Esophageal perforation is an uncommon event that is a medical/surgical emergency, with a 15-30% mortality rate. The aim of the present study was to communicate our experience in the management of esophageal perforation, evaluating the different strategies utilized, in an effort to establish measures to guide decision-making in selecting treatment.
Materials and methodsA retrospective descriptive study was conducted on patients diagnosed with esophageal perforation at our hospital center, within the time frame of 2000 and 2019.
ResultsOver the past 19 years, 15 patients were diagnosed with esophageal perforation. Surgical treatment was carried out in 80% of the cases. Primary closure, reinforced with plasty, was performed in 67% of the patients, of whom 62.5% had early diagnosis and a 100% survival rate. Diagnosis was late in 37.5% of the cases, with a 33.3% survival rate. Esophagectomy and gastric pull-up were performed on 25% of the patients, 66.6% of whom had early diagnosis and a 100% survival rate. In the 33.3% that had late diagnosis, the mortality rate was 100%. Esophagectomy, with cervical esophagostomy and feeding jejunostomy, was performed on one of the patients (8.3%) that had early diagnosis and a 100% survival rate.
ConclusionsThe main survival predictor in esophageal perforation is the interval of time between the injury and its diagnosis, and in turn, the resulting treatment. Each patient with esophageal perforation should have individualized treatment to adequately manage the condition.
La perforación de esófago es una patología poco frecuente, siendo una urgencia médico-quirúrgica con una mortalidad del 15-30%. El objetivo del estudio es comunicar nuestra experiencia en el manejo de la perforación esofágica, evaluando las distintas estrategias usadas, y tratar de establecer unas pautas para orientar en la toma de decisiones en el tratamiento a seguir.
Material y métodosEstudio descriptivo retrospectivo de pacientes diagnosticados con perforación de esófago en nuestro centro desde el año 2000 hasta el 2019.
ResultadosEn los últimos 19 años, 15 pacientes fueron diagnosticados con perforación de esófago. Se realizó tratamiento quirúrgico en el 80% de los casos. Se realizó sutura primaria reforzada con plastia en el 67% de los pacientes, y de ellos fueron diagnosticados de manera precoz el 62.5% con una supervivencia del 100%. El 37.5% fueron diagnosticados tardíamente con una supervivencia del 33.3%. Se realizó esofaguectomía y ascenso gástricos en el 25% de los pacientes, de ellos se diagnosticaron de manera precoz el 66.6% con una supervivencia del 100%. El 33.3% fueron diagnosticados tardíamente con una mortalidad del 100%. En uno de los pacientes (8.3%) se realizó esofaguectomía con esofagostoma cervical y yeyunostomía de alimentación, siendo diagnosticado de manera precoz con una supervivencia del 100%.
ConclusionesEl principal predictor de supervivencia en la perforación de esófago es el intervalo de tiempo entre la lesión y el diagnóstico, y por tanto del tratamiento. El tratamiento de la perforación esofágica debe individualizarse en cada paciente, para poder realizar un adecuado manejo de esta patología.
Esophageal perforation is an uncommon event. It is a medical/surgical emergency, with a 15-30% mortality rate.1–4
At present, its incidence has increased, and its etiology has changed. Fifty percent of cases are due to an iatrogenic cause because of the increase in the performance of diagnostic and therapeutic endoscopic techniques.2–4
Because the esophagus has no serosa, it is exposed to total perforations, and thus to contamination of the mediastinum. Given the poor ability to limit infection, it rapidly progresses to mediastinitis. The severity of esophageal perforation is determined by the contamination of the mediastinum from gastroduodenal content and oral secretions. Said contamination triggers mediastinitis, which if not treated, can rapidly progress to sepsis and death.3–6
The main survival predictor in cases of esophageal perforation is the interval of time from the esophageal injury to its diagnosis and subsequent treatment.5–7
Its management, whether conservative or surgical, is still a subject of debate. Conservative treatment of esophageal perforation is accepted in patients that meet the Cameron criteria. Described in 1979, those criteria are: a well circumscribed intramural or transmural perforation, no signs or symptoms of sepsis, a contained perforation, no distal obstruction or malignant esophageal disease, and perforation that is not located in the abdominal esophagus.
If the Cameron criteria are not met, conservative treatment is contraindicated, and surgical treatment should be carried out.6–11
The aim of the present study was to communicate our experience in the management of esophageal perforation at a tertiary care center, evaluating the different strategies employed and attempting to establish guidelines that can aid in deciding on the choice of treatment.
Materials and methodsA retrospective descriptive study was conducted on patients diagnosed with esophageal perforation at our hospital center, within the time frame of 2000-2019. The inclusion criteria were: diagnosed esophageal perforation, patients above 14 years of age, and conservative, endoscopic, or surgical treatment.
Patients under 14 years of age and those with esophageal perforation secondary to caustic substance ingestion were excluded.
The study variables were age, sex, location, etiology, previous esophageal disease, time interval to diagnosis, presence or absence of signs of sepsis (through the Quick SOFA score), the Cameron criteria, treatment (conservative, endoscopic, or surgical), surgical technique, complications, and survival.
Statistical analysisA retrospective descriptive analysis of the study variables was carried out, with the qualitative variables expressed as frequency percentages and the quantitative variables as measures of central tendency.
The statistical analysis was performed using the SPSS 16.0 program.
ResultsOver the past 19 years, 15 patients were diagnosed with esophageal perforation. Ten of those patients were men, 5 were women, and their mean age was 65 years (range: 41-90).
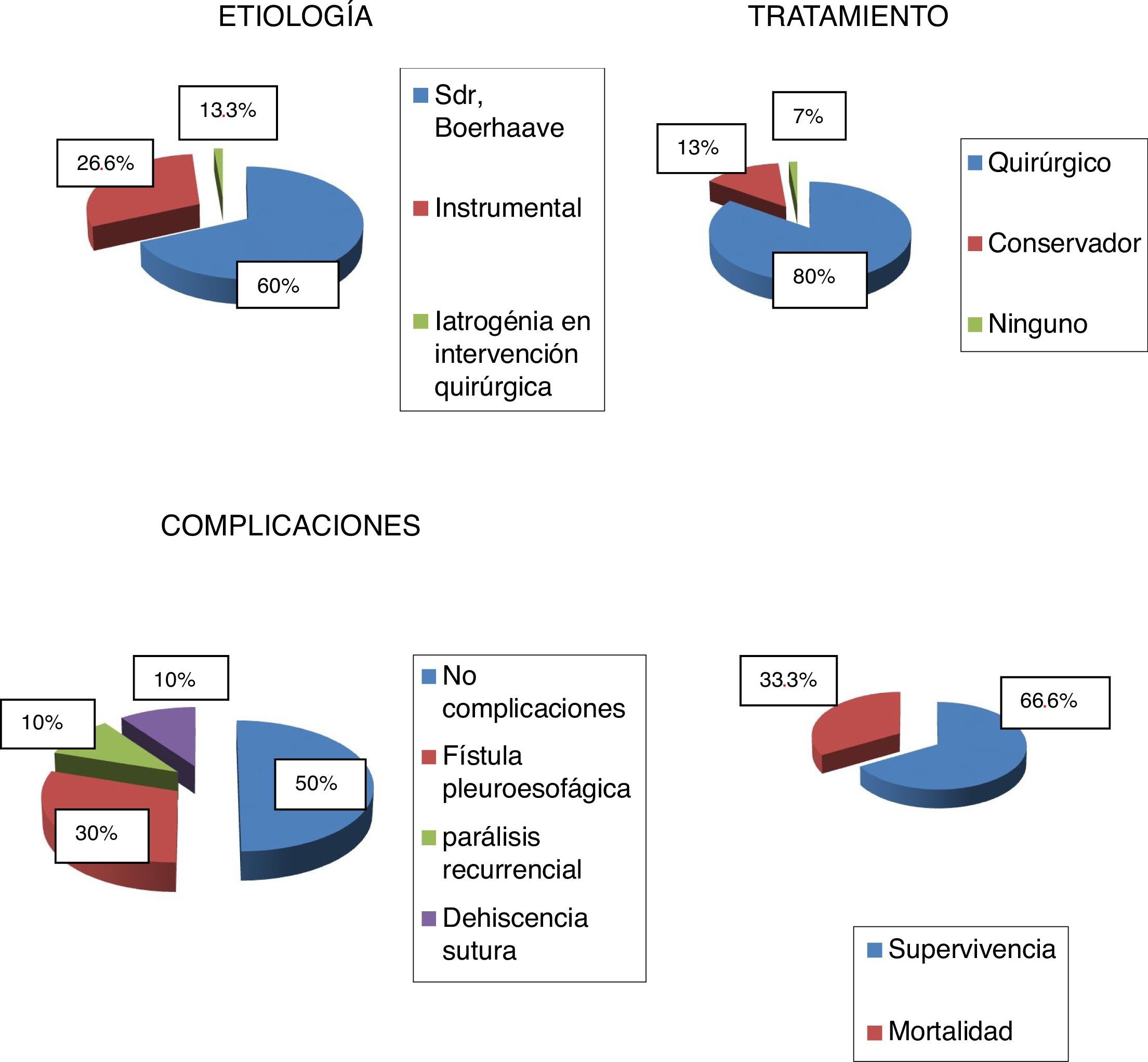
Etiology frequency was 9 (60%) patients with Boerhaave syndrome, 4 (26.6%) patients with perforation due to instrumentation, involving dilation for achalasia, post-endoscopic retrograde cholangiopancreatography, and endoscopic stent removal, and 2 (13.3%) patients with perforation due to iatrogenic surgical injury.
The clinical characteristics of the sample, location of the perforation, time interval from the perforation event to diagnosis, presence or absence of the Cameron criteria, treatment (conservative, endoscopic, or surgical), survival, and postoperative complications are summarized in Table 1.
Clinical characteristics of the patients.
| Etiology | Location | Event-to-treatment time interval | Cameron criteria | Treatment | Survival and complications |
|---|---|---|---|---|---|
| Boerhaave syndrome | - Cervical esophagus: 0 patients | < 24 h: 4 patients | Yes: 0 | Conservative: 1 patient | Survived: 5 patients |
| 9 patients | - Thoracic esophagus: 7 patients | >24 h: 5 patients | No: 9 patients | Surgical: 7 patients | Complications: |
| - Abdominal esophagus: 2 patients | None: 1 patient | - Esophagopleural fistula: 3 patients | |||
| - No complications in 3 patients | |||||
| Iatrogenic endoscopic injury (dilation for achalasia, post-ERCP, stent removal) | - Cervical esophagus: 1 patient | < 24 h: 4 patients | Yes: 2 patients | Conservative: 1 patient | Survived: 4 patients |
| 4 patients | - Thoracic esophagus: 3 patients | >24 h: 0 patients | No: 2 patients | Surgical: 3 patients | No patient presented with complications |
| - Abdominal esophagus: 0 patients | |||||
| Iatrogenic surgical injury (surgical intervention for giant hiatal hernia) | - Cervical esophagus: 0 patients | < 24 h: 1 patient | Yes: 0 patients | Conservative: 0 patients | Survived: 1 patient |
| 2 patients | - Thoracic esophagus: 0 patients | >24 h: 1 patient | No: 2 patients | Surgical: 2 patients | Complications: |
| - Abdominal esophagus: 2 patients | - Recurring paralysis |
ERCP: endoscopic retrograde cholangiopancreatography.
The most frequent perforation location in our sample was the thoracic esophagus, occurring in 10 patients (66.6%), followed by the abdominal esophagus, presenting in 4 patients (26.6%), and the cervical esophagus, occurring in one patient (6.6%).
In the patients with thoracic esophageal perforation, surgical treatment was carried out in 8 patients (80%) and conservative treatment in one patient (10%), due to high anesthesia and surgery risk and severe associated comorbidities. The other patient died during the diagnosis (10%).
Thoracic esophageal perforation survival was 6 patients (60%).
Surgical treatment was carried out in 100% of the 4 patients that had abdominal esophageal perforation, with a 75% survival rate.
The only patient that presented with cervical esophageal perforation received conservative treatment and survived.
Diagnosis made in fewer than 24 h from clinical symptom onset was considered early diagnosis and diagnosis made more than 24 h from clinical symptom onset was considered late diagnosis. Based on those definitions, early diagnosis was made in 9 cases (60%), with 100% survival, whereas late diagnosis was made in 6 cases (40%), with 0% survival.
Conservative treatment encompassed: medical treatment, pleural drainage tube placement, or percutaneous drainage performed by an interventional radiologist.
Surgical treatment included: primary suture, esophagectomy with or without reconstruction through gastric pull-up in the same surgery, placement of a T-tube drain to produce a targeted fistula, and esophageal exclusion.
One patient (7%) died during the diagnosis; thus, no treatment was carried out.
Two patients (13%) received conservative treatment. One of those patients had cervical esophageal perforation secondary to endoscopic retrograde cholangiopancreatography. The Cameron criteria were met, diagnosis was early, and the patient survived. The other patient had thoracic esophageal perforation secondary to Boerhaave syndrome, did not meet the Cameron criteria, had late diagnosis, and died.
Surgical treatment was performed in 80% of the cases, 8.3% of whom met the Cameron criteria.
Even when the Cameron criteria were met, the surgical team that evaluated the patients decided upon surgical treatment if there was poor progression despite conservative treatment, a progressive increase in acute phase reactants in the laboratory tests, and clinical worsening, with an increase in dyspnea and hemodynamic instability.
Regarding the surgical techniques, 67% of the patients had primary suture. Early diagnosis was made in 62.5% of them, with 100% survival, and late diagnosis was made in 37.5%, with 33.3% survival.
Esophagectomy and gastric pull-up were performed in 25% of the patients. Early diagnosis was made in 66.6% of them, with 100% survival, and late diagnosis was made in 33.3%, with 0% survival.
Esophagectomy with cervical esophagostomy and feeding jejunostomy was performed in 8.3% of the patients, with early diagnosis and 100% survival.
The overall mortality rate of our case series was 33.3% and the overall survival rate was 66.6%.
Survival was 100% in all the patients with early diagnosis, regardless of perforation location or etiology or the treatment performed.
Fifty percent of the cases had no postoperative complications.
One of the most frequent postoperative complications was esophagopleural fistula (30%). It was treated conservatively, with the exception of one case that required surgical treatment. Esophagectomy with cervical esophagostomy and feeding jejunostomy was performed, with reconstruction 4 years later, through colonic transposition.
There was one lethal outcome due to postoperative primary suture dehiscence.
The graphs showing the results in percentages of etiology, treatment, mortality, and complications in the sample are displayed in Fig. 1.
Discussion and conclusionsIn our case series, the most frequent cause of esophageal perforation was Boerhaave syndrome (60%), followed by perforation due to instrumentation (26.6%), unlike the current tendency, in which the most frequent cause is due to instrumentation, at 50%, according to the literature.2–5
The most frequent location of the perforations was the thoracic esophagus (66.6%), followed by the abdominal esophagus (26.6%) and the cervical esophagus (6.6%).
Surgical treatment was carried out in the patients with perforations in the thoracic esophagus and those with perforations in the abdominal esophagus, regardless of whether or not the Cameron criteria were met, with the exception of two cases of thoracic esophageal perforation. One of them died during the diagnosis and the other underwent conservative treatment due to advanced age (90 years), severe associated comorbidities, and high anesthesia and surgery risk.
The patient with cervical esophageal perforation received conservative treatment and survived. Cervical esophageal perforations have a better prognosis because there is no early mediastinal involvement. Good results with conservative treatment in that group of patients have been described in the literature.8–10
The choice of surgical technique depends on the location of the perforation, the presence or absence of previous esophageal disease, the scope of contamination, esophageal viability, and the general health status of the patient, all of which are dependent on the time interval from the perforation event to the diagnosis/treatment. Outcome is less favorable for patients with late diagnosis and for those that undergo more aggressive surgical treatment (e.g., esophagectomy, if the patient remains hemodynamically stable, and esophageal exclusion or targeted fistulization, if the patient is hemodynamically unstable and/or is a high surgical risk).
If the esophageal wall is viable and the associated contamination is mild, primary suture associated with drainage can be performed.10,11
Esophageal perforation is a surgical emergency, with high mortality. A 30% mortality rate is described in the literature, and it was 33.3% in our case series.
Severity is determined by the contamination of the mediastinum with salivary secretion and gastroduodenal content, that rapidly progresses to mediastinitis, given that the infection is difficult to delimit. Everything depends on the time interval from the perforation event to its diagnosis and consequent treatment.12–16
In our case series, the patients that had early diagnosis had 100% survival, regardless of the location or etiology of the perforation or the treatment carried out.
In 1979, Cameron defined the criteria that esophageal perforations should meet, for the patient to undergo conservative treatment, signifying that either conservative or surgical treatment could be correct.
Conservative treatment is a risky therapeutic choice, given that mediastinal sepsis can progress, if not treated aggressively. Thus, some authors do, not recommend it, whereas others reserve it solely for perforations that are diagnosed late, meet the Cameron criteria, because the development of sepsis is less frequent in those patients.
Conservative treatment has also been proposed for patients that have a high anesthesia and surgery risk due to elevated comorbidity.1–3
If the Cameron criteria are not met, conservative treatment is not indicated, and the patient should undergo surgery.
Patients with early diagnosis more frequently meet the Cameron criteria because the time interval from the perforation event to diagnosis is shorter, supposing less contamination of the mediastinum, which determines severity, and consequently less systemic involvement of sepsis.
In conclusion, the main survival predictor in esophageal perforation is the time interval between the injury and its diagnosis, and in turn, its treatment. Treatment should be individualized in each patient, with the option of conservative treatment in cases that meet the Cameron criteria. The correct identification of patients that can undergo conservative treatment offers the possibility of satisfactory progression, with low morbidity and mortality, eliminating the need for surgery, and thus minimizing risks and the associated healthcare costs. However, if the classification is incorrect, and a patient with surgical criteria is given conservative treatment, the results will certainly be bad. Therein lies the importance of ample knowledge of the criteria for conservative versus surgical treatment in the life-threatening event that is esophageal perforation.
Ethical considerationsThe authors declare that no experiments were conducted on humans or animals for the present study, that they have followed the protocols of their work center on the publication of patient data, and that they have preserved patient anonymity at all times.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: García-Moreno V, Maiocchi K, Gómez-Quiles L, Villarin-Rodríguez A, Aliaga-Hilario E, Martínez-Hernández A, et al. Tratamiento de la perforación de esófago, revisión de nuestra experiencia en un hospital de tercer nivel en los últimos 19 años. Rev Gastroenterol Méx. 2022;87:405–410.