The risk factors for fatty liver disease are frequent in the Mexican population and the available studies appear to underestimate its prevalence. Our aims were to know the prevalence of metabolic (dysfunction) associated fatty liver disease (MAFLD) in an open population and determine the clinical and sociodemographic characteristics, nutritional status, physical activity level, and prevalence of metabolic syndrome, in the affected population.
Materials and methodsVolunteers from the general public were invited to take part in the study. Three separate questionnaires were applied to 1) determine the sociodemographic characteristics and health status of the participants, 2) evaluate the quality of their diet, and 3) to evaluate their level of physical activity. The participants underwent somatometry, laboratory tests, liver ultrasound, and FIB-4 index determination, and transition elastography (FibroScan®) was carried out on all subjects with signs suggestive of liver fibrosis that agreed to undergo the procedure. The statistical analysis was carried out using SPSS for Windows, version 22, software.
ResultsA total of 585 volunteers were studied, resulting in a prevalence of MAFLD of 41.3%, a predominance of men above 50 years of age, poor dietary habits, and sedentary lifestyle. Male sex, obesity, metabolic syndrome, and elevated ALT were risk factors for the disease and 40% of those affected had advanced fibrosis.
ConclusionsThe prevalence of MAFLD in our population is one of the highest in the world. The conditioning factors of the disease can be modified. Therefore, public policies that redirect the current trend are required.
Los factores de riesgo para la enfermedad por hígado graso son frecuentes entre la población mexicana y los estudios disponibles al parecer subestiman su prevalencia. Nuestros objetivos fueron: conocer la prevalencia de MAFLD (metabolic [dysfunction] associated fatty liver disease) en población abierta y determinar las características clínicas, socio-demográficas, estado nutricional y grado de actividad física; así como la prevalencia del síndrome metabólico entre la población afectada.
Material y métodosSe hizo una convocatoria abierta al público en general; a quienes aceptaron participar les aplicamos un cuestionario para determinar sus características sociodemográficas y estado de salud; otro para evaluar la calidad de su alimentación y uno más para evaluar su grado de actividad física. Les realizamos somatometría, exámenes de laboratorio, ultrasonido hepático y el índice FIB-4; quienes mostraron datos sugestivos de fibrosis hepática fueron convocados a una elastografía de transición (Fibroscan®). El análisis estadístico se realizó con el paquete SPSS para Windows, versión 22.
ResultadosSe estudiaron 585 voluntarios, la prevalencia de MAFLD en ellos fue de 41.3%, con predominio en hombres mayores de 50 años, con mala alimentación y sedentarismo; el sexo masculino, la obesidad, el SMet y elevación de ALT son factores de riesgo para la enfermedad; 40% de los afectados tenían fibrosis avanzada.
ConclusionesLa prevalencia de MAFLD en nuestra población es de las más altas del mundo; los factores condicionantes de la enfermedad son susceptibles de modificar por lo que se requieren políticas públicas que reorienten la tendencia actual.
At the middle of the past century, a growing number of patients with liver damage of unknown cause began to be observed; histopathologic study showed changes similar to those seen in alcoholic hepatitis, but patients stated they had no excessive alcohol consumption. This novel clinical entity was described by different names, until 1980, when Ludwig1, in an attempt to unify the diverse terminology, named it nonalcoholic steatohepatitis (NASH). We now know that it is only an intermediate stage of a more complex clinical entity that, until recently, was called nonalcoholic fatty liver disease (NAFLD).
NAFLD has very heterogeneous clinical patterns, a complex pathophysiology, and an eminently metabolic base. Consequently, a recent international expert consensus proposed naming it metabolic (dysfunction) associated fatty liver disease (MAFLD)2. To simplify its diagnosis, the documentation of steatosis through imaging studies, biomarkers, or liver biopsy, together with the presence of type 2 diabetes mellitus (DM2) and/or overweight or obesity, is now considered sufficient. Additionally, in the case of patients with normal weight and steatosis, diagnosis can be made when at least two of the following conditions are present:
- •
Dyslipidemia
- •
Waist > 102/88 cm
- •
Blood pressure > 130/85 mmHg
- •
Blood glucose level > 100-125 mg/dl
- •
HbA1c from 5.7 to 6.4% or a homeostatic model assessment (HOMA) > 2.5, for evaluating insulin resistance
- •
C-reactive protein > 2 mg/dl
There has been a notable increase in the prevalence of the disease over the past 40 years, caused by ever-increasing unhealthy lifestyle habits, characterized by the excessive consumption of foods and beverages with a high content of added sugars and saturated fats, together with extreme sedentarism. These habits have become more and more common in a broad sector of the worldwide population, and very particularly, in the Mexican population. They favor the appearance of other diseases that frequently accompany fatty liver, such as obesity, DM2, arterial hypertension (AHT), and dyslipidemia, all of which make up the so-called metabolic syndrome (MetS), of which MAFLD is another component.
MAFLD is currently estimated to affect 25% of the world population3. In Mexico, there are few prevalence studies. In 2000, a 10.3% prevalence of biopsy-corroborated nonalcoholic steatohepatitis in an open population was reported4 and in 2006, a 14.3% prevalence of ultrasound (US)-determined hepatic steatosis was reported in a population of medically insured subjects5. Recently, in 2019, at a check-up clinic in Mexico City, the results of US and laboratory test results of almost 1,500 subjects were retrospectively analyzed, reporting a 30.9% prevalence of nonalcoholic fatty liver disease6.
However, based on recent reports from the National Health and Nutrition Survey of the Mexican National Institute of Public Health, the reality of the situation may be different. Mexicans are exposed to a national environment that promotes the indiscriminate consumption of foods and beverages that favor obesity and its complications. In 2016 the survey reported that more than 70% of adults in Mexico presented with overweight and obesity, and the majority had visceral obesity, which is more frequently associated with MetS and greater cardiovascular risk. In addition, the national prevalence of chronic diseases is on the rise, such as DM (7.2% in 2006 and 9.4% in 2016)7, ATH (25.5%)8, and hypercholesterolemia (28%).
Ethnicity has also been related to a higher risk of the disease. In the United States, where there is great ethnic diversity, several studies have shown that the Hispanic population, particularly of Mexican origin, has a higher risk, even when its obesity rates are lower than those in, for example, African Americans9. A possible explanation for said risk is a certain genetic predisposition in the Mexican population related to the PNPLA-3 gene10 that induces greater susceptibility to fatty liver.
Fatty liver is frequently associated with one or more components of MetS. Its prevalence increases proportionately with the number of MetS components, and they increase the risk of fibrosis, the main factor of poor prognosis in liver disease11.
Fatty liver is a serious public health problem due to the fact that the high prevalence of metabolic comorbidities increases the demand for medical attention, as well as for economic and healthcare resources, to manage its consequences. By the year 2030, in the United States, nonalcoholic steatohepatitis is estimated to be the main cause of hepatocellular carcinoma and will hold first place among the indications for liver transplantation12.
And so, we are dealing with a disease that is highly prevalent worldwide and closely related to metabolic alterations frequently seen in the Mexican population. There are indications that Mexicans have greater susceptibility, leading to the supposition that the true prevalence in Mexico is higher than the figures reported up to now.
Because there are no current studies on the prevalence of MAFLD in an open Mexican population, the Asociación Mexicana de Gastroenterología began an epidemiologic project in 2019, the first stage of which was carried out at Boca del Rio, Veracruz.
Our aims were: to determine the prevalence of MAFLD in an open population from the municipality of Boca del Rio, in Veracruz, and describe its sociodemographic characteristics, comorbidities, nutritional status, dietary habits, and physical activity. The secondary aims were to establish the prevalence of MetS and determine the usefulness of the biologic FIB-4 index and FibroScan®, in the evaluation of liver fibrosis in patients with MAFLD.
Materials and methodsA call for study volunteers was made to the general public and workers and students of the Universidad Veracruzana. The study population included subjects above 18 years of age, born in Mexico, that gave their informed consent to undergo vital sign measurement; anthropometry that included body weight, height, waist perimeter, and a body composition analysis, using the bioelectrical impedance method with SECA mBCA-514® equipment; liver ultrasound; blood sampling for laboratory tests that included complete blood count with platelets, blood chemistry, liver function tests, lipid profile, and fasting insulin; and FibroScan®. All the volunteers took a brief survey that included a family history and sociodemographic questionnaire. Two additional questionnaires were applied, one evaluated dietary intake quality (mini ECCA, the Spanish acronym), developed by the NUTRICLOUD company13, and the other assessed the level of physical activity14 (the International Physical Activity Questionnaire), both of which have been validated in the Mexican population. The evaluations, surveys, and blood sample collection for laboratory tests were carried out over a 3-day period in February 2020, at the installations of the Instituto de Investigaciones Medico-Biológicas of the Universidad Veracruzana.
In accordance with an international expert consensus2, MAFLD was diagnosed in persons with US-identified hepatic steatosis plus overweight or obesity and/or DM2; or in subjects with normal or low weight, that had hepatic steatosis plus two or more of the following alterations: increased waist perimeter, AHT, dyslipidemia, hyperglycemia, insulin resistance, or elevated C-reactive protein.
Persons diagnosed with active cancer or a terminal disease, pregnant women, or alcohol consumption >30 g/day in men and >20 g/day in women, or persons with other known chronic liver diseases, were not included in the present study. The questionnaires, measurements, blood sample collection for laboratory tests, somatometry, ultrasound studies, and FibroScan® were performed at the installations of the Research Unit of the Instituto de Investigaciones Medico Biológicas of the Universidad Veracruzana.
Hepatic steatosis was documented through US imaging studies interpreted by radiologists certified by the Consejo Mexicano de Radiología. The laboratory tests were processed at the Diagnóstico Movil laboratory in Mexico City, whose certification is valid.
The FIB-4 index was calculated in all the volunteers to evaluate their risk for liver fibrosis, using the following formula:
The subjects with results suggestive of fibrosis were offered a FibroScan® study, 2 weeks after their initial evaluation, and as a control group, a randomly chosen subgroup of healthy non-MAFLD volunteers, were offered the same study.
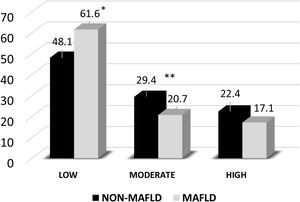
Statistical analysisThe calculation for minimum sample size was performed using the formula for calculating proportions15:
n: sample size
N: total population (variable)
Z: deviation from the accepted mean value (1.962)
p: calculated proportion (25%)
q: 1 - p (0.75%)
d: maximum allowable margin of error (5%)
To carry out the abovementioned calculation, and according to the most recent international reports, we utilized an estimated disease prevalence of 25%; a population in the state of Veracruz of 8,063,000 inhabitants in 2020; a 95% confidence interval; and a maximum allowable margin of error of 5%. Thus, we obtained a minimum of 288 individuals to analyze. By taking into account possible losses, an additional 20% was added, for a total of 346 subjects to evaluate.
To describe the patient characteristics, the results were presented in frequencies and percentages for the qualitative variables, and in means with standard deviations or medians with interquartile ranges (25th to75th percentile) for the quantitative variables, according to data distribution. Asymmetry, kurtosis, and Kolmogorov-Smirnov test values were analyzed to determine the data distribution. The statistical analysis of the quantitative variables was performed, utilizing the Student’s t test or Mann-Whitney U test for the group comparisons, depending on the normality of the data. The chi-square test or Fisher’s exact test was employed to analyze the qualitative variables. In the univariate analysis, a p ≤ 0.05 was considered for selecting the variables included in the multivariate analysis, which was performed through multiple linear regression, to identify the risk factors associated with MAFLD. The odds ratio (OR) was estimated, with a 95% confidence interval.
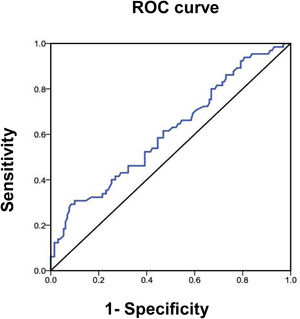
The area under the ROC curve was determined, to quantify the diagnostic accuracy of the FIB-4 index for advanced fibrosis, with respect to the FibroScan® test.
The data were captured in the Microsoft Excel® program and analyzed using the Statistical Package for the Social Sciences® for Windows®, version 22 software.
Ethical considerationsThe protocol was evaluated and approved by the Scientific Ethics Committee of the Instituto de Investigaciones Medico Biológicas of the Universidad Veracruzana, following the ethics regulations. This study was designed and conducted, according to the principles of the Declaration of Helsinki. All the participants responded to a call for voluntary participation in the study and accepted as volunteers. They signed written statements of informed consent that guaranteed the confidentiality of the personal data and all test results. All volunteers were personally advised of their results and received copies of them. When necessary, they were directed to the corresponding healthcare service to begin or continue their medical control.
ResultsA total of 585 volunteers were studied; their mean age was 48.2 ± 14.1 years, 418 were women (71.5%), and 167 were men (28.5%). The prevalence of MAFLD in the participants analyzed was 41.3%, with a slight predominance in men, at a 1.3:1 ratio (50% vs. 37.8%, OR 1.67, 95% CI 1.14-2.43; p < 0.0055).
According to the definition of the International Diabetes Federation, the prevalence of MetS was higher in the subjects affected by MAFLD (62.4%), compared with those not affected (27.4%) (p < 0.001). In addition, MetS was a risk factor for MAFLD, with an OR of 1.82 (95% CI 1.18-2.81).
The results of the homeostatic model assessment for insulin resistance showed a higher incidence in the group affected by MAFLD. That group also had higher figures of ALT and AST, as shown in Table 1.
Prevalence of MAFLD and some clinical differences in the MAFLD and non-MAFLD cases
| Variable | Non-MAFLD | MAFLD | p | OR | 95% CI | pa |
|---|---|---|---|---|---|---|
| n (%) | 343 (58.6%) | 242 (41.3%) | ||||
| Sex M/W (167/418) | 83(49.7%)/260 (62.2%) | 84(50.3%)/158 (37.8%) | < 0.006 | 1.67 | 1.14-2.43 | 0.0055 |
| Age (years) | 49 (35-59) | 50 (41-57) | 0.23 | 0.99 | 0.98-1.01 | 0.6 |
| MetS (IDF) | 94 (27.4%) | 151 (62.4%) | < 0.001 | 1.82 | 1.18-2.81 | 0.006 |
| Elevated ALTb | 61 (17.7%) | 116 (47.9%) | < 0.00001 | 4.07 | 2.8-5.9 | 0.003 |
| Elevated ASTc | 56 (16.4%) | 95 (39.3%) | < 0.001 | 1 | 0.97-1.03 | 0.928 |
| HOMA-IR | 1.4 (0.99-2.02) | 1.92 (1.35-3.19) | < 0.001 | 1.06 | 0.99-1.12 | 0.89 |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; HOMA-IR: homeostatic model assessment for insulin resistance; IDF: International Diabetes Federation; M: men; MAFLD: metabolic (dysfunction) associated fatty liver disease; OR: odds ratio; MetS: metabolic syndrome; W: women; 95% CI: 95% confidence interval.
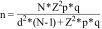
By age groups, the prevalence of MAFLD was lower in the subjects under 29 years of age (barely 3.7%), with an increase starting at 30 years of age. The group of 50 to 59 years of age was the most affected, as shown in Fig. 1.
We found no significant difference between the two groups, with respect to the characteristics of place of residence, socioeconomic status, occupation, or ethnicity.
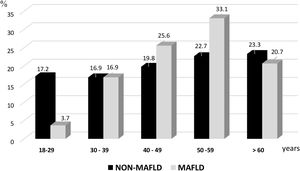
Nutritional statusThe body mass index (BMI) was higher than 25 kg/m2 in the majority of the volunteers analyzed (82.4%). In those affected by MAFLD, 29.8% presented with overweight, 66.9% with obesity, and only 3.3% had normal weight (Fig. 2). A BMI ≥ 30 kg/m2 was a risk factor for the disease, with an OR of 4.59 (95% CI 3.23-6.53), p < 0.00001.
With respect to body composition, the higher percentage of fat (predominantly visceral fat) and lower percentage of lean mass, in the volunteers with MAFLD, are shown in Table 2.
Results of the nutritional status evaluation
| All n = 585 | Non-MAFLD n = 343 | MAFLD n = 242 | p | |
|---|---|---|---|---|
| Weight (kg) | 75.6 (64.5-87.7) | 69.5 (60.7-81.0) | 81.6 (72.8-94.5) | < 0.001 |
| BMI (kg/m2) | 29.7 (26.1-34.4) | 27.3 (24.4-31.1) | 31.9 (29.3-35.9) | < 0.001 |
| Abdominal perimeter (cm) | 94 (85.4-104.3) | 88.5 (80.5-98) | 102 (93.2-111.3) | < 0.001 |
| Hip circumference (cm) | 104 (97.5-112.8) | 100.5 (95-108) | 108 (101.7-116) | < 0.001 |
| Waist-hip index | 0.90 (0.84-0.96) | 0.87 (0.82-0.93) | 0.94 (0.88-0.98) | < 0.001 |
| Fat mass (%) | 41.4 (35-7-46.9) | 40.6 (34.5-45.6) | 42.9 (37.1-48.3) | < 0.001 |
| Lean mass (%) | 58.5 (53.0-64.2) | 59.4 (54.4-65.4) | 57.1 (51.7-62.9) | < 0.001 |
| Muscle mass (kg) | 19.1 (15.8-24.7) | 17.8 (15.1-22.1) | 20.5 (16.9-26.9) | < 0.001 |
| Visceral fat (kg) | 2.9 (2.2-3.8) | 2.5 (2.0-3.3) | 3.4 (2.7-4.6) | < 0.001 |
| Quality of diet according to the mini-ECCA | ||||
| Very good dietary habits | 119 (20.3%) | 74 (21.6%) | 45 (18.6%) | |
| Good dietary habits | 226 (38.6%) | 141 (41.1%) | 85 (35.1%) | 0.058 |
| Poor dietary habits | 190 (32.5%) | 102 (29.7%) | 88 (36.4%) | |
| Very poor dietary habits | 50 (8.5%) | 26 (7.6%) | 24 (9.9%) | |
BMI: body mass index; MAFLD: metabolic (dysfunction) associated fatty liver disease.
Regarding the dietary intake quality evaluated in the Mini-ECCA questionnaire, poor dietary quality was more common in the MAFLD group (Table 2).
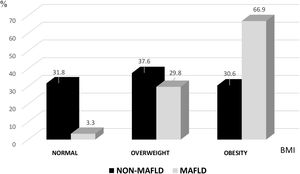
Physical activityThe International Physical Activity Questionnaire revealed that 61.6% of the subjects with MAFLD had a low level of physical activity vs. 48.1% of the non-MAFLD group, with a statistically significant difference (OR 95% CI 1.24-2.42; p < 0.001). Moderate physical activity was associated with a lower risk of MAFLD (OR IC 95% 0.42-0.92; p < 0.017) and a high or more intense level of physical activity was more common in the non-MAFLD group (Fig. 3). Those data underline the importance a low level of physical activity has in the pathophysiology of the disease.
FibrosisThe results of the FIB-4 index showed that 64.8% of the study sample had no signs indicative of fibrosis; 33% had an indeterminate result, and 2.2% had signs suggestive of advanced fibrosis.
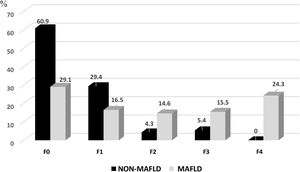
FibroScan® was performed 2 weeks after the initial evaluation, once the results of the laboratory tests were reviewed. Of the 195 volunteers that underwent the test, 103 were from the MAFLD group and 92 were from the non-MAFLD group. In those subjects that presented with MAFLD, 29.1% had grade F0, 16.5% had F1, 14.6% had F2, 15.5% had F3, and 24.3% had F4. A grade ≥ F2 was more common in the subjects with MAFLD than in the non-MAFLD group (54.5% vs. 9.7%), as shown in Fig. 4. Importantly, according to those results, almost 40% of the subjects in the MAFLD group already had advanced grades of fibrosis (F3-F4).
The area under the curve for the FIB-4 index, for evaluating the presence of advanced fibrosis (≥ F3) by FibroScan®, showed 31% sensitivity and 90% specificity, with an area under the ROC curve of 0.610 (95% CI 0.53-0.69; p = 0.013). The Spearman correlation of the FIB-4 index with FibroScan®, for advanced fibrosis in the 195 individuals evaluated, was r = 0.230 (p < 0.001) (Fig. 5).
Discussion and conclusionsFew studies have been carried out on the prevalence of fatty liver in Mexico. Those that have been conducted are not up-to-date, and their results are conflicting, due to the fact that the majority are performed on selected populations, leading to bias. Unlike the previous studies, ours was conducted on an open population, with an adequate sample size, and is the first study to establish the prevalence of fatty liver, according to the new nomenclature of MAFLD. In addition, it analyzed the sociodemographic conditions of the subjects affected, their health status, dietary quality, and customary physical activity.
The increase in the prevalence of MAFLD is closely related to obesity, DM2, and MetS. According to the Encuesta Nacional de Salud y Nutrición survey, the prevalence of obesity in the Mexican population, in persons above 20 years of age, is 42%. The situation is alarming in the Mexican pediatric population, given that 27.8% of children under 11 years of age already present with overweight or obesity16.
The metabolic alterations in the Mexican population are exacerbated by the national obesogenic environment that promotes poor dietary habits and a sedentary lifestyle.
Based on our results, we conclude that the prevalence of MAFLD in our population is elevated (41.3%), and among the highest worldwide.
Similar to that reported in international studies, our results showed a higher occurrence of MAFLD in men above 50 years of age that had a sedentary lifestyle, poor eating habits, and obesity. Male sex, obesity, MetS, and elevated ALT were shown to be risk factors for the disease.
In contrast to reports conducted in Asia, the percentage of cases with MAFLD in normal weight subjects in our population was low, at barely 3.3% of the sample.
In the analysis of cases of suspected advanced fibrosis, the correlation between the FIB-4 index and FibroScan® results was low, and those results are being carefully analyzed.
Regarding the FibroScan® results, it is concerning that close to 40% of the subjects with MAFLD had advanced fibrosis, especially because fibrosis is the most important factor for poor prognosis, in such cases.
Our study is the first collaborative effort carried out to document the prevalence of MAFLD in an open population in Mexico and the initial report of the general results are presented herein. The rest of the information is vast, a large part of which is still being processed, and will be described in much more specific and detailed future reports.
One of the limitations of the present study is the fact that the majority of the population that responded to a call for volunteers were workers at the Universidad Veracruzana and their relatives, which could result in reference bias, with respect to the sociodemographic status of the subjects analyzed. In addition, our results are regional, and in future studies on MAFLD, its behavior and prevalence in other regions of the country are important to determine, given the heterogeneity in the Mexican population. We must also clarify that even though patients with significant alcohol consumption, as well as those with other chronic liver diseases, are included in the new MAFLD definition, we decided to exclude those cases, to carry out an evaluation of patients with a predominance of metabolic dysfunction.
Thus, we are able to conclude that the prevalence of MAFLD in our population is one of the highest worldwide and that the affected group shares widely described characteristics, such as the presence of MetS, poor dietary habits, and a sedentary lifestyle, with the disease appearing more frequently in men above 30 years of age and less frequently in thin persons.
The high prevalence seen in our population can be explained by multiple factors. An important fact to consider is that the majority of the predisposing factors to the disease are modifiable, such as harmful habits, overweight, and obesity. Therefore, in light of our results, more aggressive public health measures should be taken to combat the sedentary lifestyle and poor dietary habits, particularly in the pediatric population, and in turn, promote a significant change in current behavioral patterns, toward healthier ones. In addition, we recommend establishing surveillance programs in at-risk populations and increasing the population’s awareness of the severity of this disease. By not doing so, if the current trend continues, we can expect to see the development of MetS and MAFLD at earlier ages in the pediatric population, with the consequent increase in mortality, related to liver diseases, cardiovascular diseases, and malignant tumors.
Lastly, with respect to MAFLD as the new nomenclature of this disease, in an effort to unify the term in the Spanish-speaking world, our group supports the proposal of the Spanish group that recommends calling it by the Spanish acronym EHmet (Esteatosis Hepática Metabólica)17.
Financial disclosureThis study was conducted with the financial support of the Research Fund of the Research committee of the Asociación Mexicana de Gastroenterología.
Conflict of interestThe authors and co-authors declare that there is no conflict of interest.
The authors wish to thank the Research Committee of the Asociación Mexicana de Gastroenterología for the financial support and the Instituto de Investigaciones Médico Biológicas of the Universidad Veracruzana for the logistical support, in carrying out the present study.
Please cite this article as: Bernal-Reyes R, Icaza-Chávez ME, Chi-Cervera LA, Remes-Troche JM, Amieva-Balmori M, Priego-Parra BA, et al. Prevalencia y características clínico-epidemiológicas de una población mexicana con enfermedad del hígado graso asociada a disfunción metabólica: un estudio en población abierta. Rev Gastroenterol Méx. 2023;88:199–207.
See related content at https://doi.org/10.1016/j.rgmxen.2022.04.003, M. Hernández-Conde and J.L. Calleja, Metabolic liver disease: A new preventable pandemic, Revista de Gastroenterología de Mex.2023;88:197–198.