The standard of care for gallbladder disease is laparoscopic cholecystectomy. Difficult dissection of the hepatocytic triangle and bleeding can result in conversion to open cholecystectomy, which is associated with increased morbidity. Identifying risk factors for conversion in the context of acute cholecystitis will allow patient care to be individualized and improve outcomes.
Materials and methodsA retrospective case-control study included all patients diagnosed with acute cholecystitis, according to the 2018 Tokyo Guidelines, admitted to a tertiary care academic center, from January 1991 to January 2012. Using logistic regression, we analyzed variables to identify risk factors for conversion. Variables that were found to be significant predictors of conversion in the univariate analysis were included in a multivariate model. We then performed an exploratory analysis to identify the risk factor summation pathway with the highest sensitivity for conversion.
ResultsThe study included 321 patients with acute cholecystitis. Their mean age was 49 years (±16.8 SD), 65% were females, and 35% were males. Thirty-nine cases (12.14%) were converted to open surgery. In the univariate analysis, older age, male sex, gallbladder wall thickness, and pericholecystic fluid were associated with a higher risk for conversion. In the multivariate analysis all of the variables, except pericholecystic fluid, were associated with conversion. Our risk factor summation model had a sensitivity of 84%.
ConclusionsPreoperative clinical data can be utilized to identify patients with a higher risk of conversion to open cholecystectomy. Being aware of such risk factors can help improve perioperative planning and preparedness in challenging cases.
El estándar de tratamiento para la enfermedad de la vesícula biliar es la colecistectomía laparoscópica. Una disección del triángulo hepatocístico complicada con sangrado puede resultar en conversión a cirugía abierta durante el procedimiento, la cual se asocia a una mayor morbilidad. La identificación de factores de riesgo por la conversión en el contexto de colecistitis aguda permitirá individualizar el cuidado del paciente y mejorar los resultados.
Materiales y métodosEstudio retrospectivo de casos y controles que incluyó a todos los pacientes admitidos en un centro académico de tercer nivel desde enero de 1991 hasta enero de 2012 con diagnóstico de colecistitis aguda según las guías de Tokio 2018. Analizamos las variables utilizando regresión logística para identificar los factores de riesgo para conversión. Las variables que se identificaron como predictores de conversión significativos en el análisis univariado fueron incluidas en un modelo multivariado. Finalmente realizamos un análisis exploratorio para identificar la sumatoria de factores con mayor sensibilidad para conversión.
ResultadosEl estudio incluyó a 321 pacientes con colecistitis aguda. La edad promedio fue de 49 años (DE: ±16.8). El 65% fueron del sexo femenino y el 35% del sexo masculino. Treinta y nueve casos (12.14%) se convirtieron a cirugía abierta. En el análisis univariado, la mayor edad, el sexo masculino, el grosor de pared vesicular y el líquido pericolecístico se asociaron con un mayor riesgo de conversión. En el análisis multivariado, todas las variables con excepción del líquido pericolecístico mantuvieron asociación con conversión. Nuestro modelo de predicción de riesgo demostró una sensibilidad del 84%.
ConclusionesEs posible utilizar datos clínicos preoperatorios para identificar a pacientes que tienen un mayor riesgo de conversión a cirugía abierta. Conocer dichos factores puede mejorar la planeación del plan quirúrgico y estar preparados para casos desafiantes.
Acute cholecystitis (AC) is an inflammatory process characterized by gallbladder distention, wall thickening, exudate formation, and the presence of pericholecystic fluid. It is associated with cholelithiasis in the majority of cases, but there are other factors that seem to contribute to its pathogenesis, including wall ischemia, motility impairment, direct chemical insults, infection, and connective tissue abnormalities1,2.
An estimated 25 million people in the United States have cholelithiasis, and nearly 20% of them will eventually develop symptoms and complications within their lifetime3.
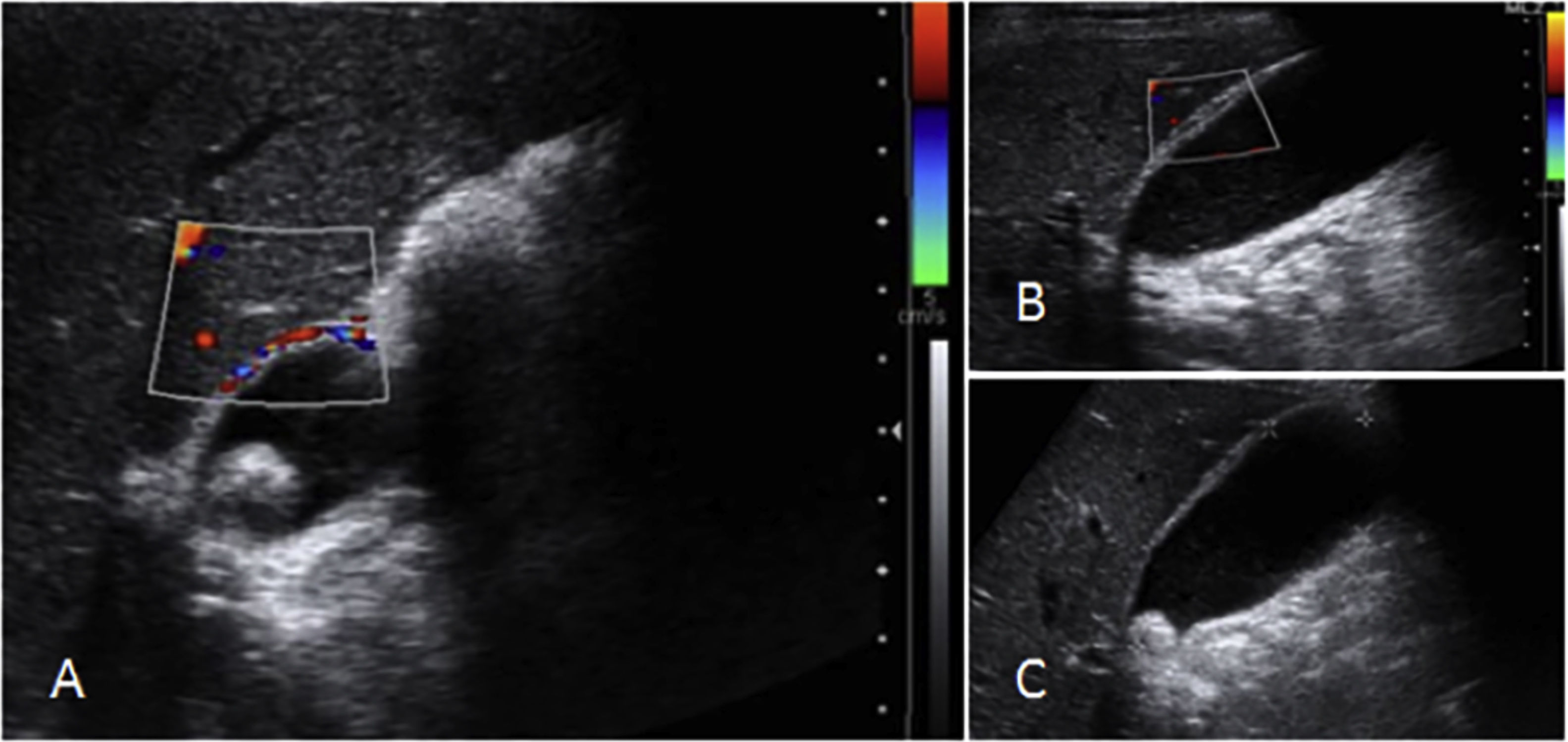
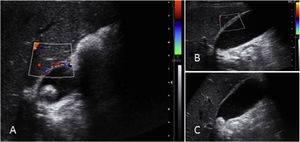
The diagnosis of AC is made utilizing the criteria of the 2018 Tokyo guidelines (TG18), which are composed of a combination of clinical, biochemical, and radiologic parameters. Abdominal ultrasound has proven to be the most cost-effective test (Fig. 1A–C)4, and although a hepatobiliary iminodiacetic acid (HIDA) scan is considered the gold standard, it is not readily available.
Laparoscopic cholecystectomy (LC) is currently the cornerstone treatment for AC. Compared with open cholecystectomy (OC), LC is associated with less morbidity, but in challenging cases, the recommendation is to convert to OC. Different studies have attempted to identify patients that will undergo technically challenging operations and consequently have an increased risk for conversion.
Previous risk prediction models have addressed that issue, but for decades, different diagnostic criteria have been used to differentiate AC from symptomatic cholelithiasis, thwarting the reproducibility of those findings in relation to AC determined according to the TG185.
We sought to create a risk factor prediction model that was able to identify patients at increased risk for conversion, in patients that were diagnosed, following currently utilized criteria.
Materials and methodsData were collected from patients diagnosed with AC that were admitted to a tertiary care academic center in Mexico City, within the time frame of January 1991 to January 2012. The diagnosis of AC fulfilled the TG18 criteria in 100% of the cases, and all the patients underwent LC. Diagnosis was confirmed by histopathologic analysis in all the cases.
Patients with missing information (including ultrasonographic assessment), acalculous cholecystitis, age below 18 years, pregnant women, patients that initially underwent OC, patients that did not fulfill the TG18 criteria, and patients initially treated with percutaneous cholecystostomy were excluded. All patients were consecutively enrolled, to have a representative sample.
The clinical and demographic variables were age, sex, body mass index (BMI), number and type of comorbidities, previous abdominal surgeries, associated cholangitis, and American Society of Anesthesia (ASA) status. The preoperative laboratory data reported hemoglobin, white blood cell differential, platelet count, and liver function test results. Ultrasound variables included the sonographic Murphy’s sign, pericholecystic fluid (defined as the presence of a hypoechoic layer within the gallbladder wall), gallbladder wall width>4mm, and the presence of hepatic steatosis. All ultrasounds were performed and read by certified radiologists from our institution.
Statistical analysisThe statistical analysis was carried out using the IBM® SPSS® Statistics Version 21 (64 bit) for Windows program (Copyright 1989–2012 IBM Corporation and others). The categorical variables were expressed as frequencies and percentages, the quantitative variables with normal distribution were expressed as means and standard deviation, and the quantitative variables with non-normal distribution were expressed as median and ranges. The categorical variables were compared, utilizing the chi-square test, whereas the quantitative variables were compared, utilizing the Student’s t test and the Mann–Whitney U test, depending on distribution type. We performed a univariate logistic regression model to assess the association between the parameters mentioned above and the rate of conversion to open surgery. Variables found to have statistically significant correlation in the univariate model were then included in a multivariate model, according to the category of the variables, and in a final multivariate model that included all the significant variables, regardless of category. We considered a p<0.05 to be statistically significant. Using the risk factors that significantly associated with conversion, we performed a pyramidal exploratory analysis to identify the risk factor summation pathway with the highest sensitivity for conversion.
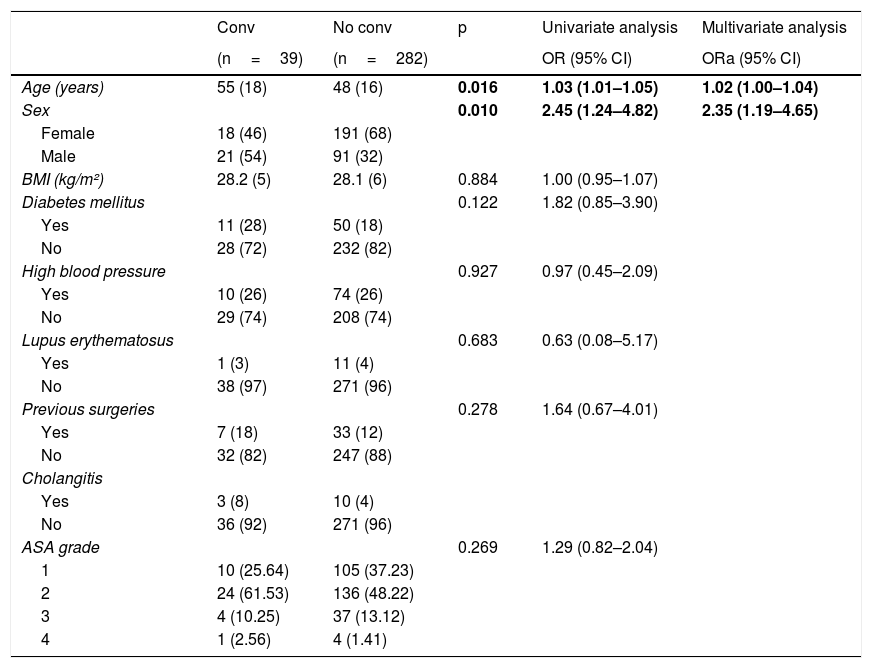
ResultsThree hundred and twenty-one patients were included, 39 (12.14%) of whom underwent conversion to OC. The mean patient age was 49.1 years (±16.8 SD), 209 patients were females (65%), and 112 were males (35%). Patients in the conversion group were significantly older (p=0.016) and there was a higher proportion of males (p=0.010). Table 1 shows the characteristics of the clinical variables. In our logistic regression analysis by variable category, both age and sex were significantly associated with conversion in the univariate and multivariate analyses (univariate: OR 1.03 [95% CI 1.01–1.05]/multivariate: OR 1.02 [95% CI 1.00–1.04] for age; and univariate: OR 2.45 [95% CI 1.24–4.82]/multivariate: OR 2.35 [95% CI 1.19–4.65] for sex).
Patient clinical characteristics.
| Conv | No conv | p | Univariate analysis | Multivariate analysis | |
|---|---|---|---|---|---|
| (n=39) | (n=282) | OR (95% CI) | ORa (95% CI) | ||
| Age (years) | 55 (18) | 48 (16) | 0.016 | 1.03 (1.01–1.05) | 1.02 (1.00–1.04) |
| Sex | 0.010 | 2.45 (1.24–4.82) | 2.35 (1.19–4.65) | ||
| Female | 18 (46) | 191 (68) | |||
| Male | 21 (54) | 91 (32) | |||
| BMI (kg/m²) | 28.2 (5) | 28.1 (6) | 0.884 | 1.00 (0.95–1.07) | |
| Diabetes mellitus | 0.122 | 1.82 (0.85–3.90) | |||
| Yes | 11 (28) | 50 (18) | |||
| No | 28 (72) | 232 (82) | |||
| High blood pressure | 0.927 | 0.97 (0.45–2.09) | |||
| Yes | 10 (26) | 74 (26) | |||
| No | 29 (74) | 208 (74) | |||
| Lupus erythematosus | 0.683 | 0.63 (0.08–5.17) | |||
| Yes | 1 (3) | 11 (4) | |||
| No | 38 (97) | 271 (96) | |||
| Previous surgeries | 0.278 | 1.64 (0.67–4.01) | |||
| Yes | 7 (18) | 33 (12) | |||
| No | 32 (82) | 247 (88) | |||
| Cholangitis | |||||
| Yes | 3 (8) | 10 (4) | |||
| No | 36 (92) | 271 (96) | |||
| ASA grade | 0.269 | 1.29 (0.82–2.04) | |||
| 1 | 10 (25.64) | 105 (37.23) | |||
| 2 | 24 (61.53) | 136 (48.22) | |||
| 3 | 4 (10.25) | 37 (13.12) | |||
| 4 | 1 (2.56) | 4 (1.41) |
For quantitative variables means±standard deviations are shown. For qualitative variables frequencies and percentages are shown. The multivariate analysis included those variables that showed significance in the univariate analysis: sex and age.
CI: confidence interval; Conv: conversion group; No conv: no conversion group; OR: odds ratio; ORa: adjusted odds ratio.
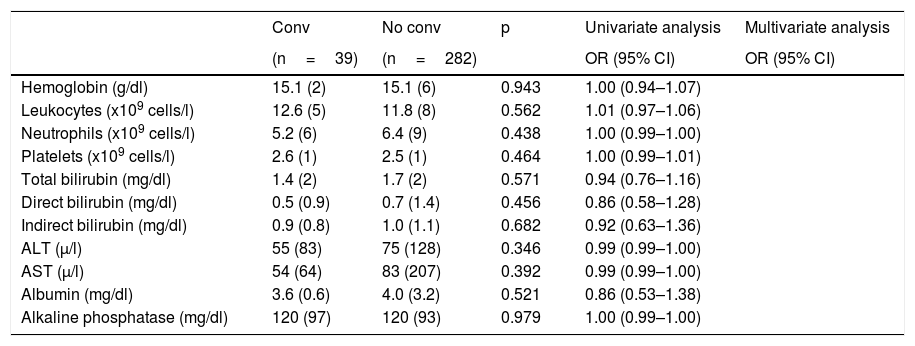
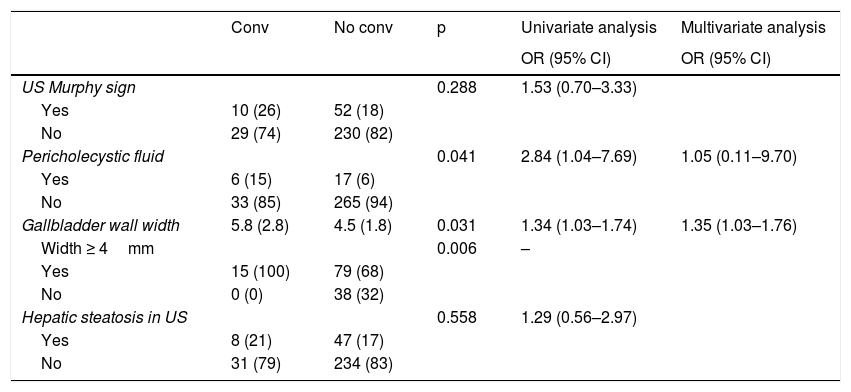
Table 2 shows the laboratory variables. Regarding the laboratory parameters, there were no significant differences between groups or correlations with conversion to open surgery in the logistic regression model. For the ultrasound variables, shown in Table 3, gallbladder wall width was significantly higher in the conversion group (p=0.031). All patients with a wall width >4mm underwent conversion to open surgery and the presence of pericholecystic fluid was also statistically higher in the conversion group (p=0.031). The logistic regression model revealed a significant association with conversion to open surgery for those two variables in the univariate model and solely for wall width in the multivariate analysis by category (univariate: OR 1.34 [95% CI 1.03–1.74]/multivariate: OR 1.35 [95% CI 1.03–1.76] for wall width; and univariate: OR 2.84 [95% CI 1.04–7.69] for pericholecystic fluid).
Laboratory parameters.
| Conv | No conv | p | Univariate analysis | Multivariate analysis | |
|---|---|---|---|---|---|
| (n=39) | (n=282) | OR (95% CI) | OR (95% CI) | ||
| Hemoglobin (g/dl) | 15.1 (2) | 15.1 (6) | 0.943 | 1.00 (0.94–1.07) | |
| Leukocytes (x109 cells/l) | 12.6 (5) | 11.8 (8) | 0.562 | 1.01 (0.97–1.06) | |
| Neutrophils (x109 cells/l) | 5.2 (6) | 6.4 (9) | 0.438 | 1.00 (0.99–1.00) | |
| Platelets (x109 cells/l) | 2.6 (1) | 2.5 (1) | 0.464 | 1.00 (0.99–1.01) | |
| Total bilirubin (mg/dl) | 1.4 (2) | 1.7 (2) | 0.571 | 0.94 (0.76–1.16) | |
| Direct bilirubin (mg/dl) | 0.5 (0.9) | 0.7 (1.4) | 0.456 | 0.86 (0.58–1.28) | |
| Indirect bilirubin (mg/dl) | 0.9 (0.8) | 1.0 (1.1) | 0.682 | 0.92 (0.63–1.36) | |
| ALT (μ/l) | 55 (83) | 75 (128) | 0.346 | 0.99 (0.99–1.00) | |
| AST (μ/l) | 54 (64) | 83 (207) | 0.392 | 0.99 (0.99–1.00) | |
| Albumin (mg/dl) | 3.6 (0.6) | 4.0 (3.2) | 0.521 | 0.86 (0.53–1.38) | |
| Alkaline phosphatase (mg/dl) | 120 (97) | 120 (93) | 0.979 | 1.00 (0.99–1.00) |
For quantitative variables means±standard deviations are shown. For qualitative variables frequencies and percentages are shown. The multivariate analysis included those variables that showed significance in the univariate analysis.
OR: odds ratio.
CI: confidence interval; Conv: conversion group; No conv: no conversion group; OR: odds ratio.
Ultrasound variables.
| Conv | No conv | p | Univariate analysis | Multivariate analysis | |
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | ||||
| US Murphy sign | 0.288 | 1.53 (0.70–3.33) | |||
| Yes | 10 (26) | 52 (18) | |||
| No | 29 (74) | 230 (82) | |||
| Pericholecystic fluid | 0.041 | 2.84 (1.04–7.69) | 1.05 (0.11–9.70) | ||
| Yes | 6 (15) | 17 (6) | |||
| No | 33 (85) | 265 (94) | |||
| Gallbladder wall width | 5.8 (2.8) | 4.5 (1.8) | 0.031 | 1.34 (1.03–1.74) | 1.35 (1.03–1.76) |
| Width ≥ 4mm | 0.006 | – | |||
| Yes | 15 (100) | 79 (68) | |||
| No | 0 (0) | 38 (32) | |||
| Hepatic steatosis in US | 0.558 | 1.29 (0.56–2.97) | |||
| Yes | 8 (21) | 47 (17) | |||
| No | 31 (79) | 234 (83) |
For quantitative variables means±standard deviations are shown. For qualitative variables, frequencies and percentages are shown. The multivariate analysis included those variables that showed significance in the univariate analysis.
CI: confidence interval; Conv: conversion group; No conv: no conversion group; OR: odds ratio; US: ultrasound.
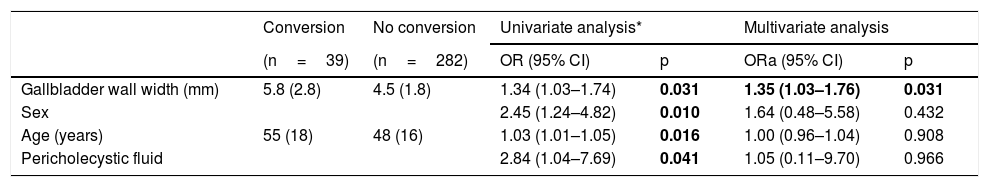
We included all factors that were significantly associated with conversion, regardless of the category of the variable, in a final multivariate model, as shown in Table 4. The only factor that maintained a significantly increased risk for conversion in that model was gallbladder width (OR 1.13, 95% CI 1.03–1.76).
Final logistic regression analysis, independent of variable category.
| Conversion | No conversion | Univariate analysis* | Multivariate analysis | |||
|---|---|---|---|---|---|---|
| (n=39) | (n=282) | OR (95% CI) | p | ORa (95% CI) | p | |
| Gallbladder wall width (mm) | 5.8 (2.8) | 4.5 (1.8) | 1.34 (1.03–1.74) | 0.031 | 1.35 (1.03–1.76) | 0.031 |
| Sex | 2.45 (1.24–4.82) | 0.010 | 1.64 (0.48–5.58) | 0.432 | ||
| Age (years) | 55 (18) | 48 (16) | 1.03 (1.01–1.05) | 0.016 | 1.00 (0.96–1.04) | 0.908 |
| Pericholecystic fluid | 2.84 (1.04–7.69) | 0.041 | 1.05 (0.11–9.70) | 0.966 | ||
For quantitative variables means±standard deviations are shown. For qualitative variables, frequencies and percentages are shown.
CI: confidence interval; OR: odds ratio; ORa: adjusted odds ratio.
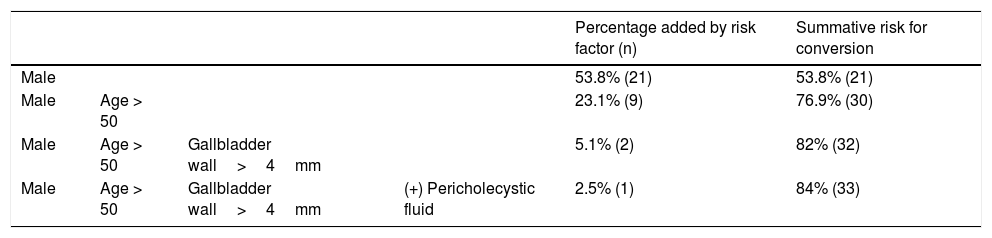
We then performed an exploratory analysis operation in the form of a risk stratification pyramid, through which our risk factor summation pathway with the highest sensitivity for conversion was able to detect 84% of the cases that would be converted. Table 5 shows our risk stratification pyramid.
Individually, male patients required conversion in 21 cases, (sensitivity: 54% and specificity: 68%) and patients with a gallbladder width>4mm required conversion in 39 cases (sensitivity: 100% and specificity: 33%). Grouping risk factors starting from male sex presented a higher summation than grouping factors starting from gallbladder width. With that operation, we corroborated that both sex and age were the main factors in evaluating the risk for conversion, followed by gallbladder width and pericholecystic fluid as additional independent factors.
Discussion and conclusionsIn our study we found that male sex, older ages, increased gallbladder wall width, and pericholecystic fluid were associated with an increased risk of conversion to OC. Prior studies on this subject have described similar findings, but some variables have been inconsistent. A retrospective study from 2007 reported an increased risk for conversion in patients with male sex, leukocytosis, hypoalbuminemia, pericholecystic fluid, type 2 diabetes mellitus, and elevated total bilirubin levels6, whereas in 2014, in a predictive model that analyzed computed tomography parameters, only the presence of pericholecystic fluid revealed a significant correlation with conversion7.
More recently, in a 2017 systemic review by Panni et al., those authors found that the most important reason for conversion was inflammation of the gallbladder wall and that age, male sex, and white blood cell count were consistent predictors throughout the studies analyzed8.
It is worth mentioning that one of the main limitations of prior studies is that they lack clear, definitory criteria for the diagnosis of AC, whereas we utilized the TG18, whose sensitivity and specificity are above 90%9. We believe that it is important to differentiate symptomatic cholelithiasis from AC in such analyses, as the former presents with considerably less inflammation and consequently involves an easier operation, with less chance of conversion. By abiding by the TG18, we also believe that our model results could be more reproducible in different patient populations. In fact, we are currently working on externally validating our results in future projects.
In relation to our study findings, they were concordant with those reported by Panni et al.8, given that our factors associated with conversion were clearly related to an increased amount of inflammation of the wall, which made tissue handling more difficult, and to the fact that the fundus had to be retracted to achieve proper exposure, when looking for the critical view of safety10.
Although the association between older age and conversion to open surgery has already been reported in other studies, it has not been clearly explained. It could be related to the fact that older adult patients often take longer to seek medical attention, and by the time they are seen, their symptoms are more complicated, making surgery more difficult, but data on that subject are still scarce.
We focused on patients diagnosed through abdominal ultrasound, as it is the most widely available imaging study in the majority of low-to-middle-income countries and has good diagnostic efficiency, despite being operator-dependent11. Identifying clinical predictors of conversion for other diagnostic modalities, such as computed tomography (CT), magnetic resonance imaging (MRI), and HIDA scan, is a challenge for the future, as many centers are more frequently utilizing those diagnostic modalities.
Our conversion rate was 12.14%, which concurs with data from other series conducted at teaching hospitals12,13, but that rate is currently decreasing because minimally invasive techniques are becoming more frequently performed worldwide. Current recommendations by the TG18 suggest that the threshold for conversion or bail-out procedures, such as subtotal cholecystectomy, should be very low, in an effort to decrease the rate of iatrogenic bile duct injuries. In the setting of a potentially difficult cholecystectomy, an open approach should at least be considered from the very beginning, especially in the absence of an experienced laparoscopist, or when the primary surgeon is more experienced or comfortable with open interventions.
On the other hand, there are also studies showing that younger and less experienced surgeons may not be as comfortable performing OC14,15, which could affect the outcomes of those patients. Therefore, the decision about the most convenient approach should always be made on an individual basis and dependent on the expertise of the available team. In our experience, the greatest advantage of OC is its improved spatial perception, as well as an improved haptic sensation, which could increase the surgeon's confidence on how to proceed during the cholecystectomy.
Another question that would be interesting to explore is how the experience or technical level of the surgeon (in the case of teaching institutions with residents) correlates with the outcomes of the intervention. Nevertheless, prospective data would be required to address that point.
We found it very helpful to include a graphic, comprehensive representation of our risk factor summation pyramid, showing the added influence of each risk factor on the percentage of cases identified. By ordering such factors by the strength of their association, we identified 84% of cases that underwent conversion.
Lastly, there are several other clinical scenarios that entail difficult cholecystectomies, such as contracted, intrahepatic, and porcelain gallbladders, that could warrant mentioning, but there is very limited evidence of their outcomes in the current literature16–18.
Identifying difficult cases with high risk for conversion could also be useful for detecting patients that are more likely to require an intraoperative cholangiogram (IOC) or common bile duct (CBD) exploration, but again, more studies are needed to support that statement.
The most important limitations of the present study were the fact that the data were retrospective, and the analysis included patients that underwent surgery at a single institution, over a long period of time, during which the learning curve and laparoscopic skills of surgeons have significantly improved.
Regarding the generalizability of our results, they are similar to those reported in the literature worldwide. Nevertheless, we are currently working on validating our predictive model for conversion in a multicenter database.
In conclusion, patients above 50 years of age, males, those with gallbladder wall thickening, and ultrasound-identified pericholecystic fluid have a higher risk for conversion to OC. The sensitivity of our risk factor summation pathway was 84%.
Ethical considerationsNo written consent was needed for the present study due to its retrospective design.
The study complies with all current bioethical research regulations, was approved by the Institutional Review Board, and was carried out, according to the principles of the Declaration of Helsinki. The authors declare that this article does not contain personal information through which any of the patients can be identified.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank the surgery department of their institution for making the present work possible.
Please cite this article as: Morales-Maza J, Rodríguez-Quintero JH, Santes O, Aguilar-Frasco JL, Romero-Vélez G, Sánchez García-Ramos E, et al. Conversión de colecistectomía laparoscópica a abierta: análisis de factores de riesgo con base en parámetros clínicos, de laboratorio y de ultrasonido. Revista de Gastroenterología de México. 2021;86:363–369.