Gastrointestinal perforation is a surgical emergency that is associated with a high mortality rate and requires special care. During the pandemic, there has been competition with COVID-19 patients for health resources, especially ICU bed availability. The primary aim of our study was to compare the incidence of gastrointestinal perforation during the COVID-19 pandemic, with cases registered before the pandemic.
Materials and methodsA retrospective, observational, single center, cohort study was conducted that included patients that underwent emergency surgery for gastrointestinal perforation in the periods during the pandemic (6 months) and before the pandemic (12 months). Sociodemographic characteristics, comorbidities, duration of hospital and ICU stay, status at discharge, and perforation site were compared.
ResultsThe study included 67 subjects (33 in the pre-pandemic period and 34 in the pandemic period). There were no significant differences regarding sex, age, or comorbidity. The perforation rate per emergency intervention was 4-times higher during the pandemic. There was an increase in the number of patients that were foreigners (4 [11%]) and nonresidents (6 [17%]). ICU admissions decreased (6 [19%]) but ICU stay increased to 137 h. Hospital stay increased by 5 days and delay in care increased 4.5 h. The number of deaths was higher (from 5 [15.2%] to 10 [29.4%]). Four patients with perforations were positive for COVID-19, were admitted to the ICU, and died.
ConclusionsDuring the COVID-19 pandemic there was an increase in the incidence of gastrointestinal perforations at our healthcare system area; symptoms were more advanced, and mortality was higher.
La perforación gastrointestinal es una emergencia quirúrgica asociada a una alta mortalidad que precisa cuidados avanzados. Durante la pandemia ha competido con los pacientes de COVID-19 por los recursos sanitarios, especialmente por la disponibilidad de camas en UCI. El objetivo principal del estudio fue comparar la incidencia de perforación gastrointestinal durante la pandemia por COVID-19 con los casos registrados en prepandemia.
Material y métodosEstudio retrospectivo observacional de cohortes unicéntrico, que incluyó a los pacientes intervenidos de urgencia por perforación gastrointestinal en periodos de pandemia (seis meses) y prepandemia (12 meses). Se compararon características sociodemográficas, comorbilidad, tiempos de ingreso hospitalario y en UCI, situación al alta y localización de la perforación.
ResultadosSe incluyeron a 67 sujetos (33 en prepandemia y 34 en pandemia). No hubo diferencias significativas con respecto al sexo, edad o comorbilidad. La razón de tasas de perforación por intervenciones urgentes fue cuatro veces mayor durante la pandemia. Aumentaron el número de extranjeros; 4 (11%) y no residentes; 6 (17%). Los ingresos en UCI disminuyeron (6 [19%]), aunque su estancia se prolongó 137 horas. La estancia hospitalaria aumentó 5 días y la demora en la atención 4.5 horas. Aumentaron las perforaciones de intestino grueso (3 [8%]). La mortalidad fue mayor; 10 (29.4%) frente a 5 (15.2%). Hubo cuatro pacientes perforados COVID-19 positivos, todos ellos fueron a UCI y fallecieron.
ConclusionesDurante la pandemia por COVID-19 hubo un aumento de la incidencia de perforaciones gastrointestinales en nuestra área de atención, con cuadros más evolucionados y mayor mortalidad.
Gastrointestinal perforation is a common surgical emergency associated with high mortality.1 The causes and factors involved in its appearance are numerous and determine lesion location.2,3
The prognosis and survival of those patients is conditioned by the location and size of the perforation, the presence of associated diseases, and progression time. Patients require much care and have prolonged hospital stay, utilizing vast amounts of resources. They tend to require care in the intensive care unit (ICU), and during the pandemic, have had to compete for ICU beds with patients with severe COVID-19 disease.
Since the time the COVID-19 pandemic was declared, healthcare systems and hospitals have had to adapt to the new situation. ICU capacity had to be broadened, resulting in the conversion of recovery units, and even waiting rooms, into ICUs.4 Healthcare personnel had to be redistributed and consultations were canceled or conducted by telephone.5 A huge effort was made to reorganize all activity to meet the most urgent needs, in a setting of resource scarcity,4,6 all of which had a strong impact on normal healthcare activity.7 User access to the healthcare services has also been conditioned. The imposed measures of social distancing, curfew, lockdown, and fear of contagion have been evaluated as causes of greater delay in meeting healthcare demands, a lower incidence of interventions in mild processes, and an increased number of cases presenting with advanced stages of disease.8,9
The current situation obliges us to study the manner in which all those changes have affected the provision of healthcare, to improve the management of the existing resources. Although there is scant scientific evidence on the topic, increasingly more studies demonstrate the need for continuing that line of investigation.10–13
Throughout the pandemic, we detected an increase in gastrointestinal perforation cases at our hospital, as well as a more advanced progression status in those patients. The need to conduct a study to confirm said trend and identify the factors involved in it became apparent.
The primary aim of our study was to compare the incidence of gastrointestinal perforation, in periods before and during the pandemic. The secondary aim was to describe the profile of the patients with gastrointestinal perforation and identify the factors related to the potential increase of incidence of the problem during the pandemic.
Materials and methodsA retrospective, observational, single-center cohort study was conducted that included patients that underwent emergency surgery for gastrointestinal perforation, in the periods before and during the pandemic. The selection of the study periods was made from data provided by the Junta de Andalucía, according to the progression of confirmed COVID-19 rates for the province of Málaga. The interval of six months was chosen for the pandemic period, in which the number of COVID-19 cases per 100,000 inhabitants was above 100, from September 1, 2020 to February 28, 2021. The pandemic period was compared with the same pre-pandemic periods from the two previous years (Pre-pandemic; Period 1.- from September 1, 2018 to February 28, 2019; Period 2.- from September 1, 2019 to February 28, 2020).
The study was carried out at the Hospital Costa del Sol de Marbella (Málaga). The hospital belongs to the Costa del Sol Health Agency and is a referral center of the Costa del Sol Healthcare System Area that serves a population of 491,619 inhabitants, according to the January 1, 2020 municipal register.
Study subjects. Patients were selected that underwent emergency surgery due to gastrointestinal perforation during the two time periods. Patients operated on that were diagnosed with acute abdomen, peritonitis, and sepsis caused by a perforation and registered in the surgical protocol were also added. The information from the clinical histories of the patients was collected from the Hospital Costa del Sol database, for later statistical analysis.
Study variables. The main study variable was the accumulated incidence (or rate) of the intervention carried out per diagnosis of gastrointestinal perforation (or diagnosis of acute abdomen, peritonitis, or sepsis registered in the surgical protocol), with respect to the total of emergency gastrointestinal surgical interventions. The sociodemographic variables of age, sex, nationality, and municipality of residence were collected. Comorbidity was registered through the Charlson Comorbidity Index and the Surgical Risk Scale (SRS),14 which encompasses the Confidential Enquiry into Perioperative Deaths (CEPOD), the risk classification of the American Society of Anesthesiologists (ASA), and the magnitude of surgery, according to the British United Provident Association (BUPA). In addition, the interval from the time the patient arrived at the emergency service to the performance of the surgical intervention, the time each patient spent in the ICU and hospitalized, the location of the perforation, the number of hospital discharges, and the number of deaths during hospitalization were registered.
Statistical analysis. Descriptive analyses were carried out, utilizing measures of central tendency, dispersion, and position for the quantitative variables and frequency distribution for the qualitative variables. The incidence of perforations adjusted to the evaluation time per period was calculated with the respective 95% confidence intervals. The differences between periods (pre-pandemic vs. pandemic) were compared using the Student’s t test (or the Mann-Whitney U test in cases of non-normal distribution) for the quantitative variables and the chi-square test (or Fisher’s exact test, in cases of expected frequencies below 5) for the qualitative variables. Statistical significance was set at a p<0.05.
Ethical considerations. The ethical principles from the latest revision of the Declaration of Helsinki and the Good Clinical Practice norms were applied. The study was approved by the Costa del Sol Research Ethics Committee, number 106-04-2021, on April 29, 2021.
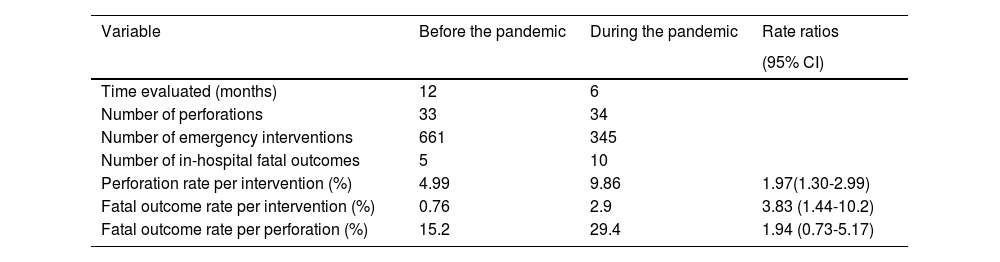
ResultsWithin the time frame of the study, a total of 1,006 emergency gastrointestinal surgeries were performed, 661 of which were carried out within the 12 months evaluated in the pre-pandemic period, identifying 33 perforations. Of the 345 emergency interventions performed within the 6 months of the pandemic period, 34 were perforations. Those data result in an estimated annual perforation rate per emergency surgery of 1.97 (95% CI: 1.30-2.99), and it was higher in the pandemic period (Table 1).
Accumulated incidence and mortality rates of perforations.
| Variable | Before the pandemic | During the pandemic | Rate ratios |
|---|---|---|---|
| (95% CI) | |||
| Time evaluated (months) | 12 | 6 | |
| Number of perforations | 33 | 34 | |
| Number of emergency interventions | 661 | 345 | |
| Number of in-hospital fatal outcomes | 5 | 10 | |
| Perforation rate per intervention (%) | 4.99 | 9.86 | 1.97(1.30-2.99) |
| Fatal outcome rate per intervention (%) | 0.76 | 2.9 | 3.83 (1.44-10.2) |
| Fatal outcome rate per perforation (%) | 15.2 | 29.4 | 1.94 (0.73-5.17) |
Ten in-hospital deaths linked to gastrointestinal perforation were registered during the pandemic period, which supposes a fatal outcome rate per intervention of 3.83 (95% CI: 1.44-10.2), higher than the rate in the pre-pandemic period.
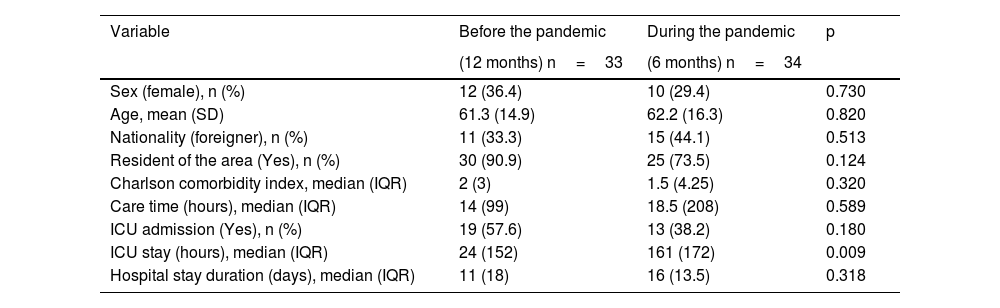
A total of 57.6% of the patients operated on for gastrointestinal perforation in the pre-pandemic period were admitted to the ICU, whereas 38.2% were admitted in the pandemic period. With respect to the distribution of the sociodemographic and clinical characteristics related to the perforations in the two periods, there were no significant differences in any of the study variables, with the exception of ICU stay duration. There was a median difference of 137hours, which was higher in the pandemic period (p=0.009) (Table 2).
Sociodemographic and clinical characteristics regarding perforations in the two study periods.
| Variable | Before the pandemic | During the pandemic | p |
|---|---|---|---|
| (12 months) n=33 | (6 months) n=34 | ||
| Sex (female), n (%) | 12 (36.4) | 10 (29.4) | 0.730 |
| Age, mean (SD) | 61.3 (14.9) | 62.2 (16.3) | 0.820 |
| Nationality (foreigner), n (%) | 11 (33.3) | 15 (44.1) | 0.513 |
| Resident of the area (Yes), n (%) | 30 (90.9) | 25 (73.5) | 0.124 |
| Charlson comorbidity index, median (IQR) | 2 (3) | 1.5 (4.25) | 0.320 |
| Care time (hours), median (IQR) | 14 (99) | 18.5 (208) | 0.589 |
| ICU admission (Yes), n (%) | 19 (57.6) | 13 (38.2) | 0.180 |
| ICU stay (hours), median (IQR) | 24 (152) | 161 (172) | 0.009 |
| Hospital stay duration (days), median (IQR) | 11 (18) | 16 (13.5) | 0.318 |
ICU: intensive care unit; IQR: interquartile range; SD: standard deviation.
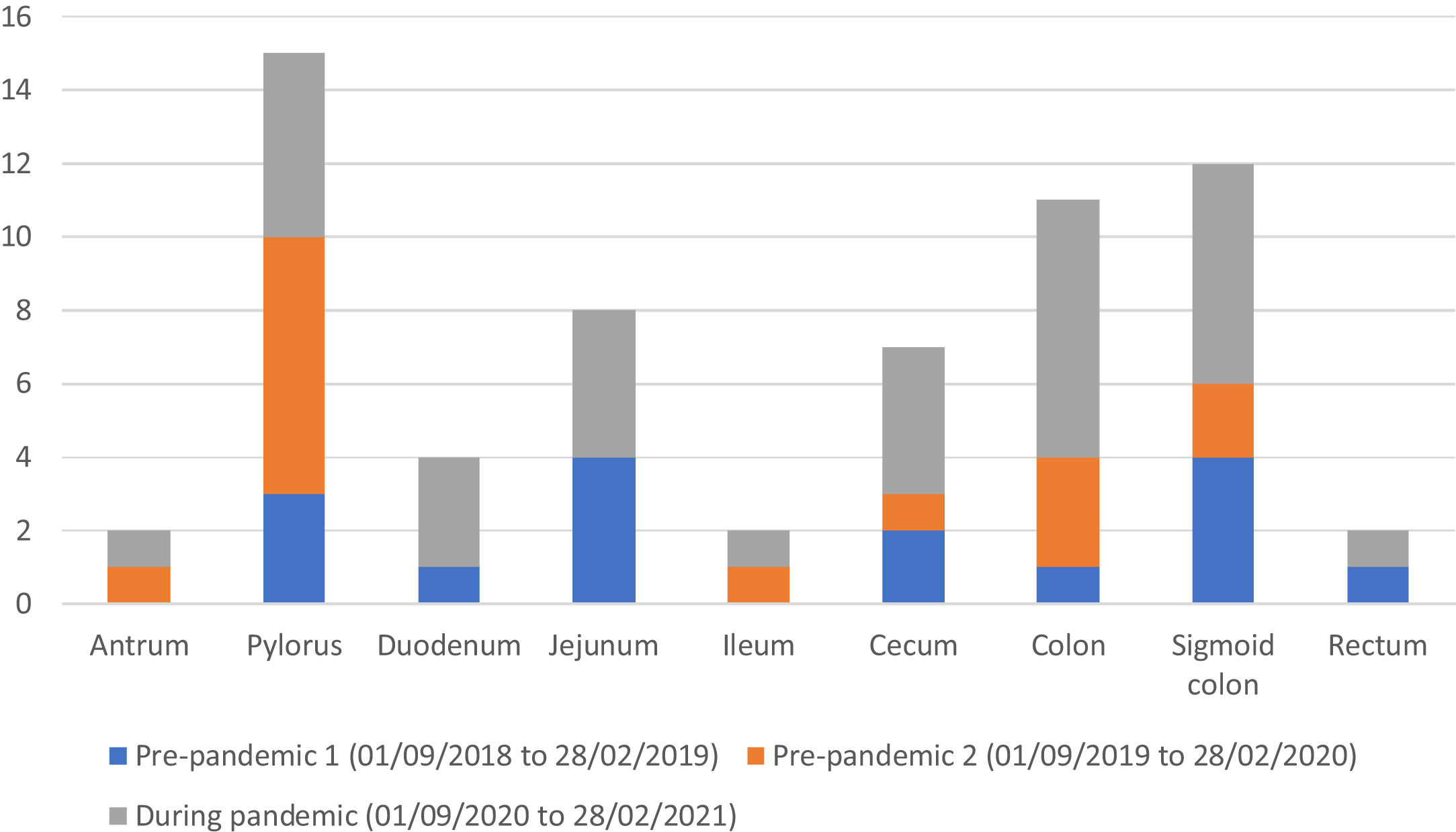
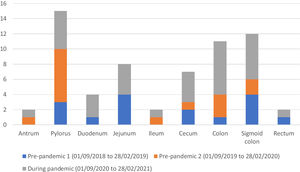
Regarding the distribution of the gastrointestinal perforation site in the two cohorts, location in the large intestine was the most frequent at 42% (6 in the sigmoid colon, 4 in the colon, 3 in the cecum, and 1 in the rectum) in the pre-pandemic patients and at 50% (7 in the colon, 6 in the sigmoid colon, 4 in the cecum, and 1 in the rectum) in the pandemic patients. There were no significant differences between the two cohorts (p=0.514) (Fig. 1).
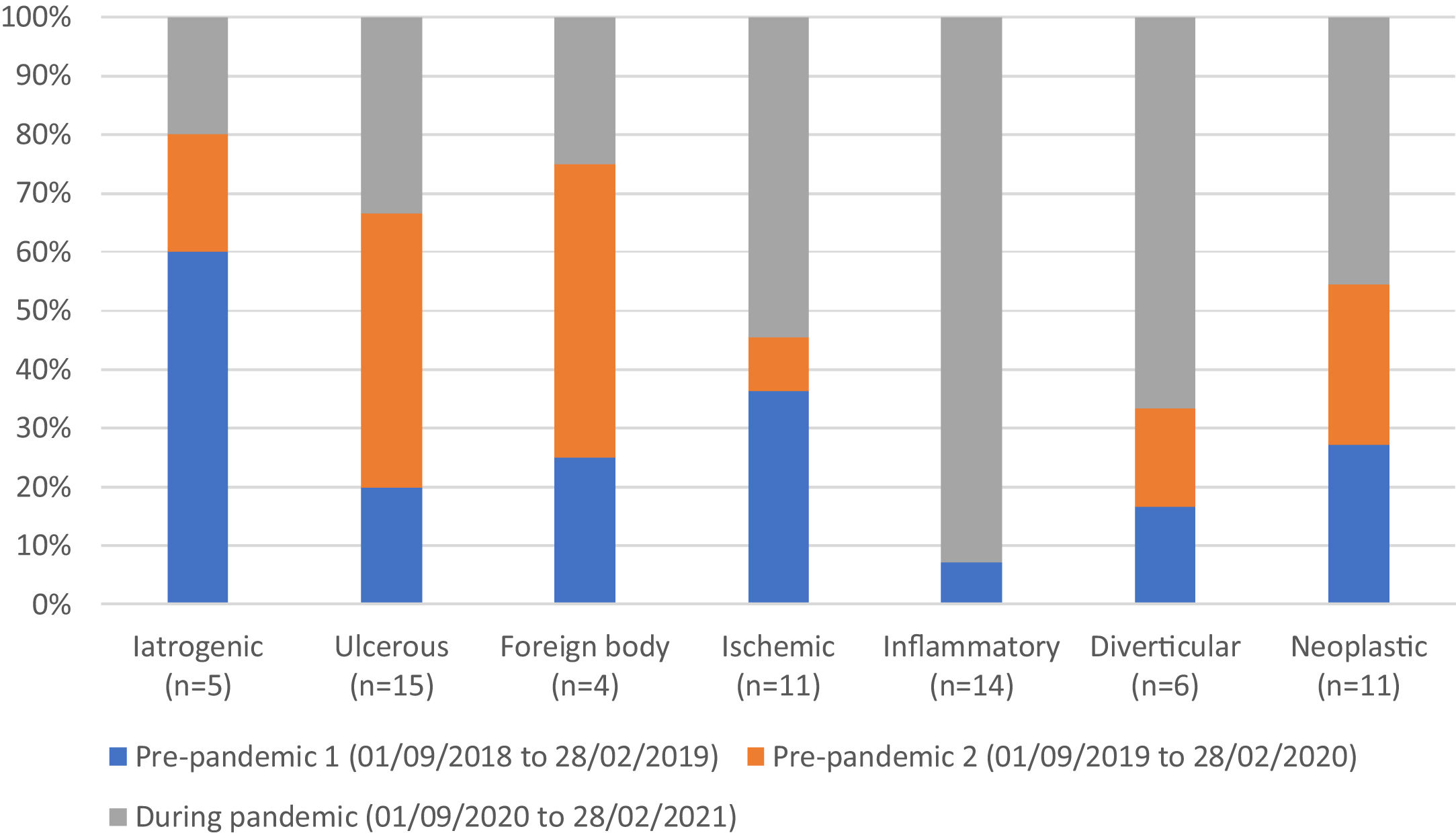
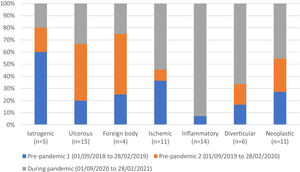
There were differences in the causes of perforation between the two cohorts. An increase in incidence of the inflammatory cause stood out at 38% (13 cases) during the pandemic versus 3% (1 case) before the pandemic (p=0.0018) (Fig. 2).
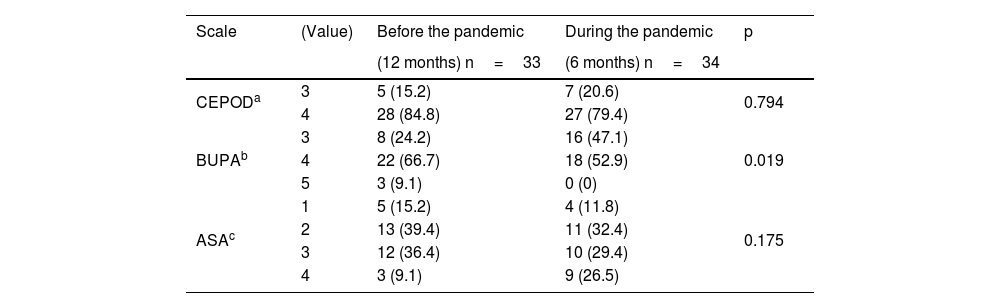
Lastly, regarding the distribution of surgical risks, the BUPA scale produced higher scores in the pre-pandemic period, with 75.8% of the scores on the 4-5 scale versus 52.9% in the pandemic period (p=0.019) (Table 3).
Distribution of surgical risk results; frequency and percentage.
| Scale | (Value) | Before the pandemic | During the pandemic | p |
|---|---|---|---|---|
| (12 months) n=33 | (6 months) n=34 | |||
| CEPODa | 3 | 5 (15.2) | 7 (20.6) | 0.794 |
| 4 | 28 (84.8) | 27 (79.4) | ||
| BUPAb | 3 | 8 (24.2) | 16 (47.1) | 0.019 |
| 4 | 22 (66.7) | 18 (52.9) | ||
| 5 | 3 (9.1) | 0 (0) | ||
| ASAc | 1 | 5 (15.2) | 4 (11.8) | 0.175 |
| 2 | 13 (39.4) | 11 (32.4) | ||
| 3 | 12 (36.4) | 10 (29.4) | ||
| 4 | 3 (9.1) | 9 (26.5) |
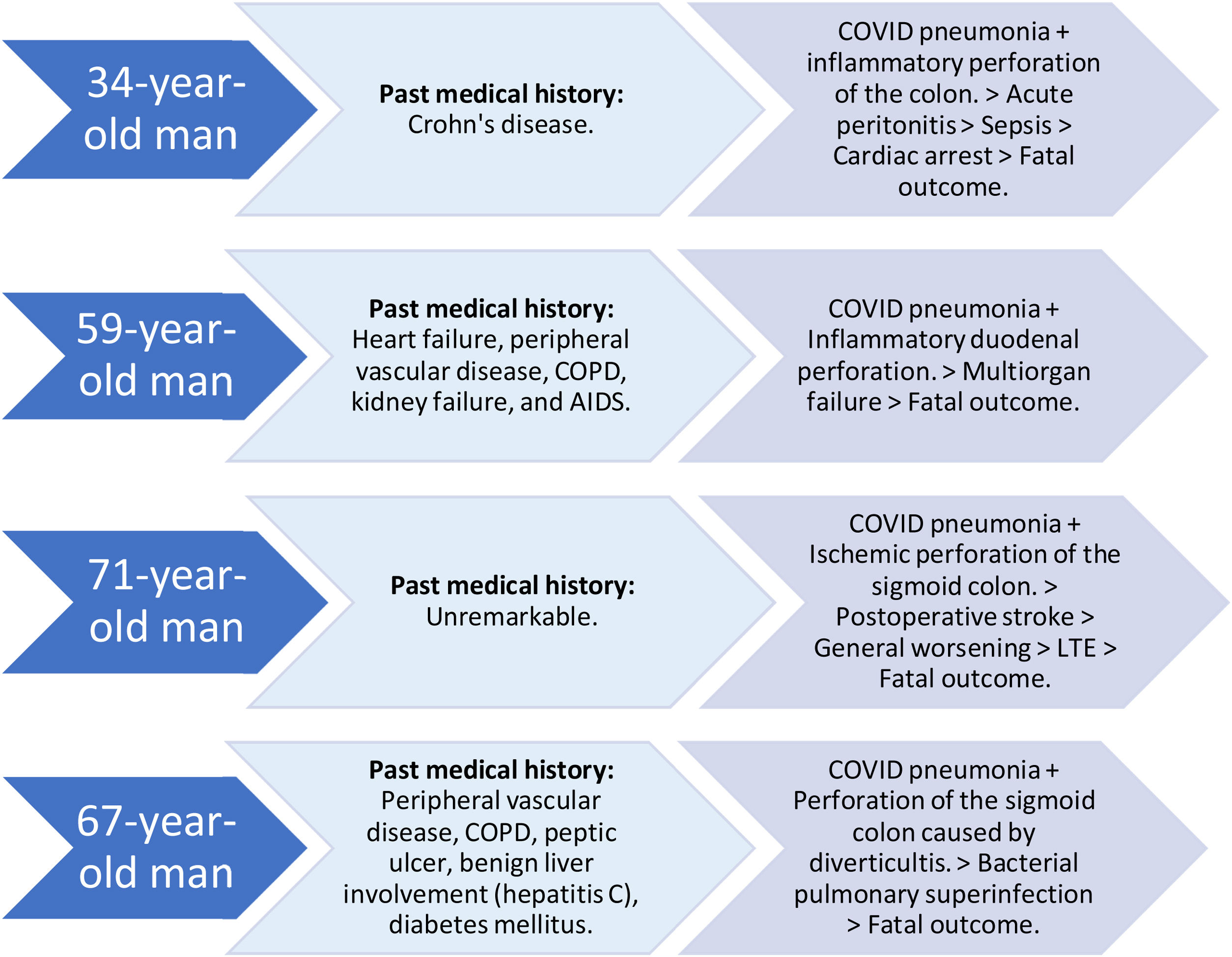
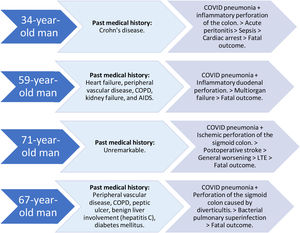
During the pandemic period, 4 (11.8%) of the patients operated on for gastrointestinal perforation were infected with COVID-19 (Fig. 3).
Profile, past medical history, and progression of COVID-19-positive patients with gastrointestinal perforation in the study period (01/09/2020 to 28/02/2021).
AIDS: acquired immunodeficiency syndrome; COPD: chronic obstructive pulmonary disease; LTE: limitation of the therapeutic effort.
The present study showed that there was an increase in cases of gastrointestinal perforation in our healthcare service area during the pandemic period of analysis. The advanced status of the patients upon arriving at the hospital, and a more torpid progression, resulted in greater mortality and longer hospital stays.
From September 1, 2020 to February 28, 2021, 345 emergency gastrointestinal surgeries were registered at our hospital center, a number that was similar to previous periods at the beginning of the pandemic. Our results differ from those of other studies, in which the number of emergency interventions during the pandemic period was lower.12,15,16 The recommendation to stay at home, fear of contagion, lifestyle changes, and a lower percentage of reinterventions could be among the causes justifying that trend.17,18 In our area, that decrease was compensated by an increase in the floating population. The exit of the United Kingdom from the European Union, the increase in online work, and the exodus from the large cities to second places of residence could be the reason for the increase we saw during the pandemic, in the number of cases of gastrointestinal perforation in foreign and non-resident patients.
There were twice as many gastrointestinal perforations during the pandemic period than cases registered in previous periods, and both the perforation rate per emergency intervention and the mortality rate per perforations indicate that, in our healthcare service area, the probability of presenting with a gastrointestinal perforation, and dying from it, was four-times higher in the pandemic period. In studies conducted in Austria, the United Kingdom, and Turkey, an increase in the cases of gastrointestinal perforation during the pandemic was reported, albeit the increase was not as significant as ours.9,10,16
The delay in the time the patient with perforation arrived at the emergency room until the surgery was started was 4.5hours longer in the pandemic period, most likely due to the organizational changes introduced in the care circuits, PCR screening for COVID-19 detection, personnel protection measures, etc. Although the delay can appear to have had little relevance, it was actually crucial in the progression and prognosis of those patients, especially if we take into account the fact that, in the pandemic period, they arrived at the emergency service with greater symptom progression.8,18
During the pandemic, 19% fewer patients with gastrointestinal perforation were admitted to the ICU due to the lack of bed availability as a consequence of the high use by COVID-19 patients. The patients that were admitted to the unit remained there for 137hours more than those admitted for the same reason in the pre-pandemic period. Likewise, mean hospital stay was 5 days longer for the group admitted during the pandemic, despite the early discharge policy to make more beds available and reduce the risk of contagion. That reinforces the idea that the more severe symptoms in the pandemic period resulted in a longer recovery time. The generalized perception among our healthcare personnel that delayed care led to worse treatment results in the patients that arrived at the emergency room during the pandemic was not supported by data from other studies.19
In general terms, comorbidity and surgical risk were similar in the two periods. Importantly, there was a higher percentage of BUPA 4 and 5 in the pre-pandemic period, which could imply the need for more aggressive interventions versus more conservative ones in the pandemic period, as well as the presence of more patients with ASA 4 in the pandemic period, suggestive of a worse general status and higher anesthetic risk.
Upon comparing the perforation sites in the two periods, no statistically significant differences were found, but clinically, there was a higher number of perforations in the large intestine in the pandemic period. Large bowel perforations tended to have a greater degree of association with oncologic disease. A possible explanation of that increase could be related to the suspension of consultations and non-urgent complementary tests that affected the screening and detection of cancer at early disease phases, resulting in patients going to the emergency room once symptoms had worsened or there were complications.10 The exacerbation of ulcer disease related to alcohol or tobacco abuse is one of the events that can give rise to gastric perforations. Even though some researchers reported that there were changes in the consumption habits of those substances during the pandemic, we could not establish a link between those findings and the results of our study.20,21
Only four (11.8%) of the patients operated on for gastrointestinal perforation during the pandemic were infected with COVID-19 (confirmed by nasopharyngeal PCR test). All of them spent time in the ICU and all of them died. Although the degree to which each disease contributed to death cannot be determined, the fact that COVID-19-positive patients presented with higher morbidity and mortality was confirmed.7,22
Despite the limitations inherent in our study’s single-center sample and retrospective data collection, its statistical power enabled clinically relevant differences to be found, regarding the impact of the pandemic on morbidity and mortality in the profile of events. In addition, the exhaustive digital clinical history archive available at our center made it possible to have unified information that was easily accessed.
Future multicenter studies conducted at hospitals of different levels of care that serve populations with different sociodemographic environments could be carried out to determine the impact of the pandemic on a wider range of settings.
In conclusion, during the COVID-19 pandemic, there was an increase in the incidence of gastrointestinal perforations in our healthcare system area. The patients presented with more severe symptoms, requiring greater care, and had a higher mortality rate. The pandemic has dramatically affected us all, but it is essential to study how it has affected the different areas of our healthcare system, to be able to efficiently manage our resources in this pandemic, as well as in future ones.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Mudarra Vela AM, Rivas Ruiz F, Atienza Carrasco J, Medina Cano FJ. Impacto en la incidencia de perforación gastrointestinal durante la pandemia de COVID-19 en el área sanitaria Costa del Sol. Revista de Gastroenterología de México. 2023;88:354–360.