¿ Introduction
Amebiasis is the infection of the human gastrointestinal tract by Entamoeba histolytica (EH), a protozoan parasite that is capable of invading the intestinal mucosa and spreading to other organs causing abscesses.1,2 Most prevalent in the tropics and subtropics, EH infections mostly occur in the developing world. Nevertheless, amebiasis also occurs sporadically in the temperate climates of developed countries and in some risk groups. Increased severity of amebiasis is noted in children (especially newborns), in women who are pregnant or postpartum, corticosteroid users, individuals with malignancy, and in the malnourished patients.1,3
Presentation ranges from mild diarrhea to dysentery and liver abscesses. However, it is known that even after years of the last episode of dysentery, a localized infection in the colon may, rarely, form a segmental mass, called ameboma. This occurs more frequently in patients untreated or inadequately treated during the course of an amoebic colitis. Diagnosis is difficult and in most cases done after surgical interventions due to insidious onset and variability of signs and symptoms.4-6 Here, we report a clinical case of cecal ameboma clinically diagnosed previous to surgical intervention that stress the importance of early multidisciplinary diagnosis and the effectiveness of standard anti-parasitic therapy.
¿ Case report
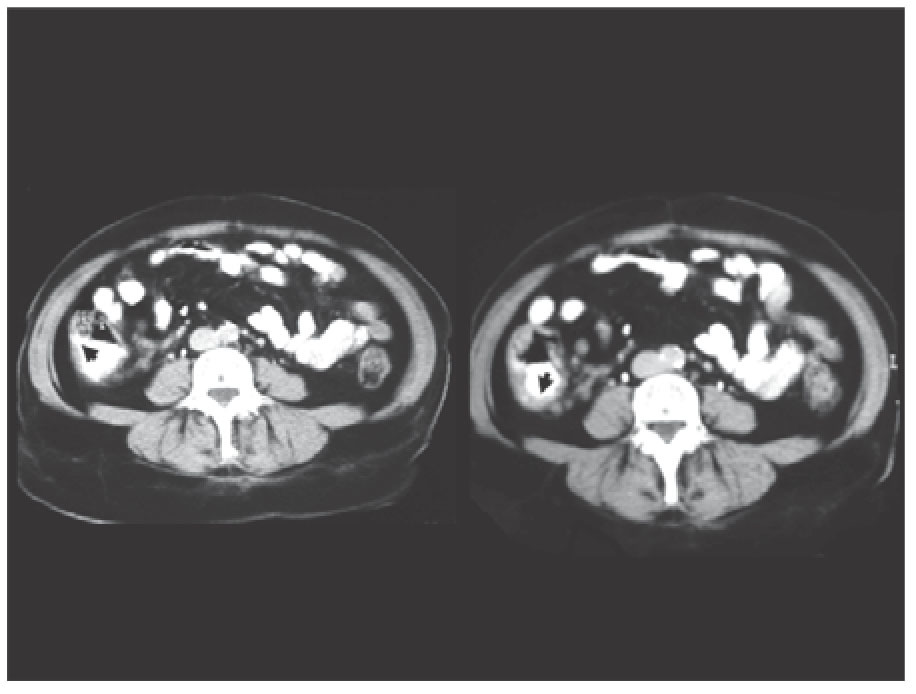
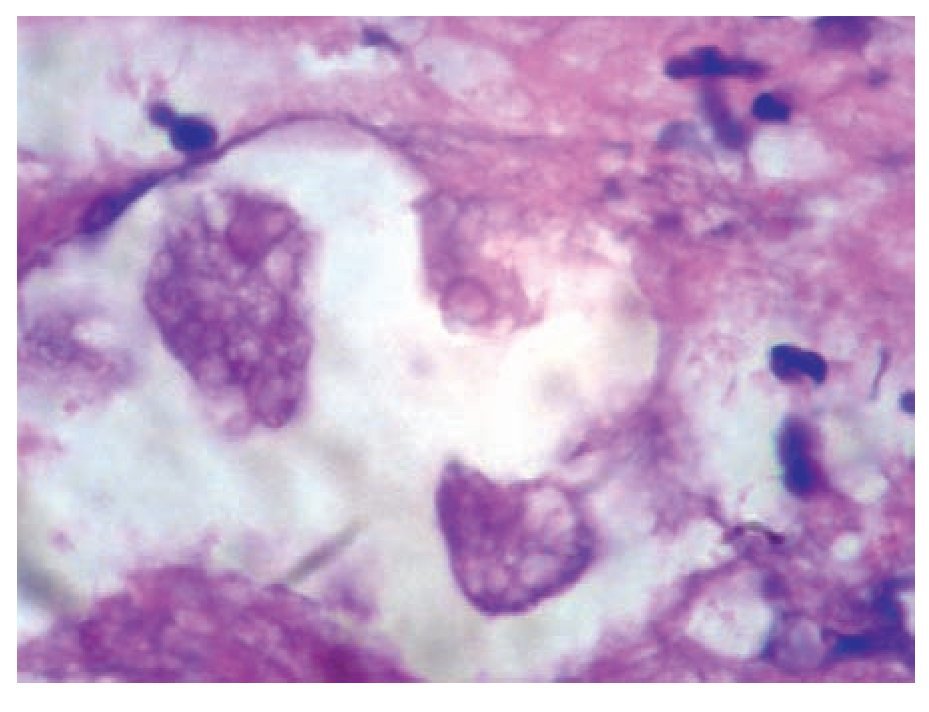
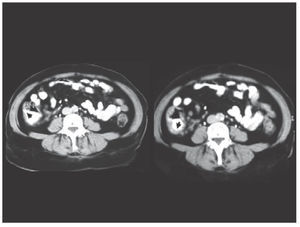
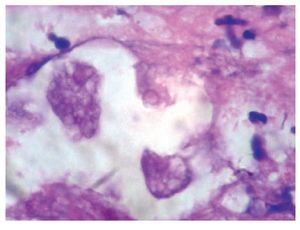
This is a 52 years old, Mexican-mestizo female, presented to our gastrointestinal emergency unit with a history of a week right lower quadrant abdominal pain, intermittent fever, bloating, tenesmus and mucus discharge in the stools. She had experienced a three kilograme weight loss in the previous four months, associated with an episode of acute bloody diarrhea which was self-medicated. Abdominal examination was soft, with palpable mass and tenderness in right lower-quadrant. No peritoneal signs were documented. Laboratory exams were unremarkable. Contrast-enhanced tomography (CT) revealed a concentric thickening (22 mm) of the cecum wall (Figure 1). The liver, spleen and pancreas were normal. Given the results of CT scan (concentric thickening and mass-like appearance on the cecum wall) a preliminary diagnosis of colon cancer was made. A colonoscopy was performed and showed a bulky-ulcerated mass in the cecum area. Multiple "flask-shaped" ulcers were documented on the surrounding mucosa and several endoscopic biopsies were taken. On histological examination, the presence of multiple crypt abscesses and superficial ulcerations were identified. In addition, amebic trophozoites were documented within the exudative tissue. Numerous phagocyted red blood cells, which are characteristic of EH, were contained within the trophozoites (Figure 2). Subsequent laboratory parameters also revealed positive anti-amoebic antibodies (titles of 1:512).
¿ Figure 1. Double contrast CT scan of the abdomen showing an irregular concentric mass on the cecal wall (large arrows) partially compressing the terminal ileum.
¿ Figure 2. Endocopic biopsy sample of a colonic ulcer showing inflammatory infiltrate Entamoeba histolytica trophozoites and trophozoites containing numerous phagocytosed red blood cells.
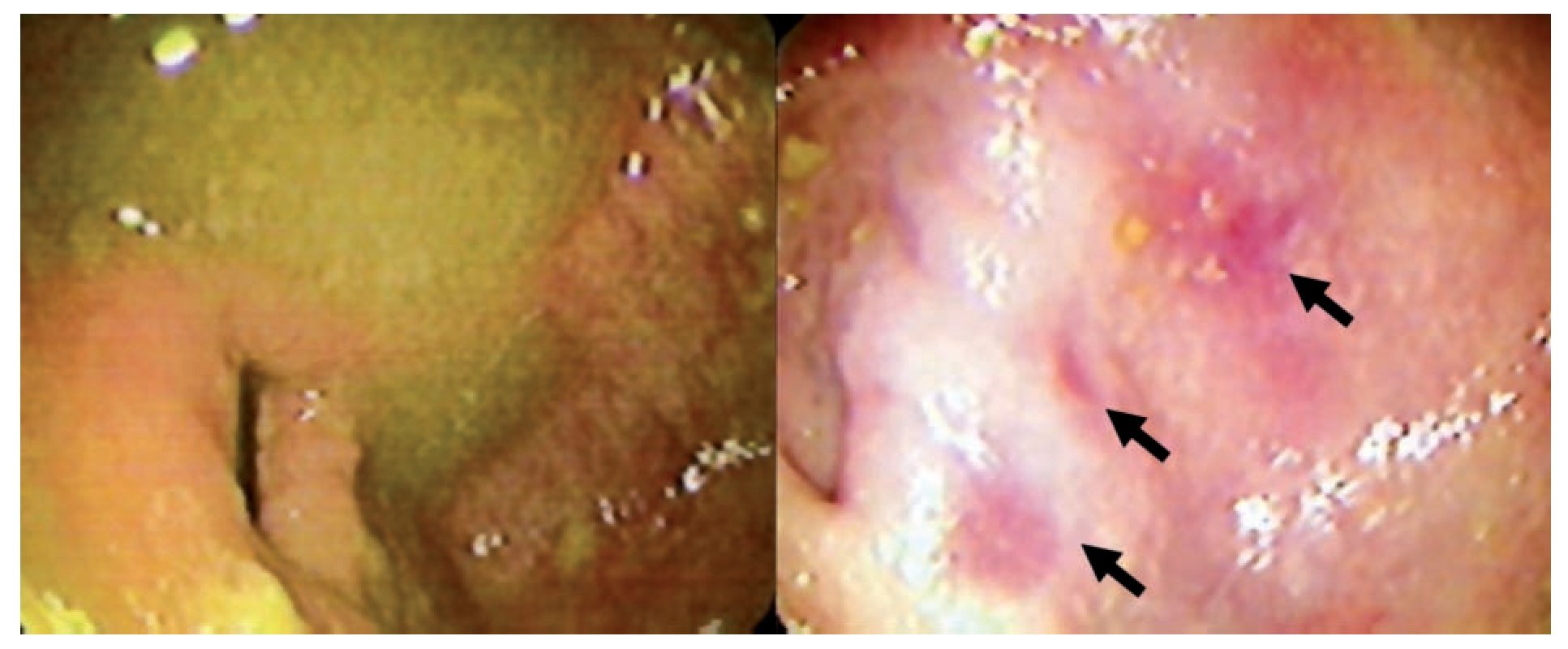
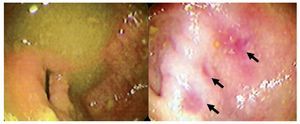
The patient was treated with oral metronidazole for 14 days, showing good clinical recovery and was discharged after two weeks due to persistent abdominal pain within the first week after starting anti-parasitic drugs and completing the diagnostic approach. During follow-up a colonoscopy was performed showing a normal cecum mucosa except for some areas of focal hyperaemia (Figure 3). The control CT scan four weeks after treatment was completely normal.
¿ Figure 3. Follow-up colonoscopy showing normal mocosa and some foci of hyperaemia (arrows) in the cecum wall.
¿ Discussion
Amebiasis is a major cause of morbidity by parasites worldwide. It is the third most common parasitic cause of death after malaria and schistosomiasis.7 EH is transmitted by the fecal-oral route. Typically, infection is acquired from ingestion of water or food contaminated by cysts. After ingestion, cysts release vegetative trophozoites at the ileo-cecal valve region and then multiply by binary fusion. Characteristic symptoms only occur when trophozoites invade the gastrointestinal mucosa. Once trophozoites encyst and infectious cyst are excreted in the feces, the life cycle of EH is complete. There is no intermediate animal host.1,8 Amebic trophozoites are capable of phagocytosis, and the demonstration of ingested red blood cells within the trophozoites indicates invasive disease. Intestinal invasion of EH results in colonic mucosal ulceration and give rise to the classic "flask-shaped" ulcers covered with white slough.9,10
In rare cases, patients with long-standing infection can develop exophytic, cicatricial and inflammatory tumors called amebomas. In these, the tissue necrosis (characteristic of amebic colitis) is replaced by an extensive inflammatory reaction. One possible explanation for this reaction is secondary bacterial over infection.11
It has been estimated that ameboma occurs in 1.5 to 8.4% of all cases.12,13 A frequent clinical observation is the reference of previous dysenteric episodes without or with inadequate treatment. Amebomas are usually solitary, variable in size and can be up to 15 cm in diameter. Men within the second and fifth decade of life are most commonly affected. Symptoms include diarrhea, fever, weight loss, rectal bleeding and in some cases bowel obstructive symptoms.1,11 In endemic areas cramping, lower abdominal pain and a palpable mass may suggest the diagnosis. Differential diagnosis must be made with Crohn's disease, appendix abscesses in younger patients and colon cancer or diverticulitis in the elderly.9
Contrast-enhanced tomography and colonos-copy are sensitive tools for the workshop of differential diagnosis of a cecal mass. Endoscopic evaluation can yield a definitive diagnosis in about 66% of cases.9 The most relevant CT findings are ileocecal tumor and partial or concentric thickening of the colonic wall. Furthermore, CT scan can help detect spread lesions to other organs.12
Other diagnostic tools are EH-specific antigen or DNA detection in stools and the presence of amebic antibodies (70-90% sensitivity) in serum samples.1,14 Histological examination of colonoscopic biopsies may be vital for the diagnosis. Although, early infection may show only non-specific neutrophilic infiltration and erosions of the intestinal mucosa, in more advanced cases the diagnosis can be based on the trophozoites detection within the necrotic debris.
Other microbiological diagnosis to considerate in patients with histological characteristics of amebiasis is the prescence of Entamoeba dispar (ED) colonization. At the beginning of the twentieth century, it was known that some people infected with EH apparently never develop symptoms and their infections spontaneously disappear. This was interpreted by many researchers as an indication that the parasite had a variable virulence. However, Brumpt in 1925 suggested the alternative explanation of the existence of two species, one capable of producing invasive disease (Entamoeba dysinteriae), and another non-pathogenic species, which he named Entamoeba dispar (ED) but were the genetic studies provided by Diamond and Clark, which demonstrated the existence of genetic differences between the two amoebas, allowing the actual and formal description of EH as the cause of amebiasis and ED as a commensal in the large bowel.14,15 Practically, the presence of red blood cells within the cytoplasm of trophozoites is a diagnostic feature for the identification of EH. Ingested RBCs are not frequently seen and in the absence of this diagnostic characteristic E. histolytica / E. dispar should be reported.16
Treatment of amebic invasion to the colonic wall includes five to 10 days of oral metronidazole (750 mg t.i.d.). In addition, an anti-amoebic luminal agent (eg. diloxanide fuorate or paromomycin) is recommended to eliminate invasive disease.1,8Usually, ameboma responds well to pharmacologic therapy and most cases improve or disappear after few weeks of treatment.18 Surgical intervention may be required only if there are complications. However, in the vast majority of cases, amebomas are confirmed when surgery was performed by preliminary diagnosis of carcinoma, acute appendicitis, lymphoma or after histological evaluation of a colonic mass discovered unexpectedly during surgery.3,19,20 This highlights the importance of keeping an open mind during the diagnostic approach of a patient with colonic tumor and to consider the "four horsemen" of cecum pathology (carcinoma, lymphoma, tuberculoma and ameboma) as a required differential diagnosis.
¿ Conclusion
We report a rare case of a cecal ameboma stressing the importance of a multidisciplinary approach and the effectiveness of medical therapy. This case did not require surgical treatment. Early therapy with anti-parasitic drugs is the cornerstone for avoid complications in patients with ameboma that are diagnosed previous to urgent surgery.
Funding & Acknowledgments:
José Altamirano receives funding from Fundación Bilbao Vizkaya Argentaria (BBVA), Fundació Clinic per a la Reserca Biomedicà, Institut d´Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS) & CIBEREHD, Barcelona, Spain.
Correspondence: José Altamirano, M.D.
Villaroel 170 08036. Barcelona, Spain.
Phone: 3467 1920 419. Fax: 3493 2746 068.
E-mail: dr_altamirano@hotmail.com
Recibido el 10 de mayo de 2010;
aceptado el 06 de julio de 2010.