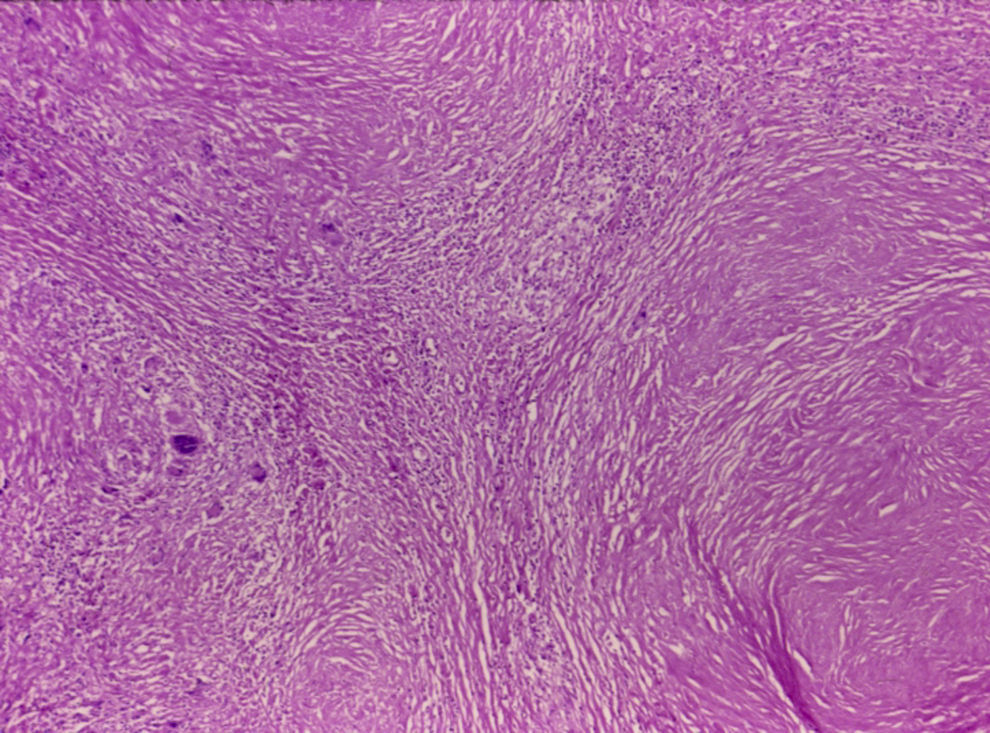
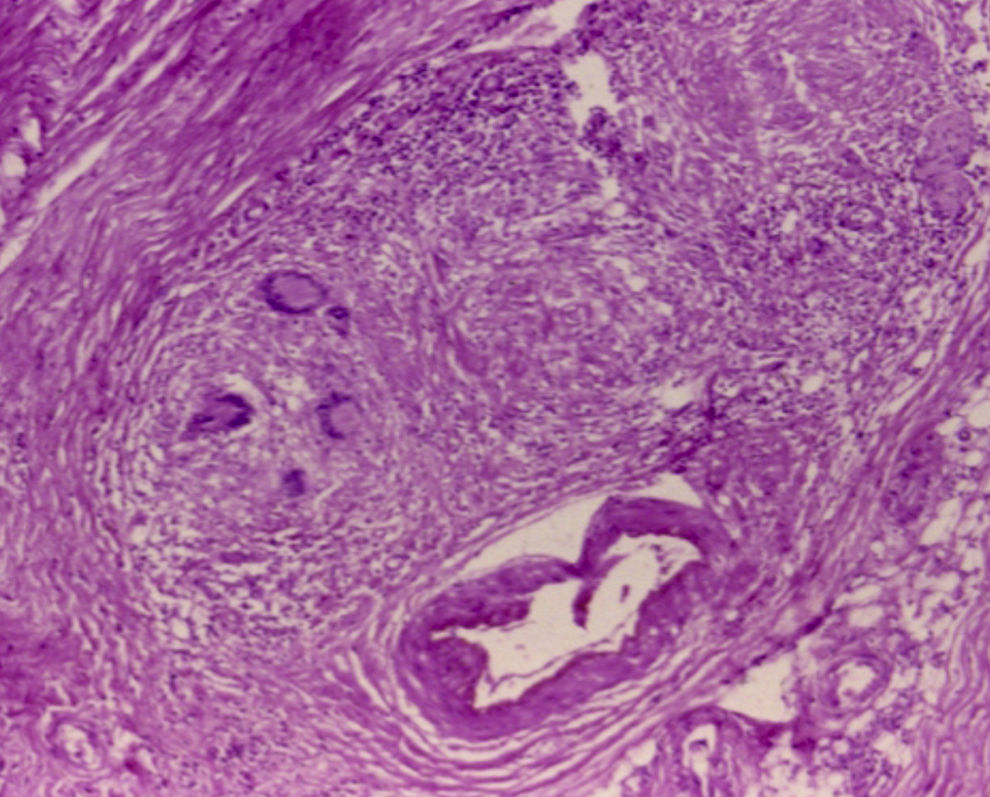
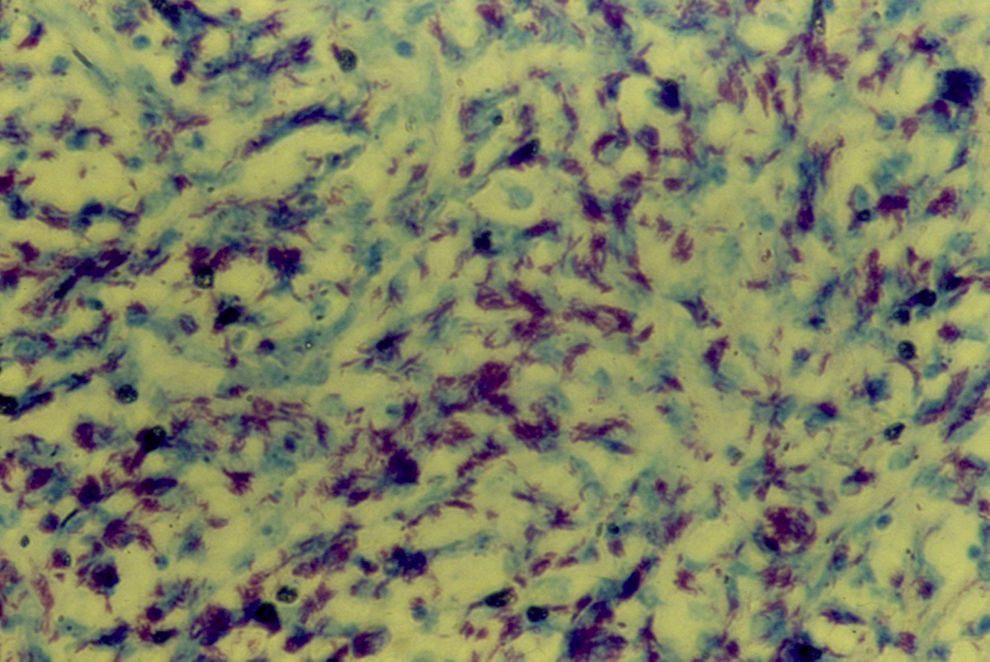
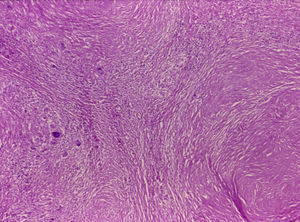
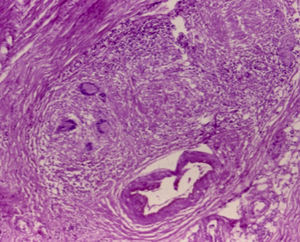
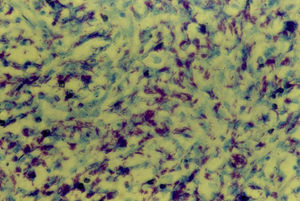
A 38-year-old single woman had type 2 diabetes mellitus. Her current illness began 3 months prior with anal pruritus, with burning anal pain and bleeding. Two weeks later, perianal ulcers appeared with increased pain and bleeding (fig. 1). The patient applied lidocaine and hydrocortisone ointments with no improvement. She sought medical attention for this symptomatology, and due to the size and lateral location of the ulcers, they were biopsied. The histopathologic study reported the presence of Langhans giant cells and an intense granulomatous reaction (figs. 2 and 3). The PCR test was positive for tuberculosis. Ziehl-Neelsen staining was done and was positive for Mycobacterium tuberculosis (fig. 4).
The patient was treated with isoniazid, rifampin, pyrazinamide, and ethambutol for 2 months and then for 6 months more with isoniazid and pyrazinamide, resulting in symptom remission and cicatrization of the perianal ulcers.
Cutaneous tuberculosis is currently very rare and can present as lupus vulgaris, miliary lesions, erythema induratum of Bazin, abscesses, or ulcers. There are very few reported cases of perianal cutaneous tuberculosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Medina-Murillo GR, Rodríguez-Medina U, Rodríguez-Wong U. Tuberculosis cutánea perianal. Revista de Gastroenterología de México. 2017;82:259–260.