Liver disease is currently one of the leading causes of death in older adults and the only option deemed curative is liver transplantation. However, it is uncertain whether the successful results obtained in older adults that receive a liver transplant in developed countries can be replicated in developing countries.
AimTo determine if there are differences in the survival time between older (≥60 years) and younger adults that underwent liver transplantation at a university-affiliated tertiary care center in Mexico City.
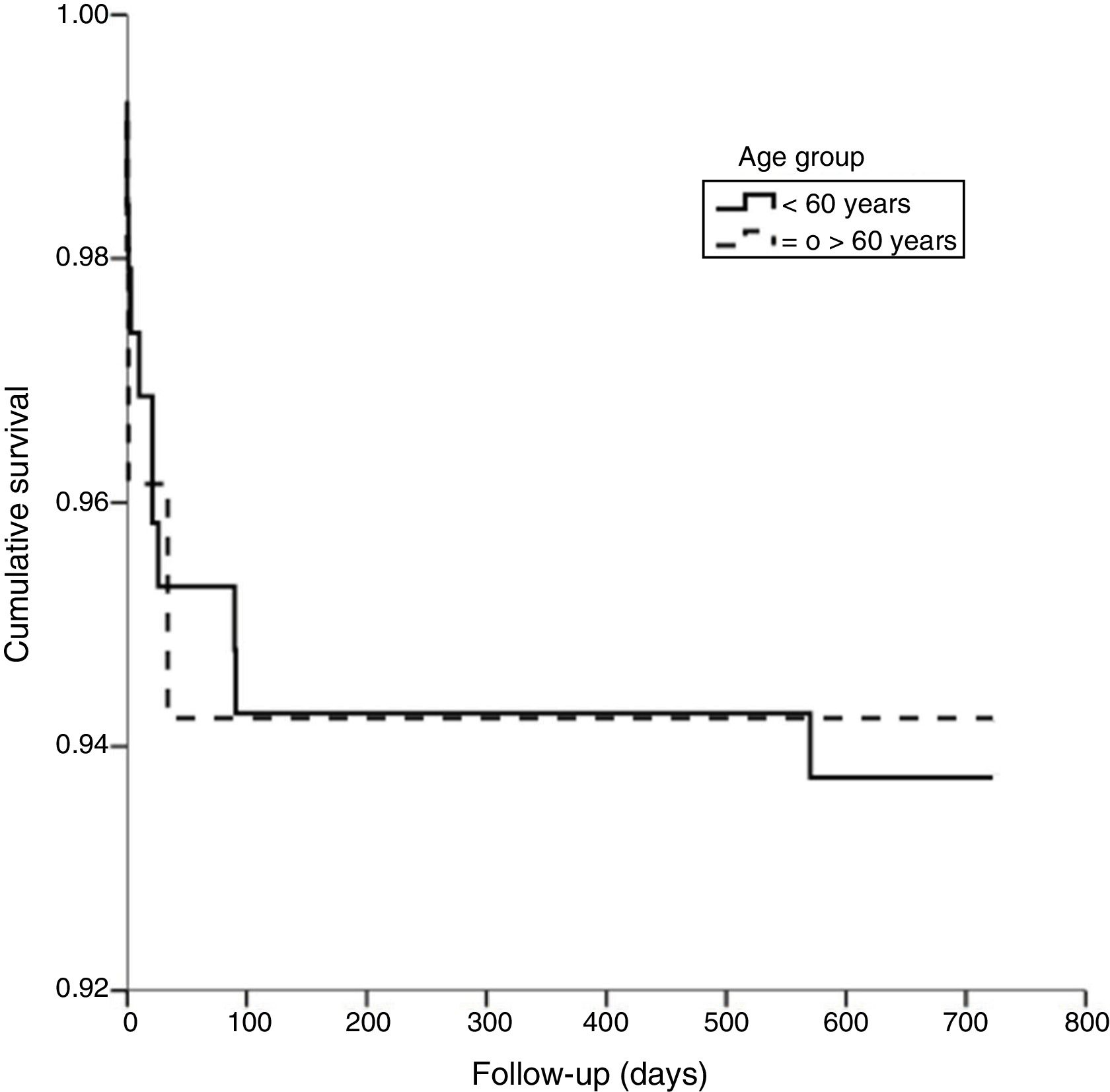
Materials and methodsA 2-year longitudinal study was conducted. It included 244 participants that were divided into 2 groups according to age at the time of transplantation: older adults (≥60 years) and younger adults (18–59 years). Survival time was defined as the number of days that elapsed between transplantation and death. Survival was expressed as Kaplan-Meier curves.
ResultsMedian age in the older adults (n=52) was 63.0 (IQR=60–69) and 23 participants were females (44.2%). In the younger adults (n=196) median age was 47.0 (IQR=16–59) and 104 were females (52%). The leading indication for transplant was hepatitis C virus. After the follow-up, fifteen participants died (twelve younger adults and three older adults). No significant differences were observed between older and younger participants in postoperative complications, the number of re-admissions, or mean post-transplantation survival time.
ConclusionsThere were no statistically significant differences in relation to survival times between older and younger adults that received a liver transplant. Older patients in developing countries should not be excluded from the selection process due only to age.
Las enfermedades hepáticas son una causa importante de muerte en las personas adultas mayores y el trasplante de hígado suele ser la única opción curativa. Sin embargo, es incierto si los buenos resultados obtenidos en esta población trasplantada en países desarrollados pueden ser replicados en los países de economías emergentes.
ObjetivoDeterminar si hay una diferencia en la sobrevida de adultos mayores (≥60 años) y adultos jóvenes sometidos a trasplante hepático en un hospital universitario de tercer nivel en la Ciudad de México.
Material y métodosEstudio longitudinal de 244 personas con dos años de seguimiento, los cuales fueron divididos por edad al momento del trasplante: adultos mayores y jóvenes. La sobrevida se definió como el número de días ocurridos entre trasplante y muerte. Esta se analizó mediante curvas de Kaplan-Meier.
ResultadosEl promedio de edad en los adultos mayores (n=52) fue 63.0 (RIC=60–69) y 23 participantes fueron mujeres (44.2%). En los adultos jóvenes (n=196), el promedio de edad fue 47.0 (RIC=16–59) y 104 fueron mujeres (52%). La principal indicación para trasplante fue infección por virus C. Durante el seguimiento, 15 personas murieron (doce adultos jóvenes y tres adultos mayores). No hubo diferencia estadísticamente significativa entre los grupos con respecto a la frecuencia de complicaciones posoperatorias, número de reingresos hospitalarios o sobrevida postrasplante.
ConclusionesNo hay diferencia en la sobrevida entre los adultos mayores y jóvenes que reciben un trasplante hepático. Los adultos mayores en los países de economías emergentes no deberían ser excluidos del proceso de selección para recibir este órgano sólo por el criterio de edad.
Liver disease, particularly cirrhosis, is currently one of the leading causes of death among older adults, as a result of the demographic transition that is taking place worldwide. In Western nations, chronic alcohol intake and infection with either hepatitis B virus or hepatitis C virus (HCV) are the main contributors to the development of cirrhosis, and the aging process is involved in the speed and intensity of liver fibrosis progression.1 The elevated mortality observed in cirrhotic patients is associated with the complications derived from that condition (e.g., hemorrhagic portal hypertension, encephalopathy, spontaneous bacterial peritonitis, etc.)2 and the only option deemed curative is liver transplantation. Acute liver failure and hepatocellular carcinoma are other indications for liver transplant.3
New developments in surgical techniques and immunosuppressive drugs have resulted in wider availability of liver transplantation and the benefits that such therapy offers an expanding population of patients, including individuals 60 years of age or older.4–8 Nonetheless, considering an older adult as a candidate for receiving a liver transplant may represent a clinical dilemma if the selection committee takes into account: 1) potential patient survival time, 2) potential graft survival time, 3) complications associated with the procedure, 4) prevalence of neoplastic disease in the elderly, 5) infectious complications due to immunosuppression, and 6) neurologic disturbances observed in that group of patients.9,10 Furthermore, characterizing chronologic age as an exclusion criterion for liver transplantation is controversial, and the cutoff point varies widely from center to center, ever since the concept of “physiologic age” was introduced into pre-transplantation assessment.11
The dilemma of transplanting livers into older adults is relatively new. Results from two reports that analyzed data from high-volume transplant centers in the United States and Europe11,12 show that perioperative complications, 1-year graft survival, 1-year patient survival, and overall survival in older adults are not statistically different from those observed in younger patients.12 However, the percentage of older adults awaiting transplantation can be <3% at some hospital centers. In Mexico, only 6.9% of patients on the liver transplant waiting list are older than 65 years of age,10 reflecting the underrepresentation of older adults in liver transplantation. Whether the good results observed in older adults that receive liver transplants in developed countries can be replicated in developing countries remains unclear, given the differences between their corresponding healthcare systems. For example, in our medical center, liver transplant protocol is adapted to our population from high-volume transplant centers.13 The main points of the protocol are:
- a)
Liver transplant candidates must be fit enough for the surgical procedure.
- b)
The patient must have a liver disease that is suitable for transplant.
- c)
Potential candidates must not have any contraindication for a transplant.
- 1)
General contraindications:
- -
Portal vein thrombosis that may limit the procedure, according to the surgeon’s criteria.
- -
Severe or uncontrolled extrahepatic comorbidities.
- -
HIV infection.
- -
≥70 years of age.
- -
Poor social support or a condition that limits access to post-transplant care.
- -
Decompensated liver disease associated with multiorgan failure or a poor survival estimate (expected 5-year survival <50%).
- -
- 2)
Specific contraindications:
- -
Active extrahepatic malignancy.
- -
Active alcohol intake.
- -
Other addictive behaviors (opioids, cocaine, cannabis).
- -
Hepatocellular carcinoma that does not fit the Milan criteria.
- -
Portopulmonary hypertension.
- -
Hepatopulmonary syndrome.
- -
- 1)
Adherence to those measures has apparently led to good clinical results in the transplanted patients. Nevertheless, it is imperative to determine if there is a difference in outcomes between older and younger transplant recipients in developing countries, so that older adults that can benefit from liver transplantation are not excluded. Therefore, the aim of the present study was to determine if there were differences in the survival time between older adults and younger patients that underwent liver transplantation at a referral center in Mexico City. The main hypothesis was that survival times after liver transplantation are similar in older adult and younger adult recipients.
Materials and methodsWe conducted a retrospective analysis on 244 patients, 18 years of age or older, that underwent orthotopic liver transplantation at a university-affiliated tertiary care center in Mexico City between January 2002 and December 2015. Participants were divided into two groups according to age at the time of transplantation: the older adult group (≥60 years) and the younger adult group (18–59 years). The category of “older adult” was established according to the Mexican national regulations. All transplant recipients that received follow-up care at other institutions were excluded from the study.
VariablesThe time of death and its cause were obtained from interviews with family or from medical records from the 2-year follow-up. Survival time was defined as the number of days that elapsed between transplantation and death (dependent variable).
Sociodemographic variables included age at the time of transplant and sex. Health-related variables included weight (kg), height (m), body mass index (BMI), the Model for End-Stage Liver Disease (MELD) score before transplantation, indication for transplant (defined as end-stage liver disease etiology), age of donor, time of surgery (hours), postoperative complications (defined as any post-surgical outcome outside of an uneventful postoperative period, such as myocardial infarction, graft loss, infection, death, etc.), number of re-admissions (defined as the number of non-elective re-admissions after transplantation), and re-admission causes (defined as the working diagnosis at the time of re-admission).
Statistical analysisFor the descriptive data, the continuous variables were presented as arithmetic median and interquartile range (IQR) and the categorical variables as frequencies (%). Nonparametric tests were used to perform the comparative analysis between the two groups, when appropriate. Two-year survival was expressed as Kaplan-Meier curves and the log-rank test was estimated. A p value of 0.05 or less was considered significant and the 95% confidence intervals (CIs) were provided. All analyses were performed using the Statistical Package for the Social Sciences version 17 for Windows® (SPSS Inc. Chicago IL). The present study was approved by the local ethics committee.
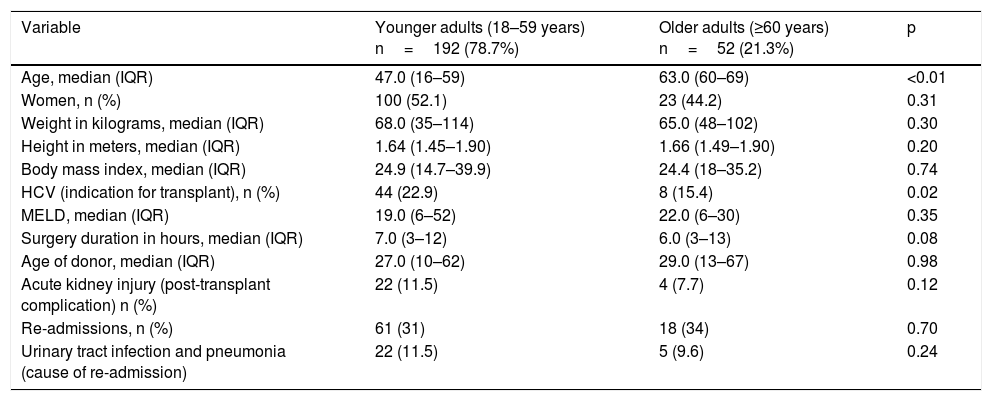
ResultsThe present study included 244 patients. A total of 196 (79%) were in the younger adult group and 52 (21%) were in the older adult group. The sociodemographic and health-related characteristics are presented in Table 1. Median age in the older adult group was 63.0 (IQR=60–69) and 23 of those patients were females (44.2%). In the younger adult group, median age was 47.0 (IQR=16–59) and 104 of those patients were females (52%). The leading indication for transplant in the younger adult group was HCV infection (22.9%), whereas there was no clearly predominant indication in the older adult group (hepatocellular carcinoma, HCV infection, nonalcoholic fatty liver disease, etc).
Participant characteristics at the time of transplantation.
| Variable | Younger adults (18–59 years) n=192 (78.7%) | Older adults (≥60 years) n=52 (21.3%) | p |
|---|---|---|---|
| Age, median (IQR) | 47.0 (16–59) | 63.0 (60–69) | <0.01 |
| Women, n (%) | 100 (52.1) | 23 (44.2) | 0.31 |
| Weight in kilograms, median (IQR) | 68.0 (35–114) | 65.0 (48–102) | 0.30 |
| Height in meters, median (IQR) | 1.64 (1.45–1.90) | 1.66 (1.49–1.90) | 0.20 |
| Body mass index, median (IQR) | 24.9 (14.7–39.9) | 24.4 (18–35.2) | 0.74 |
| HCV (indication for transplant), n (%) | 44 (22.9) | 8 (15.4) | 0.02 |
| MELD, median (IQR) | 19.0 (6–52) | 22.0 (6–30) | 0.35 |
| Surgery duration in hours, median (IQR) | 7.0 (3–12) | 6.0 (3–13) | 0.08 |
| Age of donor, median (IQR) | 27.0 (10–62) | 29.0 (13–67) | 0.98 |
| Acute kidney injury (post-transplant complication) n (%) | 22 (11.5) | 4 (7.7) | 0.12 |
| Re-admissions, n (%) | 61 (31) | 18 (34) | 0.70 |
| Urinary tract infection and pneumonia (cause of re-admission) | 22 (11.5) | 5 (9.6) | 0.24 |
HCV: hepatitis C virus; IQR: inter-quartile range; MELD: Model for End-Stage Liver Disease.
The comparative analysis between groups is also presented in Table 1. The leading postoperative complication was acute kidney injury (AKI) in both groups, and no statistical difference was observed when comparing its frequency in the younger vs. the older patients (11.4 vs. 7.7%, respectively, p=0.12). Moreover, there was no statistically significant difference in the number of re-admissions between groups or in the re-admission causes, of which infectious diseases (more frequently urinary tract infection and pneumonia) were the main causes (11.4% in the younger adults vs. 9.6% in the older adults, p=0.24).
During the 2-year follow-up, there were 15 deaths (3 in the older adult group [5.8%] and 15 in the younger adult group [6.3%]), with no statistical difference (p=0.98) (Fig. 1). No graft loss was reported during that period.
Discussion and conclusionThe results of the present study did not show any statistical difference regarding survival times after transplantation between older adults and younger adults during the 2-year follow-up period. That finding supports the initial hypothesis that age at the time of diagnosis is not associated with survival prognosis when patients are carefully selected for transplantation. Those results partially replicate the findings from similar studies conducted in various countries. In one of the largest single-center cohorts, Aduen et al.14 analyzed diverse outcomes after a 5-year follow-up period in 42 post-liver transplant patients that were ≥70 years of age and compared them with 42 controls aged 60 years or younger. That study did not find a significant increase in post-transplant mortality (RR=1.00, 95% CI: 0.43–2.31; p>0.99), graft loss rates (RR 1.17, 95% CI: 0.54–2.52; p=0.70), or in the frequency of perioperative complications (infections, mechanical complications from the surgical procedure, etc.). In the largest series on that topic, data derived from the Scientific Registry of Transplant Recipients and the University Health System Consortium of the United States showed no statistical significance when comparing older liver transplant recipients with their younger counterparts in relation to: 1) length of hospital stay, 2) graft survival time, or 3) overall survival during 5-year follow-up.15 It is possible that the similar survival times in younger and older liver transplant recipients stem from the rigorous, standardized protocols utilized to select potential candidates, as opposed to simply the age of the potential recipient. Such protocols consider aspects that include the patient’s support network, as well as the availability of immunosuppressive drugs and medical follow-up after transplantation.16 In the same vein, studies comparing younger vs. older patients have not found significant differences in the leading causes of complications in the postoperative period (e.g., AKI or infections). That is important, since it could be assumed that the lower physiologic reserve of older individuals negatively impacts the tolerance of the hemodynamic derangements that occur during and after the surgical procedure, or of the drugs required during and after hospitalization.17,18
The proportion of older adults receiving a liver transplant at our center (21%) is higher than that in other reports, whose ranges vary from 5 to 15%.19,20 Such findings may be the result of the meticulous selection process used at our institution, which evens out the incidence of adverse outcomes across different age groups undergoing the same procedure. However, regarding the complete national liver transplantation waiting list in Mexico, out of 376 individuals, only 26 were in the “65+” category, perhaps reflecting that age is the exclusive reason older adults are not being considered for liver transplant. Consequently, the results of the present study could be used as initial support for the statement that age, alone, does not influence the outcome of mortality, at least in the short term, in liver transplant recipients. Taking that into account could potentially benefit patients that are “fit” for transplantation, despite their chronologic older age.
Limitations of the present study were the fact that the data were derived from a single center, the sample size was relatively small, no patients 70 years of age or older were included, and the survival data comparison was performed over a 2-year period. However, perhaps the study’s biggest strength was the selection protocol employed at our institution. It is a comprehensive clinical assessment, rather than simply a cutoff value for age, which may render a similar incidence of adverse health-related outcomes after liver transplant in both older recipients (between 60–69 years) and their younger counterparts. With that in mind, patient age should not be an exclusion criterion for transplantation if the overall health status of the patient allows that therapeutic option.
We found no statistically significant differences in the survival times of older adults and younger adults that received a liver transplant. Given that the mortality rate did not change during the 2-year follow-up, those results suggest that older patients should not be excluded from the selection process due to age, alone. Moreover, older adults could significantly benefit from transplantation, through improved autonomy and quality of life. However, more evidence from larger, multicenter, prospective studies with longer follow-up periods is needed to assess all the potential benefits that liver transplantation can offer the older adult.
FundingNone.
Conflict of interestNone.
Please cite this article as: Hernández-Ruiz V, García-Lara JMA, Zamudio-Rodríguez A, García-Juárez I, Avila-Funes JA. Trasplante de hígado en adultos mayores mexicanos: un estudio comparativo en un solo centro. Revista de Gastroenterología de México. 2019;84:455–460.