The prevalence of cow's milk protein allergy (CMPA) has increased in recent years, and is associated with antimicrobial use during the perinatal period, prematurity, the type of childbirth, and the decrease in breastfeeding. The aim of this study was to analyze whether there is any association between these factors and the development of CMPA.
Material and methodsA retrospective, comparative, cross-sectional, observational study was conducted by reviewing the case records of 101 children diagnosed with CMPA and seen at the Department of Gastroenterology and Nutrition of the Instituto Nacional de Pediatría within the time frame of January 2012 and August 2013. The following variables were included: age, sex, weeks of gestation, history of maternal infection and antimicrobial use during the pregnancy, type of delivery, and feeding with human milk, and its duration. Likewise, the case records of 90 children were reviewed as a control group on not having CMPA or any other allergy. The chi-square test was used for proportions, and the Mann-Whitney U test was used for comparing means in the statistical analysis.
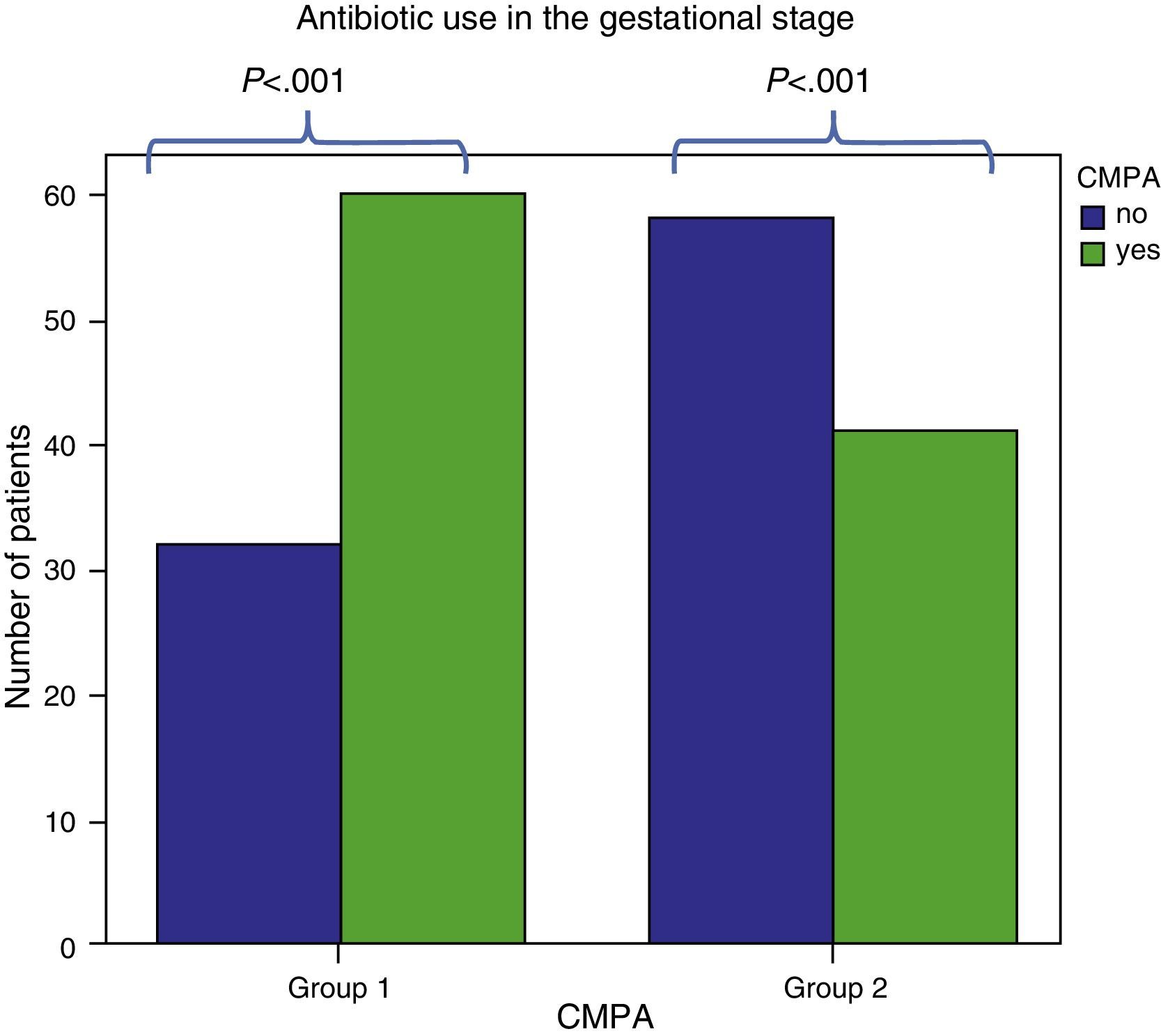
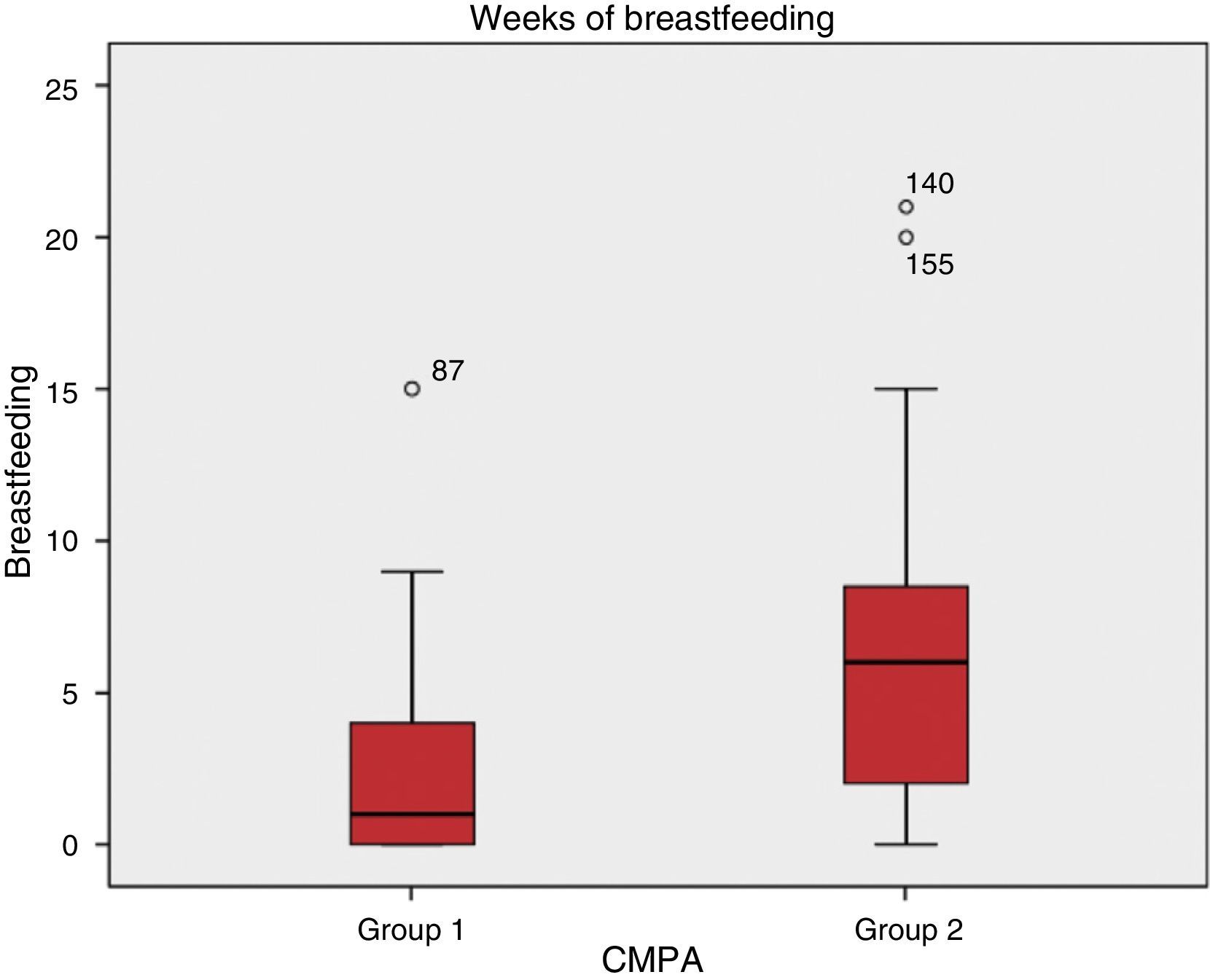
ResultsThe factors associated with CMPA were the use of antimicrobials during gestation and breastfeeding duration in months. Both factors were statistically significant (P<.001). No association was found between CMPA and gestational age or type of delivery.
ConclusionsThe statistically significant associated factors were breastfeeding duration and the use of antimicrobials during the gestational stage. These results underline the necessity for prospective studies.
La alergia a las proteínas de la leche de vaca se ha incrementado en los últimos años, asociado al uso de antimicrobianos en el periodo perinatal, prematuridad, el tipo de nacimiento y la disminución de la lactancia materna. El objetivo de este estudio fue analizar si existe alguna asociación entre estos factores y el desarrollo de alergia a las proteínas de la leche de vaca (APLV).
Material y métodosEstudio comparativo, retrospectivo, transversal, observacional. Se revisaron los expedientes de 101 niños con diagnóstico de APLV que asistieron al Departamento de Gastroenterología y Nutrición del INP de enero de 2012 a agosto de 2013. Se incluyeron las siguientes variables: edad, sexo, semanas de gestación, antecedente de infecciones y uso de antimicrobianos en la madre durante el embarazo, tipo de parto, alimentación con leche materna y duración de la misma. Así mismo se revisaron los expedientes de 90 niños como grupo control sin APLV ni otro tipo de alergias. Para el análisis estadístico se utilizo prueba de Chi cuadrado para proporciones o U-Mann-Whitney en el caso de comparación de medias.
ResultadosSe encontró que los factores asociados a APLV fueron el uso de antimicrobianos en la etapa gestacional y la duración en meses de la lactancia materna; en todos ellos existió una diferencia estadísticamente significativa (p<0.001). No se encontró asociación de APLV con la edad gestacional y el tipo de nacimiento.
ConclusiónLos factores asociados estadísticamente significativos fueron la duración de la lactancia materna y el uso de antibióticos durante la etapa gestacional, lo que obliga a realizar estudios prospectivos.
Food allergy is defined as an adverse immunologic reaction occurring from exposure to a specific food, and is different from another reaction to food, such as intolerance, drug reactions, and toxin-mediated reactions.1,2 A rise in food allergy prevalence has been observed in recent years.3,4 Cow's milk proteins are the main cause of food allergy in children under 2 years of age. Cow's milk protein allergy (CMPA) is defined as an immunologic reaction to the proteins of cow's milk, accompanied with signs and symptoms, the large majority of which are gastrointestinal, although it can also present with dermatologic and respiratory manifestations.5
There is a 2.2 to 2.8% prevalence of CMPA worldwide in children under 1 year of age. In a study on Dutch children, Schrander found a prevalence of 2.8%, whereas Host reported a prevalence of 2.2%.6,7 No epidemiologic studies have been conducted in Mexico and therefore CMPA prevalence is not known with certainty, although it has been estimated at 5 to 7%.5
There are different hypotheses for explaining the increase in allergy, and CMPA in particular, but they are subject to debate. In general, the explanatory factors that have been proposed are: the use of antimicrobials during the perinatal period, prematurity, cesarean section delivery, and a lack of feeding with human milk.8–10
The aim of the present study was to analyze this probable association with CMPA in the child population that was attended to at our institution.
MethodsA comparative, retrospective, cross-sectional, observational study was conducted. The case records were reviewed of 101 children diagnosed with CMPA (group 1) that were seen at the Department of Gastroenterology and Nutrition of the Instituto Nacional de Pediatría within the time frame of January 2012 and August 2013. The diagnosis of cow's milk protein allergy was made with the simple open blind challenge test, exactly as established in the international guidelines.11,12 All the children whose case records contained the following required information were included in the study: age, sex, weeks of gestation (all patients with 36 weeks of gestation or fewer were considered premature), maternal use of antimicrobials during the pregnancy, type of delivery, and feeding with human milk and its duration in weeks.
In order to determine antibiotic use, the mothers of the patients that utilized antibiotics in the last trimester of the pregnancy were included in the study. Likewise, the case records were reviewed of 90 children used as the control group. They were seen in gastroenterologic outpatient consultation for other reasons (hepatopathy, polyps, abdominal pain) and did not present with CMPA or any other allergy (group 2). The groups were paired by sex and age and the same variables were reviewed for both. All patients with case records that were incomplete or did not contain the required data were excluded from the study.
Statistical analysisThe SPSS v20 program was employed and descriptive statistics were used for the demographic variables. The chi-square test was used for proportions and the Mann-Whitney U test for the comparison of means.
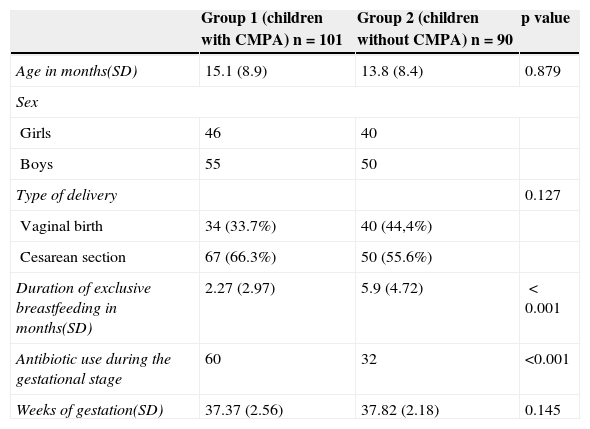
ResultsA total of 101 children were diagnosed with CMPA (group 1) and 90 children made up the control group (group 2). Table 1 shows the demographic characteristics and distribution of the children studied.
Demographic characteristics.
| Group 1 (children with CMPA) n=101 | Group 2 (children without CMPA) n=90 | p value | |
|---|---|---|---|
| Age in months(SD) | 15.1 (8.9) | 13.8 (8.4) | 0.879 |
| Sex | |||
| Girls | 46 | 40 | |
| Boys | 55 | 50 | |
| Type of delivery | 0.127 | ||
| Vaginal birth | 34 (33.7%) | 40 (44,4%) | |
| Cesarean section | 67 (66.3%) | 50 (55.6%) | |
| Duration of exclusive breastfeeding in months(SD) | 2.27 (2.97) | 5.9 (4.72) | <0.001 |
| Antibiotic use during the gestational stage | 60 | 32 | <0.001 |
| Weeks of gestation(SD) | 37.37 (2.56) | 37.82 (2.18) | 0.145 |
Results expressed in means and SD: standard deviation; CMPA: cow's milk protein allergy.
Figure 1 shows the results related to the use of antimicrobials during the third gestation trimester; 60 mothers in the CMPA group received antibiotics compared with 32 in the control group and the difference was statistically significant (p<0.001), with an OR of 2.62 (CI: 1.47-4.76)
No statistically significant differences were found in regard to gestational age or type of delivery (vaginal or cesarean section) and their association with CMPA.
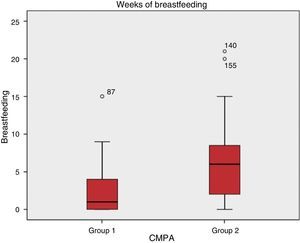
Figure 2 shows the statistically significant difference (p<0.001) found in the comparison of the months of breastfeeding in the two groups.
DiscussionDifferent articles suggest that certain factors are most likely related to the development of allergy, and to CMPA in particular.
With respect to the use of antimicrobials in the perinatal stage, it is known to be a factor that promotes changes in the gut microbiota of the mother and the fetus, which could alter the immune response, decreasing the level of cytokines that facilitate intestinal tolerance, in other words, IL-10 or TGF-ß.8 Therefore, we investigated whether there was any relation to the presence of infection in the mother and her use of antibiotics during the pregnancy and the development of CMPA. In our study, in the CMPA group, there was a greater frequency in antibiotic use and it was statistically significant. Other studies support our results; they have evaluated the relation between antibiotic use in the first months of life and allergy development, demonstrating an increase in allergies in children exposed to antibiotics during the perinatal stage.9 This association can pave the way for multivariate studies that analyze the specific importance of this factor in the development of CMPA.
Prematurity, measured in gestation weeks in this study, has also been regarded as a risk factor for the development of CMPA, due to immaturity of the gastrointestinal barrier, and even more so in those children that presented with hypoxia and intestinal ischemia, because it favors high molecular weight-antigen absorption, resulting in a greater probability for developing allergy.10,13,14 In our study, even though we found no differences between the two groups, other studies have established prematurity as a probable factor associated with the development of allergies.10
Human milk continues to be accepted as the gold standard for nutrition in children because it is known that it contains all the nutrients that are necessary and essential for good growth and development. In addition to this, it contains immunologic factors, such as IgA, TGF-ß, and IL-10 that prevent the development of allergic diseases, celiac disease, and even type 1 diabetes mellitus.15 Several studies have shown the difference in microbiota in breast-fed children, compared with formula-fed children. The microbiota of the children fed with human milk is composed of a greater number of bifidobacteria and lactobacilli, whereas the microbiota of formula-fed children consists of a greater number of enterococci and enterobacteria. This difference is thought to be due to the immunologic stimulus of the different human milk nutrients, such as the different molecules with antimicrobial activity and the presence of prebiotics and probiotics.16,17 There was a clear statistical difference in our study between CMPA development and the duration of breastfeeding. The CMPA group had a lower mean duration of 2.2 months, compared with 5.9 months in the control group.
Cesarean section delivery has also been proposed as one of the main risk factors for developing cow's milk protein allergy, asthma, and allergic rhinitis. In our study, even though there were no statistically significant differences in the two groups, there were a greater number of children delivered by cesarean section in group 1. Perhaps this can be explained by the sample size and also by the high rate of cesarean sections performed in Mexico, reaching 69.8% in the private sector and 38.9% in the public health sector hospitals according to the most recent National Health and Nutrition Survey (ENSANUT, Spanish acronym).18 Other authors have demonstrated that children delivered by cesarean section have a higher incidence of food allergies.19–21
Despite the limitations of our study, the main one being its retrospective design, we were able to identify at least 2 factors associated with CMPA. The primary factor was the reduced duration of breastfeeding. Mexico requires public policies that promote breastfeeding at least during the first year of life. Policies are also needed to prevent the indiscriminate use of antibiotics by the mother during gestation.
ConclusionsAs mentioned above, the main limitation of our study was the fact that it was a retrospective one. Nevertheless, it establishes the need for a prospective study and for the promotion of breastfeeding in an effort to reduce the number of cases of CMPA. This allergy has a high treatment cost due to the need for specialized formulas such as the extensively hydrolyzed ones and/or elemental formulas, in the most severe cases. We believe our sample size was too small to encounter a relation to the other associated factors of prematurity and childbirth by cesarean section. Moreover, an association with cesarean section deliveries was especially difficult to find, due to the high number of these types of births in Mexico.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Toro Monjaraz EM, Ramírez Mayans JA, Cervantes Bustamante R, Gómez Morales E, Molina Rosales A, Montijo Barrios E, et al. Factores perinatales asociados al desarrollo de alergia a las proteínas de la leche de vaca. Revista de Gastroenterología de México. 2015;80:27–31.