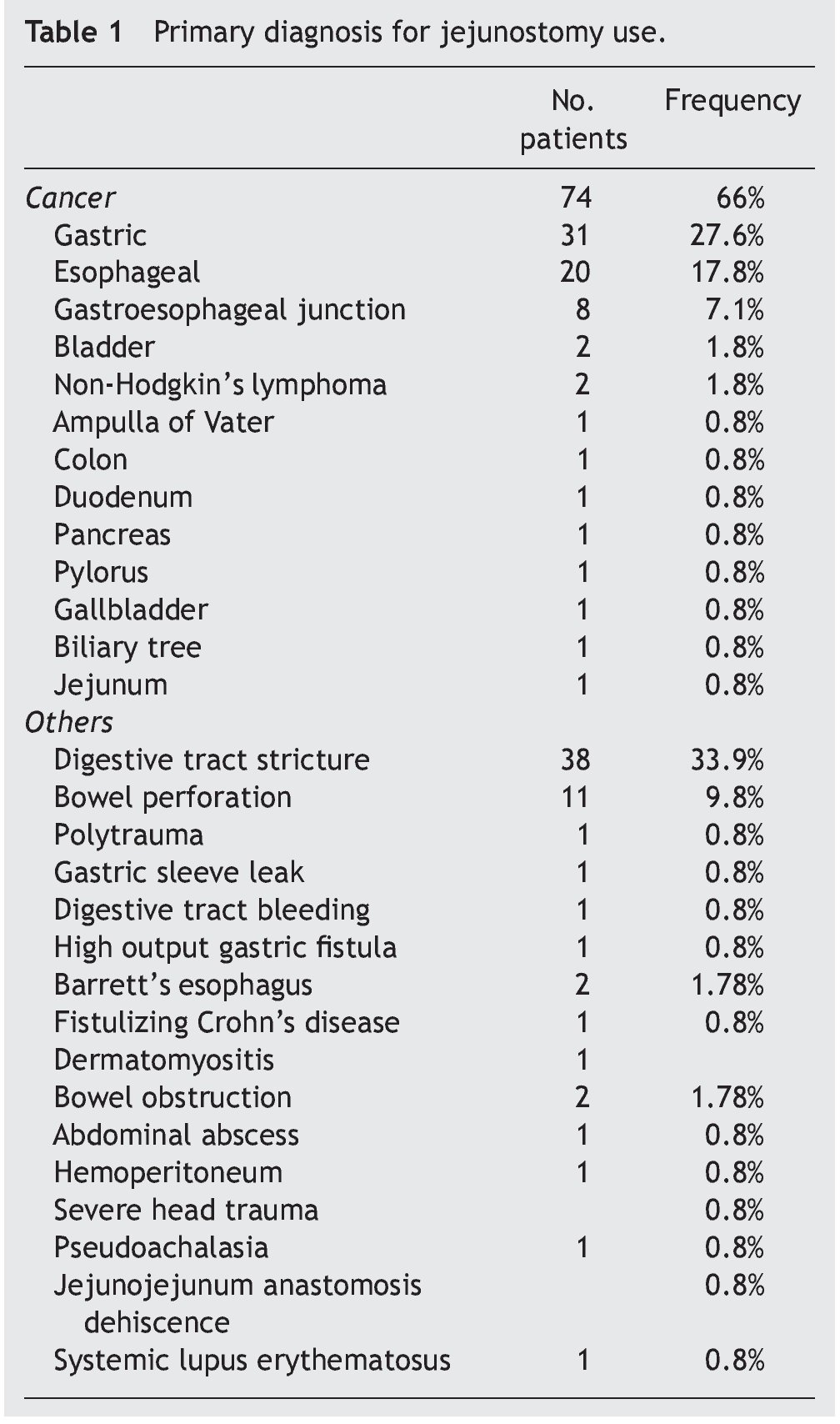
This study included 112 patients (55 women and 57 men) with a mean age of 54.2 ± 12.3 years and a median of 56 years (range, 17-86 years). In 74 cases (66%), the patients presented with malignant tumor. The most frequent ones were gastric cancer with 31 cases (27.6%) and esophageal cancer with 20 cases (17.85%). The rest of the causes are described in Table 1.
The mean of the BMI was 22.08 (range 12-38). Eight patients (7.14%) were obese at the time of surgery and 15 patients (13.39%) were malnourished. The remaining 89 patients (79.46%) had adequate weight for their height.
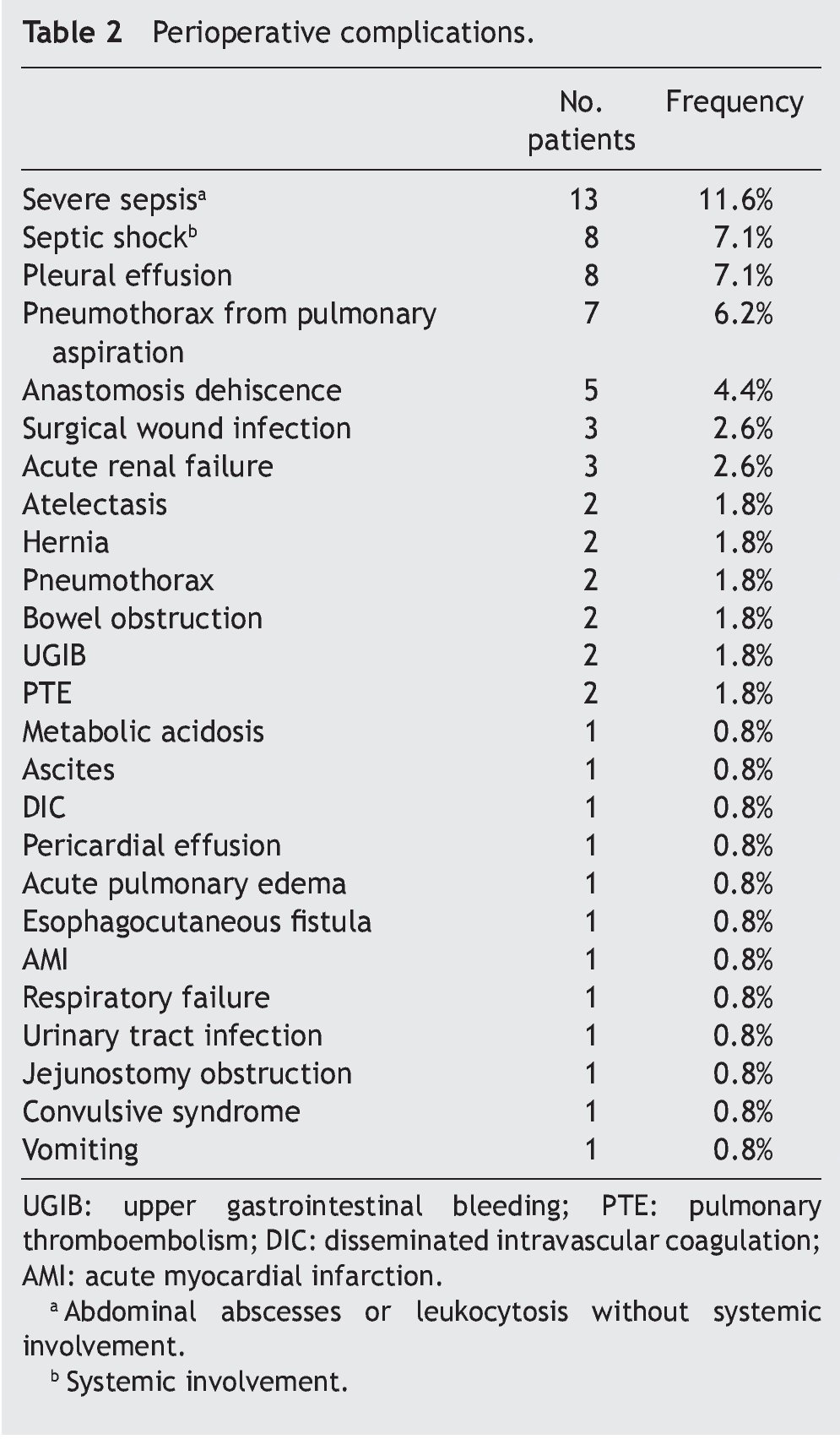
Other surgical interventions were carried out at the same time as the jejunostomy in 91 patients (81.25%). Of the patient total, 48 (42.9%) had postoperative complications. The number of surgical complications was 39 (34.82%) and the most frequent were: 13 cases (11.6%) of severe sepsis and 8 cases (7.14%) of septic shock. A total of 33 patients (29.46%) presented with medical complications, among which the most frequent were 8 cases (7.14%) of pleural effusion and 7 cases (6.25%) of pneumothorax due to pulmonary aspiration. The remaining postoperative complications are described in Table 2. Thirteen patients (11.6%) in the study had both medical and surgical complications.
In the analysis of the factors associated with complications after the jejunostomy, obesity (OR 2.3 95% CI 1.2-5.7; p = 0.011) and hypoalbuminemia (OR 1.9 95% CI 1.1-4.9; p = 0.027) were significantly associated with the development of surgical complications. On the other hand, lymphocytopenia was associated with the development of medical complications (OR 1.5 95% CI 1.2-3.4; p = 0.012), as well as with the develop ment of complications in general (OR 1.6 95% CI 1.3-5.1; p = 0.003).
Discussion
Malnutrition is a significant problem in patients undergoing major gastrointestinal surgery. Patients with neoplastic lesions of the upper digestive tract can arrive at surgery with a deficient nutritional status, which, along with the habitual postoperative prolonged fast, makes the implementation of nutritional support advisable. Thus, providing nutrition has become a vital part of conventional postoperative care and is a customar y practice in many centers in which abdominal resection surgery is performed.
In various randomized clinical trials and meta-analyses, postoperative enteral nutrition has been shown to be safer than parenteral nutrition and is associated with significantly lower postoperative morbidity. It also preserves the enteric flora and results in the use of fewer resources.5-8 Different routes have been utilized, but the safest and most effective feeding route is still not clear and the choice continues to be based on the surgeon's familiarity with a given technique. In our institution, the jejunostomy technique used almost exclusively is the Witzel technique. It is preferred to parenteral feeding because, as mentioned above, the use of the enteral route is associated with a lower number of complications, particularly infectious ones. Because ours is a retrospective study and the choice of catheter placement depended on the attending physician in each particular case, we do not know if there were nutritional support alternatives to jejunostomy in each case, nor do we know why this route was chosen.
There is a risk for the development of complications with jejunostomy catheter placement, as there is with any surgical procedure.2,9-12 In the bibliography reviewed, the frequency of these complications varies from 2 to 65%.13-15 This variation is partially due to the fact that some authors13,14 consider digestive symptomatology to be a complication caused by catheter use, while others do not.2,11 On the other hand, in the prospective study conducted by Jones et al.,15 123 patients operated on for major abdominal trauma were divided into two groups; the study group was the patients that had undergone a jejunostomy and the control group was the patients that received parenteral nutrition. The clinical presentation of gastrointestinal symptoms was evaluated in both groups and the comparative study showed no significant differences between the 2 groups.
In our study, from the patient total, 48 (42.9%) had postoperative complications. The number of surgical complications was 39 (34.82%), the most frequent of which were sepsis, with 13 cases (11.6%), and septic shock, with 8 cases (7.14%). Sepsis is reported in the medical literature as one of the most common complications.2,13,16,17 A total of 33 cases (29.46%) presented with medical complications, and the most frequent were pleural effusion, with 8 cases (7.14%), and pneumonia due to pulmonary aspiration, with 7 cases (6.25%). These are also reported as major complications in the medical literature.13,18,19,22 Thirteen patients (11.6%) in the study presented with both medical and surgical complications.
Hypoalbuminemia is one of the factors involved in the incidence of jejunostomy complications; it is also related to postoperative risk factors involving the digestive tract in cases of rectal cancer,19-27 colostomy,26-28 ileus,29-32 and hepatic complications.33,34 In the medical literature, hypoalbuminemia is described as a malnutrition marker, and it has also been reported on in relation to the mortality associated with chronic diseases. Its role in acute pathology is not well understood,35,36 making it a significant variable in major surgery; its presence prolongs hospital stay.
Lymphocyte count has also been described as a general health status marker in these patients, as well as a malnutrition marker. In other studies it has been found to be a risk factor for the development of complications possibly due to a deficient immune response; it has also been described as a marker for general health status deterioration, including severe malnutrition.37
In addition, obesity is a predisposing factor for the development of surgical complications, because tissues are more friable when there is a great quantity of fatty deposits, facilitating wound dehiscence or infection. In our study, both obesity and hypoalbuminemia doubled the risk for developing surgical complications in patients undergoing jejunostomy catheter placement.
The strengths of this study are that it is one of the few that has analyzed the factors associated with these complications, it was conducted in the same institution, and the postoperative progression was well documented. Perhaps we have overestimated the complication rate because in order to avoid study bias we included all complications that developed within a 30-day postoperative time lapse. At times it was very difficult to distinguish between complications associated with the jejunostomy per se vs. those derived from the underlying pathology of the patient.
In conclusion, jejunostomy is associated with an elevated frequency of medical, as well as surgical, complications. Even though it has been established as a better alternative to parenteral nutrition, its associated morbidity must be taken into account before establishing its routine use as a means of nutritional support. This is especially true in the case of patients presenting with factors associated with the development of such complications, which in our study were obesity, hypoalbuminemia, and lymphocytopenia. In patients with these risk factors, the nutritional support alternatives of nasoenteral catheter feeding and total parenteral nutrition are suggested.
Financial disclosure
No financial support was received in relation to this article.
Conflict of interests
The authors declare that there is no conflict of interest.
Received 17 August 2012;
accepted 21 January 2013
* Corresponding author at:
Dirección de Cirugía. Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán".
Vasco de Quiroga 15. Col. Sección XVI. Tlalpan, Mexico City 14000.
Fax: +55 55739321.
E-mail address: herimd@hotmail.com (H. Medina-Franco).