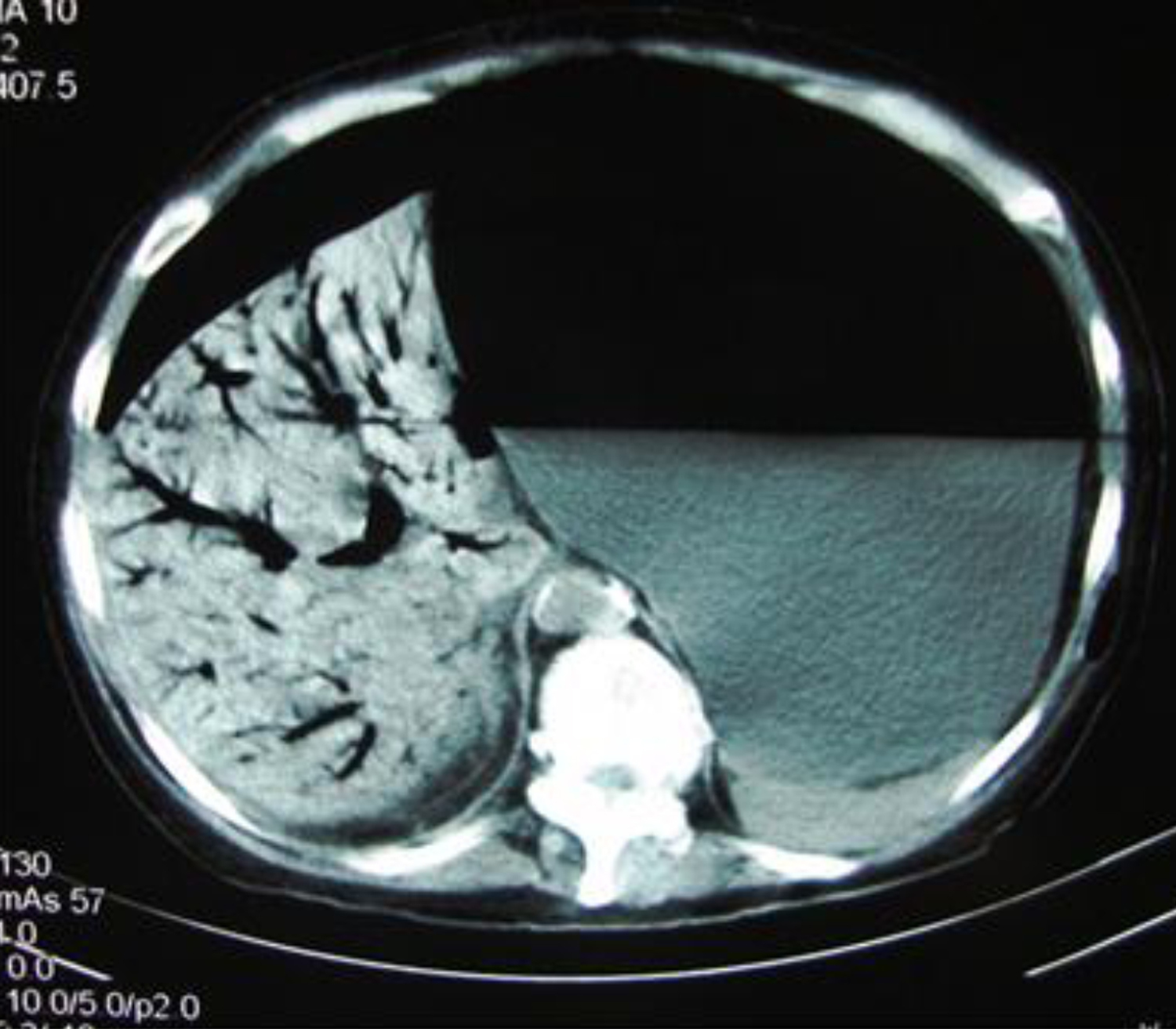
A 56-year-old woman was admitted to the emergency room with a one-day history of abdominal distension and epigastric pain. She started having symptoms after bowel preparation for colonoscopy. Abdominal CT scan showed an extremely distended stomach and small bowel (Figure 1), as well as gas in the hepatic-portal veins (Figure 2). Hepatic portal venous gas is a rare condition that occurs when intraluminal gas enters the portal venous circulation. Although there have been numerous reported causes, the majority are due to intestinal ischemia, with an estimated mortality rate of 75–80%. Mucosal barrier disruption of any kind can theoretically result in hepatic portal venous gas, but it appears to be more common in intestinal ischemia, inflammatory bowel disease, and peptic ulcer disease. Iatrogenic mucosal tears from endoscopy can also result in this situation. Diagnosis is usually made by plain abdominal radiography, sonography, color Doppler flow imaging, or computed tomography scan. An abdominal CT scan showed the classic sign of dilated vessels extending to within 2 cm of the liver capsule, in contrast to biliary gas, which ends up collecting centrally as a result of the centripetal movement of bile.
Figure 1.
Figure 2.
Conflict of interestThe authors declare that there is no conflict of interest.
Financial disclosureNo financial support was received in relation to this study.
Corresponding author at: Rua José Bonani, 199, Taubaté, São Paulo 12031-260, Brazil. Tel.: +55 012 15 36813888; fax: +55 012 15 36316061. geriaclin@hotmail.com