There is growing evidence that gut flora plays a role in the development of Irritable Bowel Syndrome (IBS). Abdominal bloating is a common symptom in these patients and the severity of this symptom could be related to the variations in their fermentative profiles, obtained by measuring the levels of breath hydrogen excretion after lactulose ingestion.
AimsOur objective was to determine the difference in abdominal bloating severity between IBS patients with high vs low levels of breath hydrogen excretion after lactulose administration.
MethodsLactulose breath tests were carried out on IBS patients in our institution between July 2009 and August 2010. Patients were requested to fill out a validated questionnaire to assess the severity of their symptoms. Abdominal bloating severity score was compared among patients with high and low breath hydrogen levels.
ResultsA total of 234 patients were enrolled. There was a statistically significant difference in the abdominal bloating severity score between groups: 7.0 (5.7-8.0) vs 6.5 (5.0-7.5), p=0.001. The comparison among IBS patients with constipation (IBS-C) in both groups also showed a statistically significant difference: 7.5 (6.0-8.5) vs 5.8 (3.5-7.2), p=0.0051.
ConclusionsThose patients with a low level of breath hydrogen excretion after lactulose ingestion presented with significantly greater abdominal bloating than those with a high level of breath hydrogen excretion.
Existen cada vez más evidencias de que la flora intestinal juega un papel en el desarrollo del síndrome de intestino irritable (SII). La sensación de distensión abdominal es un síntoma frecuente en estos pacientes, y la severidad del mismo pudiera estar relacionada con las variaciones en el perfil fermentativo, de acuerdo con los niveles de hidrógeno espirado luego de la ingesta de lactulosa.
ObjetivosDeterminar la diferencia en la severidad de la sensación de distensión abdominal entre pacientes con SII, con alto vs bajo nivel de hidrógeno espirado luego de la administración de lactulosa.
MétodosSe realizaron pruebas de aliento con lactulosa en pacientes con SII de nuestra institución, entre julio del 2009 y agosto del 2010. A todos los pacientes se les solicitó que completaran un cuestionario validado, para determinar la severidad de sus síntomas. De acuerdo con este, se comparó la severidad de la distensión abdominal entre pacientes alto y bajo nivel de hidrógeno espirado.
ResultadosUn total de 234 pacientes fueron incluidos. Se encontró una diferencia estadísticamente significativa en el grado de severidad de la distensión abdominal entre los grupos: 7,0 (5,7-8,0) vs 6,5 (5,0-7,5), p=0,001. La comparación entre pacientes con SII con estreñimiento (IBS-C) en ambos grupos, también mostró una diferencia estadísticamente significativa: 7,5 (6,0-8,5) vs 5,8 (3,5-7,2), p=0,0051.
ConclusionesAquellos pacientes con bajo nivel de hidrógeno respiratorio excretado, luego de la ingesta de lactulosa presentaron significativamente mayor severidad de la distensión abdominal, en comparación con aquellos con un alto nivel de excreción respiratoria de hidrógeno.
Irritable bowel syndrome (IBS) is a functional bowel disorder characterized by the association of abdominal pain or discomfort with an alteration in bowel habit.1 Its exact etiology remains unknown; it is thought to be a multifactorial problem, and may include altered motility, visceral hypersensitivity, and a chronic inflammatory response.2 There is growing evidence that bacteria may play a role in IBS.3 It is also known that the relative predominance of specific bacterial populations may determine the presenting symptoms.4
Abdominal bloating is a common symptom among these patients, and its exact mechanism is unknown; evidence as to its origin points toward a complex interaction of multiple factors, such as intestinal dysmotility or paradoxical abdominal wall movements, as contributors.5,6 This could be the result of an increased production of intestinal gas and is related to an altered fermentative profile.7–9 However, it is not known whether the frequency and severity of abdominal bloating fluctuates with the variations in pulmonary hydrogen excretion. Our aim was to determine the difference in abdominal bloating severity between IBS patients with both high and low breath hydrogen excretion.
Since low breath hydrogen excretion is possibly related to an increase in methane excretion, we hypothesized that a difference in the severity of abdominal bloating could be found due to the effect of methane on intestinal motility, as has been previously described.10
MethodsA sequential analysis of lactulose breath tests (LBT) carried out at the Gastroenterology Division of the Centro de Educación Médica e Investigación Clínica (CEMIC) in Buenos Aires-Argentina between July 2009 and August 2010 was performed. Consecutive outpatients from the Gastroenterology Division with a diagnosis of IBS according to Rome III criteria were selected. Demographic data and the IBS Severity Symptom Scale (IBS-SSS) scores were collected. The bloating score was compared between the groups.
IBS Severity Symptom ScaleAll patients filled out the IBS-SSS questionnaire to assess the severity of their symptoms. This scale had been previously translated and validated into Spanish11,12 and consists of five 10-point visual analog scales to rate each item. The items evaluated by this questionnaire were: abdominal pain intensity, abdominal pain frequency (number of days over the last ten days when abdominal pain was significantly present), abdominal bloating severity, satisfaction with bowel movement frequency, and the impact of symptoms on patient quality of life. Abdominal bloating severity was calculated in each patient using a scale from 0 to 10.
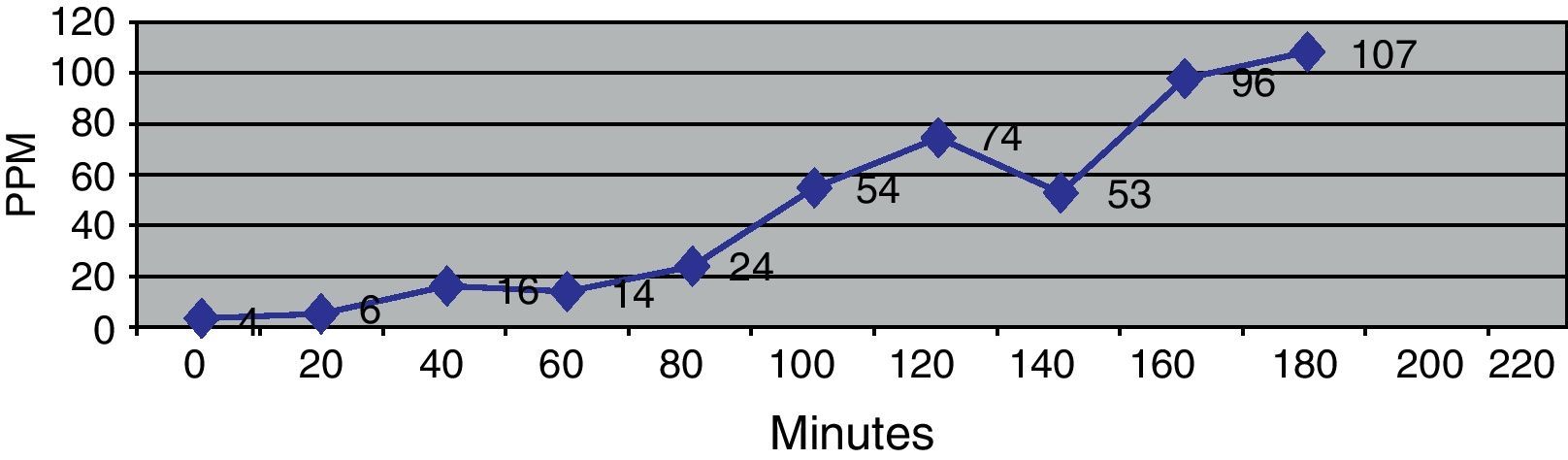
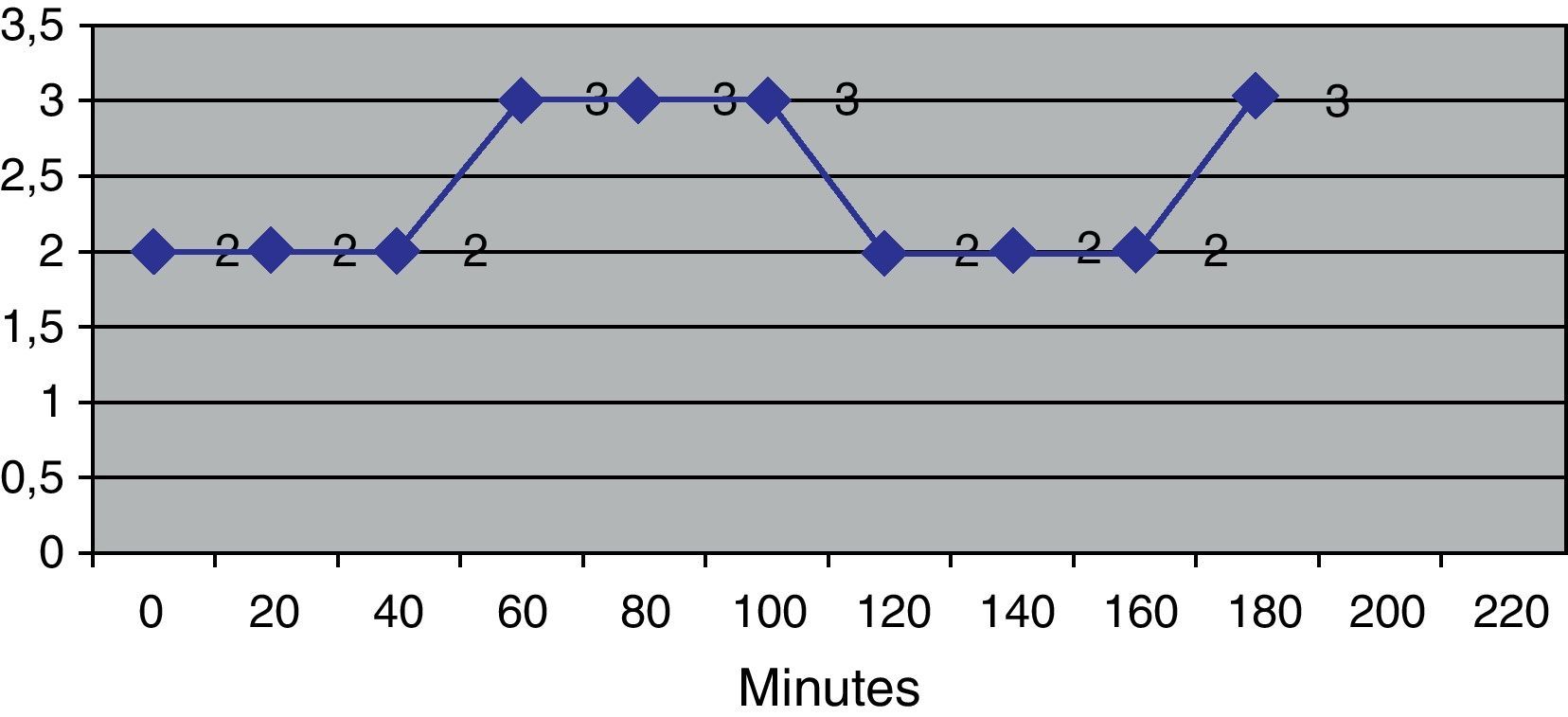
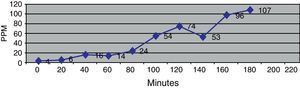
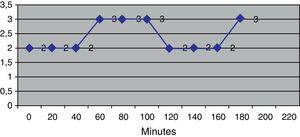
Lactulose Breath TestThe LBT was performed according to previously described techniques13 as part of the study protocol carried out on these patients at our institution. After a 12-hour fasting period, patients were asked to drink 10g of lactulose and to periodically collect exhaled samples of breath (every 20minutes for a three hour period). The samples were then analyzed for hydrogen concentrations (measured in parts per million) using a QuinTron® 12I plus gas chromatograph (QuinTron® Instruments Company, Milwaukee, WI, USA). The results were used to create a hydrogen concentration/time curve, and the area under the curve (AUC) was calculated for each case, as previously done by Kotler et al.14
Patients were classified into two groups according to the results of the LBT: those with a low (<1.000) and those with an elevated (>3.000) AUC (Figs. 1 and 2). Those patients with AUC values between 1.000 and 3.000 were excluded, because these values are considered to be within normal range.
Patients taking part in the trial were required to pay for their lactulose breath tests. This expense was covered by the health insurance of those subjects that could not afford the tests. All participating patients signed an informed consent document approved by the Institutional Review Board (IRB).
Statistical AnalysisFor statistical analysis, Epi Info® (3.5.1 Version, Center for Disease Control and Prevention, Atlanta GA) was used. Categorical variables were expressed as percentages. Continuous variables were expressed as mean ± standard deviation (SD), or median with interquartile range, in the case of non-parametric variables. Comparison of continuous variables was made using the Student's t test or Mann-Whitney U test for non-parametric variables. Comparison of categorical variables was carried out using the Fisher's exact test. A p value of <0,05 was considered to be statistically significant.
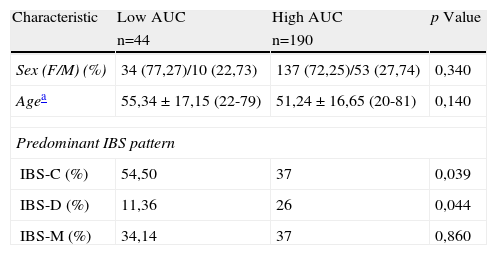
ResultsA total of 380 patients were included in the study. One hundred and twenty patients with a LBT AUC between 1.000 and 3.000 were excluded, along with 10 patients unwilling to complete the IBS-SSS questionnaire. Sixteen unsubtyped IBS (IBS-U) patients were also excluded because of the small number of patients in this group. Two hundred and thirty-four patients were classified into the above-mentioned groups: 190 in the AUC >3.000 group and 44 in the AUC <1.000 group. The baseline characteristics of both groups are shown in Table 1. Forty-four patients (19%) showed an early increase in hydrogen excretion compatible with small intestine bacterial overgrowth (SIBO), according to previously used criteria.12 These patients were included in the AUC >3.000 group.
Demographic comparison between patients with abnormally high and low AUC in the LBT.
| Characteristic | Low AUC | High AUC | p Value |
| n=44 | n=190 | ||
| Sex (F/M) (%) | 34 (77,27)/10 (22,73) | 137 (72,25)/53 (27,74) | 0,340 |
| Agea | 55,34 ± 17,15 (22-79) | 51,24 ± 16,65 (20-81) | 0,140 |
| Predominant IBS pattern | |||
| IBS-C (%) | 54,50 | 37 | 0,039 |
| IBS-D (%) | 11,36 | 26 | 0,044 |
| IBS-M (%) | 34,14 | 37 | 0,860 |
AUC: area under the curve; LBT: Lactulose Breath Test; IBS-C: irritable bowel syndrome with constipation; IBS-D: irritable bowel syndrome with diarrhea; IBS-M: mixed irritable bowel syndrome.
There was a significantly higher proportion of IBS-C patients in the low AUC group, and a higher proportion of IBS with diarrhea (IBS-D) in the high AUC group. There was no difference in age or sex between groups.
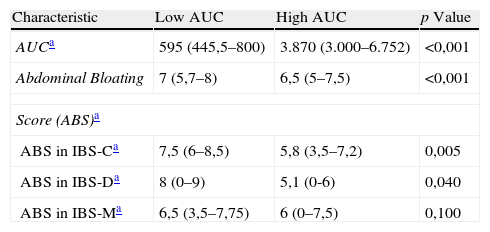
Severity of abdominal bloating was compared, as shown in Table 2. Patients with a low AUC presented a slightly higher, but significant score in abdominal bloating severity. Since abdominal bloating severity has been associated with the presence of constipation, and the low AUC group had a higher proportion of IBS-C patients, abdominal bloating scores between IBS-C patients in both groups were compared. Moreover, the difference between IBS-C patients in both groups remained significant. Table 2 also shows the difference in bloating severity between IBS-D and mixed IBS (IBS-M) patients.
Comparison of the IBS-Severity Symptom Scale and the LBT between groups.
| Characteristic | Low AUC | High AUC | p Value |
| AUCa | 595 (445,5–800) | 3.870 (3.000–6.752) | <0,001 |
| Abdominal Bloating | 7 (5,7–8) | 6,5 (5–7,5) | <0,001 |
| Score (ABS)a | |||
| ABS in IBS-Ca | 7,5 (6–8,5) | 5,8 (3,5–7,2) | 0,005 |
| ABS in IBS-Da | 8 (0–9) | 5,1 (0-6) | 0,040 |
| ABS in IBS-Ma | 6,5 (3,5–7,75) | 6 (0–7,5) | 0,100 |
LBT: Lactulose Breath Test; AUC: area under the curve; ABS: abdominal bloating score; IBS-C: irritable bowel syndrome with constipation; IBS-D: irritable bowel syndrome with diarrhea; IBS-M: mixed irritable bowel syndrome.
In the current study we found that those IBS patients with low hydrogen excretion in the LBT have slightly higher, but significant abdominal bloating severity than those with elevated hydrogen excretion, a finding that could be related to the predominance of hydrogen-consuming gut flora.
As mentioned before, a large proportion of IBS patients complain of abdominal bloating, irrespective of the predominant cathartic symptom pattern.5 There are several factors that contribute to the occurrence of bloating in these patients, and probably the best explanation for this symptom is an interaction between all of them. For instance, Tremolaterra et al. showed that the inability of the abdominal wall muscles to adapt to the changes of intraabdominal volumes is related to this symptom.6 It could be associated with an abnormal production of intestinal gas. Accarino et al. found an increase in intestinal gas production during bloating episodes both in patients with intestinal dysmotility and in those with normal function. They also described changes in abdominal wall motion during these episodes.15
There is considerable evidence demonstrating that bacterial flora have an etiologic role in the genesis of IBS symptoms. Kassinen et al. showed that the fecal microbiota is significantly altered in IBS patients.16 Several studies show an increased hydrogen excretion in breath tests using non-absorbable saccharides, suggesting the presence of SIBO in IBS patients.17,18 A recent meta-analysis by Shah et al. described a LBT sensitivity and specificity of 43,6% and 83,6%, respectively, in the diagnosis of IBS.3 This is a very controversial point, because the LBT has not been shown to be a useful tool for distinguishing IBS patients from controls.19 This etiologic association is further suggested by controlled trials that have shown a symptomatic improvement in IBS patients treated with antibiotics, such as neomycin, metronidazole or rifaximin.20–22
According to current evidence, patients with elevated hydrogen excretion in a LBT suffer from more severe and frequent symptoms than those that have a normal-range pulmonary excretion of this gas. However, there is a distinct population with a low concentration of hydrogen excretion that may have a different symptomatic pattern. Extremely low values of breath hydrogen have been shown to be associated with methane that is produced by intestinal microorganisms. Cloarec et al.23 have found an inverse relationship between hydrogen and methane concentrations in breath tests performed on normal subjects.
We excluded those patients with an AUC in the LBT between 1.000-3.000, because these patients have values of hydrogen excretion considered to be within normal limits, according to previous evidence.17
Hydrogen measurement in the LBT shows clear advantages over breath methane testing; first, it is easier to measure and therefore is more feasible.24 On the other hand, we believe the hydrogen breath test would be a valuable initial approach in selected patients, because not only could its low excretion be inversely related to methane production, but it could also reflect the predominance of sulphate-reducing bacteria, whose influence in colonic motor abnormalities is not known. There is evidence to support the idea that intestinal gases, such as methane, can be active molecules, producing an alteration in intestinal motor function. A study by Pimentel et al. showed an inverse relationship between serotonin concentration and methane production in IBS patients; serotonin is known to participate in the control of peristaltic movements. In part, this may be an action mechanism of methane in bowel movement dysfunction.10 Furthermore, the abovementioned can explain why patients with a low AUC in our cohort showed a significantly higher frequency of IBS-C. Agrawal et al. found a significant association between abdominal distention and delayed intestinal transit and constipation.25 Intestinal transit was measured by the LBT. In order to avoid bias, and given that IBS-C patients were present in both studied groups, these patients were analyzed separately, and a significant difference was still found in the abdominal bloating severity score between high and low AUC in the LBT.
Study limitations have been taken into consideration. First of all, we did not measure pulmonary methane excretion. Evidence points toward a link between methane production and constipation, and could be related to the low pulmonary hydrogen excretion and abdominal bloating severity in these patients. On the other hand, we did not take into account some relevant clinical variables of the included patients, such as body mass index. We only compared abdominal bloating severity between groups, and did not consider the presence and severity of abdominal distention. Unfortunately, breath testing is an indirect and imperfect measurement of the pathologic action of gut flora. However, it is far more feasible than other tests that are considered more specific, such as small bowel culture. As a consequence, care must be taken when drawing conclusions from the results of our study.
ConclusionsPatients with a low area under the curve in the lactulose breath test have more severe abdominal bloating than the IBS patients with elevated hydrogen pulmonary excretion, regardless of the predominant clinical pattern.
FundingNo financial support was provided.
Conflicts of interestThe authors have no conflicts of interest to declare.