There is conflicting evidence regarding the benefit of urgent esophagogastroduodenoscopy (EGD) for reducing mortality and rebleeding, in the context of nonvariceal upper gastrointestinal bleeding.
AimTo describe the decrease in the risk for mortality, rebleeding, and red blood cell transfusion, with the performance of urgent EGD, in patients with nonvariceal upper gastrointestinal bleeding.
Materials and methodsWe carried out a search for cohort studies or controlled clinical trials, published from December 1966 to May 2020, that compared urgent EGD versus elective EGD in the management of adults with nonvariceal upper gastrointestinal bleeding, utilizing the MEDLINE, Embase, LILACS, and Cochrane Central Register of Controlled Trials databases. Our primary outcome was the hospital mortality comparison. The incidence of rebleeding and the mean number of red blood cell units transfused were also compared. A random effects model was utilized for the meta-analysis.
ResultsTwenty-one studies that met the eligibility criteria were included, involving 489,622 patients. We found no differences in the mortality of subjects exposed to urgent EGD versus elective EGD (RR 1.12 [0.72-1.72]). There was a significant increase in the risk for rebleeding (RR 1.30 [1.05-1.60]) in the subjects exposed to urgent EGD, and fewer red blood cell units were transfused in those patients (RR 0.52 [0.05-0.99]).
ConclusionsUrgent EGD in subjects with nonvariceal upper gastrointestinal bleeding does not appear to have a significant impact on short-term mortality.
Existen discrepancias en relación al beneficio de la esofagogastroduodenoscopía de urgencia para disminuir la mortalidad y el resangrado en el contexto de la hemorragia de tubo digestivo alto no variceal.
ObjetivoDescribir la reducción en el riesgo de la mortalidad, el resangrado y la transfusión de glóbulos rojos de la esofagogastroduodenoscopía urgente en la hemorragia de tubo digestivo alto no variceal.
Materiales y métodosBuscamos estudios de cohorte o ensayos clínicos controlados que comparasen la esofagogastroduodenoscopía de urgencia versus la esofagogastroduodenoscopía electiva en el manejo de sujetos adultos con hemorragia de tubo digestivo alto no variceal. Los estudios fueron identificados usando MEDLINE, Embase, LILACS y el Cochrane Register of Controlled Trials desde diciembre de 1966 hasta mayo de 2020. Nuestro desenlace primario fue la comparación de la mortalidad hospitalaria. Se compararon la incidencia de resangrado y el promedio de unidades de glóbulos rojos transfundidas. Para el meta-análisis, se utilizó un modelo de efectos aleatorios.
ResultadosSe incluyeron 21 estudios que cumplieron con los criterios de elegibilidad y que involucraron 489,622 pacientes. No encontramos diferencias en la mortalidad de sujetos expuestos a esofagogastroduodenoscopía de urgencia versus electiva [RR 1.12 (0.72-1.72)]. Identificamos un incremento significativo del riesgo para resangrado [RR 1.30 (1.05-1.60)] y un menor número de unidades de glóbulos rojos transfundidas en sujetos expuestos a esofagogastroduodenoscopía de urgencia [RR 0.52 (0.05-0.99)].
ConclusionesLa esofagogastroduodenoscopía urgente en sujetos con hemorragia de tubo digestivo alto no variceal no impresiona tener un impacto significativo en la mortalidad a corto plazo.
Nonvariceal upper gastrointestinal bleeding (NVUGIB) is the most prevalent gastrointestinal emergency in the hospital environment.1 NVUGIB management has improved over the past few decades, thanks to the introduction of faster and more effective diagnostic and therapeutic elements, such as the administration of proton pump inhibitors,2 the advent of esophagogastroduodenoscopy (EGD) with different types of endoscopic hemostatic treatments,3 and the establishment of eradication treatment of Helicobacter pylori – a bacterium closely linked to the development of peptic ulcer.4
Despite those advances, the morbidity and mortality due to NVUGIB is not insignificant, even in advanced specialty hospitals.5,6 Therefore, efforts made to identify diagnostic and therapeutic elements that can reduce the morbidity and mortality in those patients are currently extremely relevant.
EGD performed on the patient with NVUGIB after his/her hospital admission potentially enables the identification and consequent treatment of lesions that significantly increase the risk for recurrent bleeding. Said intervention has been shown to reduce the risk for rebleeding and the need for surgical treatment.7 An international consensus by the Asia-Pacific working group recommends the performance of EGD in those patients, within the first 24 h of their hospital admission.8 Nevertheless, current evidence fails to clearly show whether the performance of that endoscopic procedure within that suggested time interval is clinically beneficial. Some controlled clinical trials have failed to demonstrate a reduction in hospital mortality or short-term mortality in patients with NVUGIB that underwent urgent EGD within 6 or 12 h from emergency room admission.9 Other cohort studies have reported contradictory results: some fail to identify a modification in the risk for death or rebleeding, according to the time the EGD was carried out,10 whereas others describe an increased risk for death if the EGD is performed after 6 h from patient admission.11
A clinical trial was recently published, describing the time to EGD in subjects admitted for upper gastrointestinal bleeding, that failed to show a reduction in the mortality rate in patients that underwent EGD in fewer than 6 h from hospital admission.12 The latest systematic review was published in 2001.13 Given the conflicting evidence in the previously published studies, as well as the lack of a recent systematic review, we decided to conduct a systematic review, with a meta-analysis, to determine whether urgent endoscopic intervention could reduce the risk for mortality and rebleeding, compared with elective EGD, in subjects with NVUGIB.
Our aim was to describe the risk for mortality, rebleeding, and red blood cell transfusion, in relation to urgent EGD in cases of NVUGIB.
Materials and methodsThe protocol of our systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO http://www.crd.york.ac.uk/prospero). We followed the recommendations of how to report a systematic review, described in the Cochrane Handbook, MOOSE proposal, and PRISMA.
Eligibility criteriaWe carried out a search for clinical trials (randomized and non-randomized) or cohort studies (prospective or retrospective) that involved adult subjects diagnosed with NVUGIB (or suspected of presenting with it) and compared urgent EGD versus elective (or non-urgent) EGD, as the initial management of those patients. Studies were included that defined NVUGIB, according to the following criteria: a) the presence of melena or b) the presence of hematochezia or c) the presence of hematemesis and d) the absence of esophageal and/or gastric varices in the EGD.
No language restrictions were applied. We excluded the studies that exclusively evaluated cirrhotic patients with variceal upper gastrointestinal bleeding, considering them a different population, in relation to prognosis, treatment, and need for urgent EGD, in the context of gastrointestinal bleeding.
Definition of urgent esophagogastroduodenoscopy and outcomesOur primary objective was to compare the incidence of hospital mortality plus 30-day mortality from the bleeding event in patients exposed to urgent EGD versus those exposed to elective EGD. Urgent EGD was defined in hours from the hospital admission of each of the patients enrolled in the study. Heterogeneity was identified regarding the cutoff value of the hours that was utilized. The cutoff value was any hour less than or equal to the first 24 h of hospital admission.
In addition, the incidence of rebleeding was compared between subjects exposed to urgent EGD and those exposed to elective EGD, as well as the transfusion requirements during hospitalization, measured in mean transfused red blood cell units, in the two groups. The definition of rebleeding employed was the same as that utilized in studies evaluating said outcome: the persistence of symptoms consistent with upper gastrointestinal bleeding (melena or hematochezia or hematemesis) during the hospital stay of any patient that required a new EGD.
Bibliographic search strategyStudies published within the time frame of December 1966 and May 2020 were identified, utilizing the MEDLINE, Embase, LILACS, and Cochrane Register of Controlled Trials (CENTRAL) databases. Abstracts of works presented at the American Congress of Gastroenterology (Digestive Disease Week) over the last 4 years were also manually reviewed and included in the present study if, in addition to meeting the eligibility criteria described above, at least one of the outcomes to be evaluated was included.
The search algorithm employed included the following MeSH terms: [“endoscopy” OR “gastroscopy” OR “early medical intervention”] AND [“gastrointestinal hemorrhage” OR “peptic ulcer hemorrhage”] AND [“mortality” OR “treatment outcome” OR “hemorrhage”].
Data selection and extraction processThree authors, (GB, CS, JL), reviewed the titles of the abstracts identified in the bibliographic search, evaluated their relevance. The complete texts of the abstracts deemed relevant were read, to determine whether they met the inclusion criteria described above. The bibliographic citations of the articles selected were also reviewed.
The following data were collected from each study: age and sex of the subjects, mean hemoglobin level in blood at hospital admission, a history of oral anticoagulant use, and the number of cases of NVUGIB whose etiologic diagnosis was peptic ulcer. The time interval to EGD utilized in each study was recorded. When there were discrepancies between authors in the data extraction process, they were resolved through a consensus of the 3 authors mentioned above plus a fourth author (IZ). To evaluate the methodological quality of the studies included in the present review, the Evidence-based Gastroenterology Steering Group Recommendations14 and the Newcastle-Ottawa guidelines15 were used.
Statistical analysisThe Review Manager (RevMan version 5.3 Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014) was used for the statistical analysis. Study heterogeneity was evaluated using the chi-square test and the I2 statistic. A random effects model was utilized, enabling a more conservative approach to be taken, as well as allowing heterogeneity between studies. The outcomes were described as relative risks (RRs), with their corresponding 95% confidence intervals (95% CIs). Sensitivity analyses were performed, taking into account the different methodological designs of the studies, as well as the different time intervals utilized for defining urgent EGD. The possibility of publication bias was evaluated through the Egger test.
Ethical considerationsThe present study meets the current bioethical research regulations. Because it is a systematic review of already published studies, approval by an ethics committee at our institution was not required. All the authors pledged to carry out the ethical principles of clinical research included in the Declaration of Helsinki.
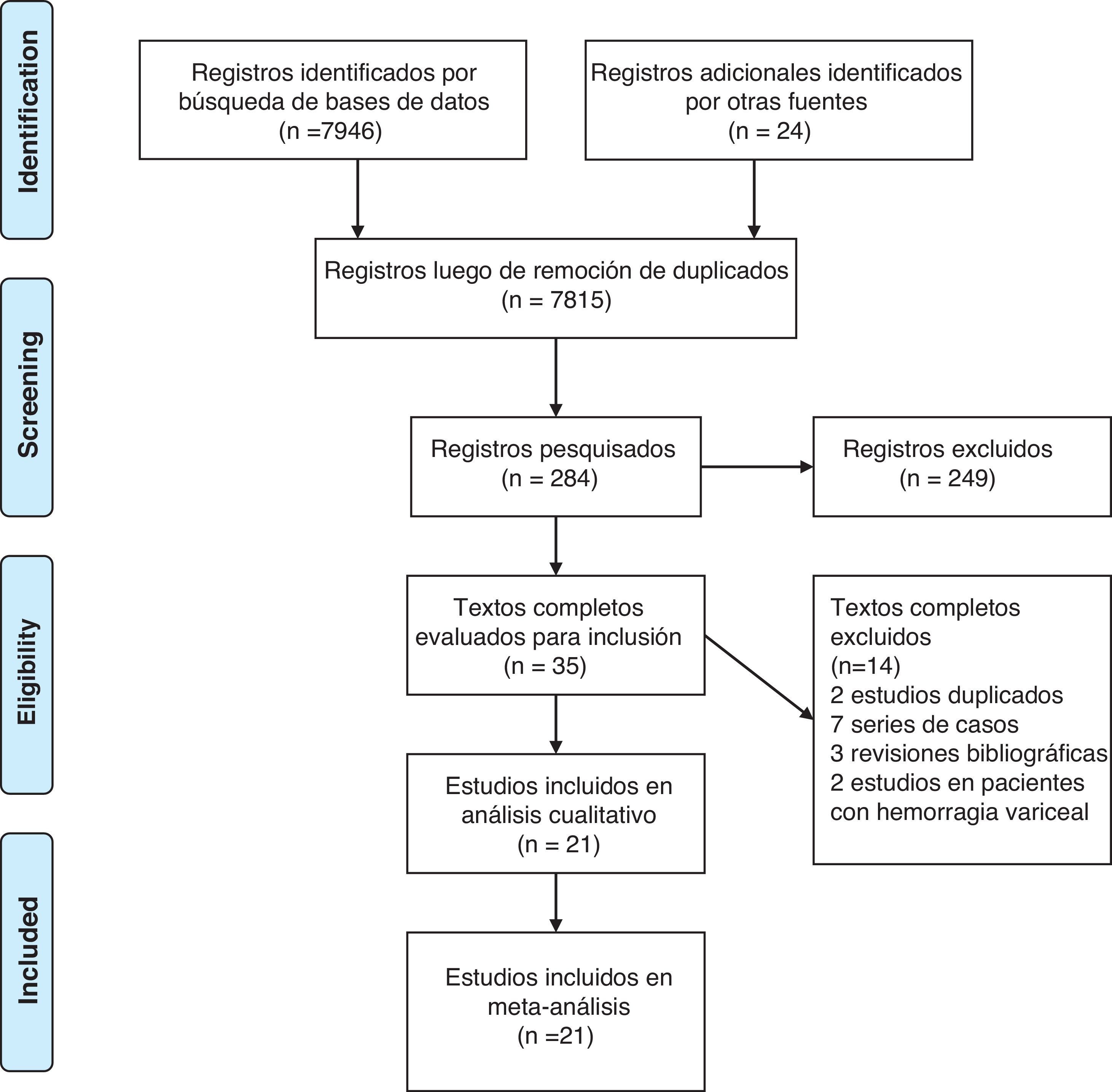
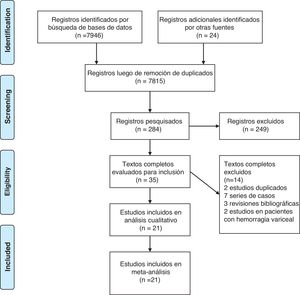
ResultsResults of the bibliographic searchThe search produced 7,970 records, from which a final 21 studies that met the eligibility criteria were included, as shown in Fig. 1.8–12,16–32 Of those studies, 5 were controlled clinical trials that involved 1,032 patients, and the remaining analyses were cohort studies, either prospective or retrospective, that included 488,590 patients with NVUGIB.
Table 1 summarizes the general characteristics of the studies included in the present review, showing the differences in the clinical characteristics of the subjects in each study, especially regarding the number of patients in whom peptic ulcer was the underlying cause of bleeding. The evaluation of the methodological quality of the studies did not produce high probabilities of bias (tables 2 and 3) and we found no significant publication bias (Egger test p > 0.05).
Characteristics of the studies included in the systematic review.
| Study author | Country | Number of patients | Male patients (%) | Mean age | Mean hemoglobin at admission (g/dl) | OAC use (%) | Patients with peptic ulcer (%) | Definition of urgent EGD (hours) |
|---|---|---|---|---|---|---|---|---|
| Randomized controlled trials | ||||||||
| Bjorkman et al.,9 2004 | USA | 93 | 66.66 | 54.50 | 14.10 | NR | 65.59 | < 6 |
| Lau et al.,12 2020 | Hong Kong | 516 | 62.98 | 70.50 | 7.30 | 3.29 | 61.43 | < 6 |
| Lee et al.,11 1999 | USA | 110 | 71.81 | 49 | 12 | NR | 47.27 | < 2 |
| Lin et al.23 1996 | Taiwan | 107 | 89.72 | 66.40 | 9.90 | NR | NR | < 12 |
| Peterson et al.,24 1981 | USA | 206 | NR | 55.10 | 11 | NR | 19.41 | < 4 |
| Cohort studies | ||||||||
| Ahn et al.25 2016 | Korea | 158 | 72.15 | 60.10 | 10.10 | NR | 64.55 | < 12 |
| Alexandrino et al.26 2019 | Portugal | 102 | 75.50 | 67 | 9.20 | 8.82 | NR | < 12 |
| Cho et al.,18 2009 | Korea | 90 | 78.90 | 57.40 | NR | NR | 100 | < 24 |
| Cho et al.10 2018 | Korea | 961 | 81 | 57 | 9.80 | 32.30 | 70.75 | < 6 |
| Cooper et al.19 1999 | USA | 909 | 54 | 66 | NR | NR | 55 | < 24 |
| Iqbal et al.,27 2018 | USA | 179 | 40 | 70 | 9.60 | NR | NR | < 24 |
| Jairath et al.,20 2012 | The United Kingdom | 4,182 | 60 | 65.80 | 10.50 | 8.20 | NR | < 24 |
| Kalla et al.,21 2019 | The United Kingdom | 133 | 65 | 65 | NR | NR | NR | <24 |
| Kim et al.,17 2018 | Korea | 253 | 63.24 | 68.40 | NR | 23.71 | 34.78 | < 24 |
| Kumar et al.,28 2017 | USA | 361 | 53.74 | 63.50 | NR | 19.66 | NR | < 12 |
| Laursen et al.,29 2016 | Denmark | 8,369 | 54.76 | 73.40 | 8.70 | 15.33 | 100 | < 24 |
| Saleem et al.,30 2020 | USA | 249 | 60.55 | NR | NR | NR | NR | < 12 |
| Sarin et al.,31 2009 | Canada | 502 | 54 | 67 | 9.10 | 29.50 | NR | < 24 |
| Siau et al.,22 2019 | The United Kingdom | 348 | 61 | 70 | NR | NR | 23,85 | < 24 |
| Wierzchowski et al.,32 2013 | Poland | 482 | NR | 62.70 | 9.20 | NR | 26.50 | < 3 |
| Wysocki et al.,16 2012 | USA | 471,512 | 66.30 | 55.30 | NR | NR | NR | < 24 |
EGD: esophagogastroduodenoscopy; NR: not reported; OAC: oral anticoagulants.
Methodological characteristics of the randomized controlled trials included in the analysis.
| Study author | Masked and randomized allocation to the intervention | Patients and treating physicians blinded | Similar cointerventions between groups | Complete follow-up | Intention-to-treat analysis |
|---|---|---|---|---|---|
| Bjorkman et al.,9 2004 | Yes | No | Yes | Yes | Yes |
| Lau et al.,12 2020 | Yes | No | Yes | Yes | Yes |
| Lee et al.,11 1999 | Yes | No | Yes | Yes | Not reported |
| Lin et al.,23 1996 | Yes | No | Yes | Yes | Not reported |
| Peterson et al.,24 1981 | Yes | No | No | Yes | Not reported |
Methodological characteristics of the cohort studies included in the analysis.
| Study author | Representativity of the cohort exposed | Cohort not exposed | Outcome not present at the beginning of the study | Cohort comparability | Adequate follow-up | Sufficient follow-up duration | Prospective/retrospective |
|---|---|---|---|---|---|---|---|
| Ahn et al.,25 2016 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Alexandrino et al.,26 2019 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Cho et al.,18 2009 | Representative | Same community | Yes | Yes | Yes | Yes | Prospective |
| Cho et al.,10 2018 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Cooper et al.,19 1999 | Representative | Same community | Yes | Yes | Yes | Yes | Prospective |
| Iqbal et al.,27 2018 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Jairath et al.,20 2012 | Representative | Same community | Yes | Yes | Yes | Yes | Prospective |
| Kalla et al.,21 2019 | Representative | Same community | Yes | Yes | Yes | Yes | Prospective |
| Kim et al.,17 2018 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Kumar et al.,28 2017 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Laursen et al.,29 2016 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Saleem et al.,30 2020 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Sarin et al.,31 2009 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
| Siau et al.,22 2019 | Representative | Same community | Yes | Yes | Yes | Yes | Prospective |
| Wierzchowski et al.,32 2013 | Representative | Same community | Yes | Unclear | Yes | Yes | Retrospective |
| Wysocki et al.,16 2012 | Representative | Same community | Yes | Yes | Yes | Yes | Retrospective |
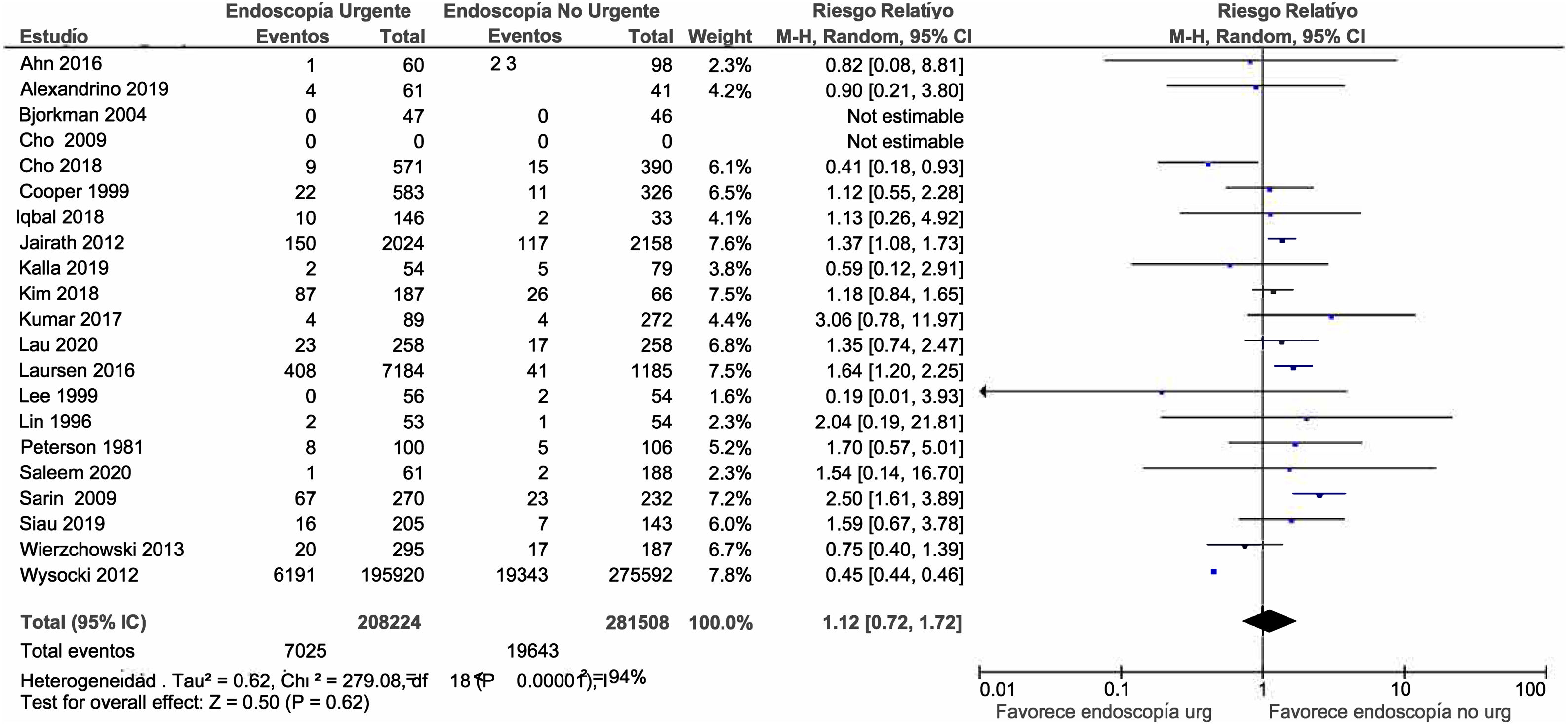
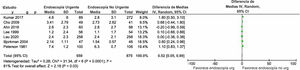
Twenty-one studies were included that reported data on mortality, with a total of 489,732 patients. In the overall analysis of that outcome, as shown in Fig. 2, we found no increased risk for hospital death and/or death within 30 days, in subjects exposed to urgent EGD versus elective EGD (RR 1.12; 0.72-1.72). That remained unaltered when exclusively taking clinical trials into account (RR 2.26; 0.32-16.22), or when separately considering cohort studies. However, in the cohort study sensitivity analysis, when the study by Wysocki et al.16 was excluded, the RR for mortality in subjects exposed to urgent EGD was 1.26 (1-1.61). Said study was excluded because its results were completely contradictory to those of the other cohort studies included in the review.
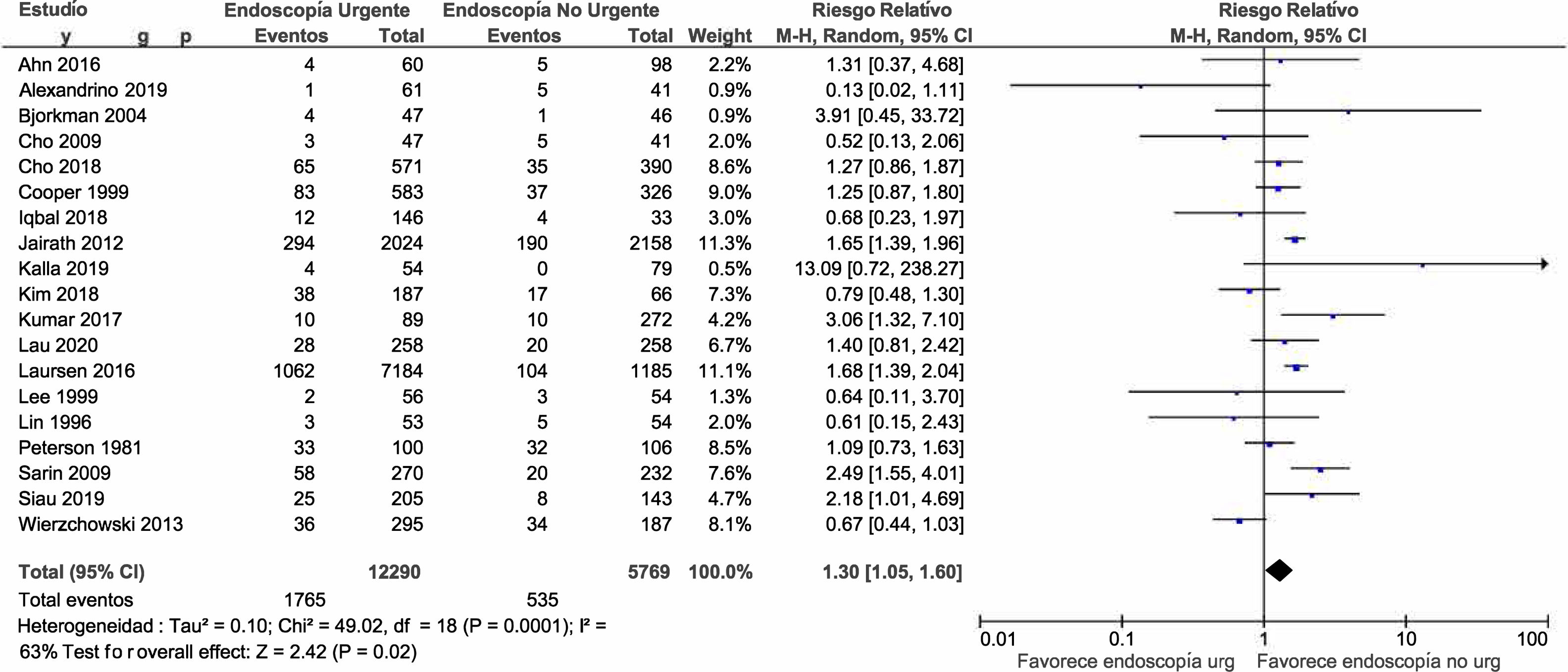
RebleedingNineteen studies were included that described data on rebleeding, with a total of 18,059 patients. The overall analysis of that outcome showed a significant increase in the risk for rebleeding in subjects exposed to urgent EGD (RR 1.30; 1.05-1.60) (Fig. 3). That finding was a reflection of the increased risk observed in the cohort studies, given that, in the separate analysis of clinical trials, the risk for rebleeding was similar in the patients exposed to urgent EGD versus those exposed to elective EGD (RR 1.16; 0.85-1.58).
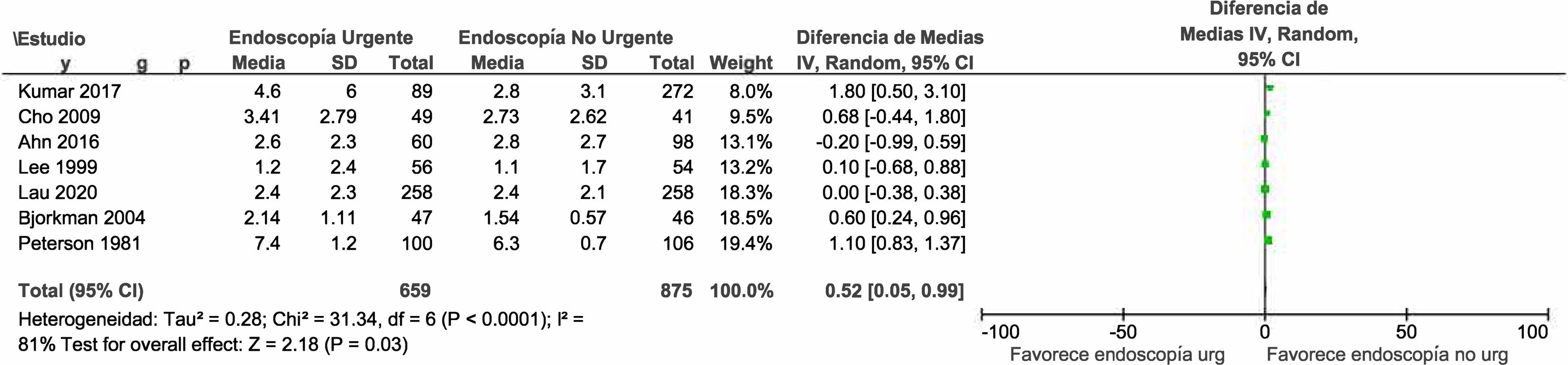
Red blood cell transfusionOnly 7 studies reported the mean number of red blood cell units transfused during the hospitalization of a total of 1,534 patients with NVUGIB. A reduced risk for red blood cell transfusion was observed in the subjects exposed to urgent EGD (RR 0.52; 0.05-0.99) (Fig. 4).
Discussion and conclusionAccording to our findings, there was no significant difference in relation to short-term mortality in subjects hospitalized due to NVUGIB, whether or not they underwent urgent EGD. However, there was an overall difference in the risk for rebleeding, even though the performance of urgent EGD significantly reduced the need for red blood cell transfusion.
To clearly explain our findings in relation to mortality, the differences in the methodologies of the studies analyzed must be emphasized. Even though the interval of time utilized to define urgent EGD varied among the randomized clinical trials, the comparison carried out in the present study was as free as possible from possible confounders and showed no significant difference in mortality between the subjects that underwent urgent EGD and those that underwent elective EGD. In contrast, in our separate sensitivity analysis of the cohort studies, the risk for mortality was increased in the subjects exposed to urgent EGD. Most likely, that discrepancy is due to the fact that certain residual confounding factors cannot be avoided in cohort studies. In fact, patients that undergo urgent EGD clinically present with some kind of aggravating condition. Thus, their underlying condition per se, not the performance of urgent EGD, could increase the risk for mortality. Indeed, there are clinical variables that increase the risk of mortality during the hospitalization of patients with NVUGIB that were not taken into account in the majority of the studies evaluated in the present systematic review. In a study by González-González,33 there was a 10.2% mortality rate in patients with NVUGIB, but only 3.1% of those cases were directly associated with bleeding. Moreover, the number of comorbidities and albuminemia upon admission (among other variables) were significantly associated with mortality. Such a patient is already at higher risk for mortality, when he/she undergoes EGD, and so the urgency of the EGD cannot be determined as the factor having a detrimental effect on that patient’s outcome. Even though it is difficult to calculate the protective effect of EGD in the context of NVUGIB, population cohort studies, such as the one by Kohn et al.,34 showed that access to EGD and NVUGIB managed by specialists were variables that significantly reduced the risk for mortality in patients hospitalized due to NVUGIB.
With respect to rebleeding, something similar to the mortality results occurred. When exclusively considering the randomized clinical trials, there was no difference in the risk for rebleeding between the subjects exposed to urgent EGD and those exposed to elective EGD. Nevertheless, in the cohort studies, urgent EGD was significantly associated with a higher risk of rebleeding. Numerous clinical variables could contribute to the risk for rebleeding in the context of NVUGIB. Travis et al.35 found that active bleeding at the time of EGD, as well as the type of hemostatic treatment employed or the use of low-molecular-weight heparin, among other variables, increased the risk for rebleeding in patients with NVUGIB, during their hospitalization. Those variables were not contemplated in the majority of the cohort studies, and so their unequal distribution could partially explain the finding of the increased risk in one group versus the other. Likewise, the risk for rebleeding in the case of peptic ulcer lesions is associated with the presence or absence of active bleeding, at the time of examination. The bleeding activity classification described by Forrest et al.36 is the most frequently used, but it was largely absent in the studies included in our review, which could explain the conflicting results observed in the risk for rebleeding in the cohort studies.
Even though fewer studies described the outcome of number of transfused red blood cell units, we found that urgent EGD was significantly associated with a lower number of units per patient. In recent years, controlled randomized clinical trials, such as the study by Villanueva et al.,37 have shown that a conservative strategy of red blood cell transfusion has a positive impact on the progression of patients hospitalized due to gastrointestinal bleeding, in general, making the number of transfused red blood cell units a relevant outcome that should be observed in patients with NVUGIB. A shorter time interval from patient admission to the performance of EGD (and eventual hemostatic therapy) should stop gastrointestinal bleeding early, and in turn, reduce total blood loss, which could explain the association observed in our meta-analysis. The length of hospital stay is another similar outcome, but given the relative scarcity of studies that evaluate it, we did not include it in our analysis. As demonstrated by Lee et al.11 hospital stay was significantly shorter in subjects that had urgent EGD, compared with those that had elective EGD. If, as shown in our study, the 2 procedures have a similar incidence of mortality, then urgent EGD becomes relevant, with respect to reducing the use of hospital resources that significantly increase the cost of healthcare in patients with NVUGIB.
The present systematic review has limitations that must be addressed. First, there are relatively few controlled clinical trials in our review, and more such studies are needed to reach the best quality conclusions possible. In addition, the heterogeneity in the definitions of urgent EGD is striking, given that the performance of EGD ranged from 2 h to 24 h after hospital admission. Even though the separate analyses of the cohort studies and clinical trials resulted in a more homogeneous definition, it reflects the relative lack of consensus in determining the cutoff interval for establishing a specific description. No distinction was made in any of the studies included in the review, regarding the manner in which NVUGIB appeared (i.e., the presence of melena, hematochezia, or hematemesis) and its impact on the outcomes, nor were the risk factors related to NVUGIB described, such as finding an actively bleeding lesion at the time of EGD. There were not enough details in the studies analyzed to carry out a meta-regression analysis to determine the effect of variables, such as age or hemoglobin level upon admission, on the outcomes studied.
In conclusion, the performance of urgent EGD in subjects hospitalized due to NVUGIB did not have a significant impact on all-cause mortality, in the short term. The clinical trials failed to demonstrate a significant difference in the risk for rebleeding, but when the cohort studies were added, the incidence of rebleeding was higher in the subjects that underwent urgent EGD. More evidence of higher quality is needed to determine the true impact of urgent EGD on the risk for those relevant clinical variables.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Bilder HG, Soccini C, Lasa JS, Zubiaurre I. Impacto del tiempo a la endoscopia digestiva en pacientes con hemorragia de tubo digestivo alto no variceal: una revisión sistemática y metaanálisis. Rev Gastroenterol Méx. 2022;87:320–329.