Inflammatory bowel disease (IBD) is a group of chronic intestinal disorders that trigger prolonged inflammation of the digestive tract. Its incidence and prevalence appear to be increasing in the African population and in Egypt. The present study aims to highlight the pattern and management of IBD in Egyptian patients.
Materials and methodsTwo hundred patients with IBD were assessed for ulcerative colitis (UC), through the Mayo score, and for Crohn’s disease (CD), with the Crohn’s disease activity index (CDAI).
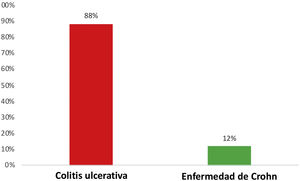
ResultsMedian patient age was 35 years, with a predominance of females. UC was more common than CD (88% and 12%, respectively) and severity was moderate, in the majority of cases. Most UC patients had left-sided lesions, whereas ileitis was the most common finding (37.5%) in the CD patients. Proctitis was the least common finding in both diseases and Crohn’s fistulizing disease was detected in 4.1% of the patients. Interestingly, peripheral arthropathy was the most common extraintestinal manifestation in the IBD patients (70%) and axial arthropathy was the least common (6%). Severe ocular or mucocutaneous involvement was very rare. Finally, biologic treatment was prescribed to 15.4% of the UC patients and 20.8% of the CD patients.
ConclusionsAlthough the clinical presentation of IBD in Egypt is comparable to that reported worldwide, diagnoses were found to be delayed. There were fewer cases of CD than UC, but more mild-to-moderate disease severity. The surveillance of patients with IBD must continue and awareness of the disease in the Egyptian medical community needs to increase. A national registry must be established, multicenter studies need to be conducted, and molecular diagnostics is recommended.
La enfermedad inflamatoria intestinal (EII) es un grupo de trastornos intestinales crónicos que detonan una prolongada inflamación del conducto digestivo. Su prevalencia e incidencia parecen estar creciendo en la población africana y en Egipto. El presente estudio pretende señalar el patrón y manejo de la EII en pacientes egipcios.
Materiales y métodosDoscientos pacientes con EII fueron evaluados por colitis ulcerativa crónica idiopática (CUCI), con la escala de Mayo, y por enfermedad de Crohn (EC), con el índice de actividad de la enfermedad de Crohn (Crohn’s disease activity index [CDAI]).
ResultadosLa edad promedio de los pacientes fue de 35 años, con predominancia de mujeres. La CUCI fue más común que la EC (88% y 12% respectivamente), y la gravedad fue moderada en la mayoría de los casos. La mayoría de los pacientes con CUCI tuvieron lesiones izquierdas, mientras que la ileítis fue el hallazgo más común (37.5%) en los pacientes con EC. La proctitis fue el hallazgo menos común en ambas enfermedades, y se detectó enfermedad de Crohn fistulante en 4.1% de los pacientes. De manera interesante, la artropatía periférica fue la manifestación extraintestinal más común en los pacientes con EII (70%) y la artropatía axial fue la menos común (6%). La afectación ocular grave o mucocutánea fue muy rara. Finalmente, se prescribió tratamiento biológico a 15.4% de los pacientes con CUCI y 20.8% de los pacientes con EC.
ConclusionesAunque la presentación clínica de la EII en Egipto es comparable a la reportada a nivel mundial, se encontró que los diagnósticos fueron tardíos. Se encontraron menos casos de EC que de CUCI, pero con mayor gravedad de leve a moderada. La vigilancia de los pacientes con EII debe continuar y el conocimiento de la enfermedad en la comunidad médica egipcia debe crecer. También es importante establecer un registro nacional, realizar estudios multicentro, y se recomienda hacer diagnósticos moleculares.
Inflammatory bowel disease (IBD) is a group of chronic inflammatory conditions of the digestive system. The cause of the disease is unknown, and it commonly requires lifelong care. IBD can result in significant morbidity, but it is not generally associated with increased mortality. Most patients are able to live normal productive lives. In the long-term, up to 75% of patients with Crohn’s disease (CD) and 30% of those with ulcerative colitis (UC) may require surgery1. The incidence and prevalence of IBD appears to be increasing in the African population and in Egypt2–4.
IBD is a complex and costly disease due to its unpredictable relapsing and remitting course, complications, hospitalizations, surgeries, and the use of expensive therapies. Thus, the steady increase in the prevalence of IBD will lead to a substantially increased burden on healthcare systems. As a lifelong disease with no cure, the compounding prevalence of IBD is due to the disparity between incidence and mortality5. An exaggerated immune response to antigenic stimulation by the gut microbiota, in a background of genetic susceptibility, is thought to drive the inflammatory process6. Environmental factors, genetic predisposition, and a dysregulated immune response may strongly increase the risk for developing IBD7.
The aim of the present study was to provide information on the pattern and management of IBD in Egyptian patients.
Materials and methodsThe study included 200 patients with IBD recruited from the IBD Clinic at the National Hepatology and Tropical Medicine Research Institute (NHTMRI) in Cairo, Egypt, within the time frame of December 2017 and April 2019. The study was approved by the Research Ethics Committees of the NHTMRI and the Faculty of Medicine, Cairo University.
A history of sociodemographic characteristics, including consanguinity and similarly affected family members, as well as a medical history including tonsillectomy, appendectomy, the use of oral contraceptives, smoking, and hospital admissions were collected for each patient. The clinical severity of UC and CD was determined using the Mayo score and the Crohn's disease activity index (CDAI), respectively8–11 (Table 1). The following laboratory tests were carried out: complete blood count (CBC), C-reactive protein (CRP), fecal calprotectin, erythrocyte sedimentation rate (ESR), and serum bilirubin (Table 2). Patients underwent colonoscopy and tissue samples were assessed through histopathologic examination.
The gastrointestinal symptoms of the patients.
| Symptoms | Ulcerative colitis | Crohn’s disease | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Abdominal pain | 92 | 52.3 | 12 | 50 | .834 |
| Fecal urgency | 54 | 30.7 | 5 | 20.8 | .321 |
| Blood and mucous in stools | 44 | 25 | 5 | 20.8 | .463 |
| Constipation | 37 | 21 | 7 | 29.2 | .366 |
| Bloating | 98 | 55.7 | 13 | 54.2 | .889 |
| Rectal bleeding | 53 | 30.1 | 9 | 37.5 | .463 |
| Diarrhea | 72 | 40.9 | 6 | 25 | .134 |
| Frequency | |||||
| Mild | 33 | 18.8 | 2 | 8.3 | .289 |
| Moderate | 12 | 6.8 | 0 | 0.0 | |
| Severe | 19 | 10.8 | 3 | 12.5 | |
| No diarrhea | 112 | 63.6 | 19 | 79.2 | |
The laboratory test results of the patients.
| Laboratory tests | Ulcerative colitis | Crohn’s disease | Normal value | p |
|---|---|---|---|---|
| Median (IQR) | Median (IQR) | |||
| Calprotectin, μg/dl | 465 (475) | 667.5 (886) | <50 | .299 |
| Hemoglobin, g/dl | 12 (2) | 12 (3) | 11.6−16.6 | .569 |
| Leukocytes, 109/l | 8(4) | 6.9 (4) | 3.4−9.6 | .517 |
| Platelets, 109/l | 279 (73) | 279 (92) | 135−371 | .467 |
| Hematocrit, 109/l | 35 (7) | 34 (8.7) | 35.5−38.6 | .899 |
| CRP mg/l | 12 (19) | 24 (19) | <10 | .538 |
| ESR mm/hour | 54 (92) | 54 (57) | Females 0−22 | 1.0 |
| Males 0−29 |
CRP: C-reactive protein; ESR: erythrocyte sedimentation rate; IQR: interquartile range.
All the statistical analyses were performed using the SPSS version 21 for Windows (SPSS Inc) program. The Kolmogorov–Smirnov test of normality was employed to validate whether the distribution of variables followed a Gaussian pattern. The normally distributed data in the groups were expressed as mean ± SD and the non-normally distributed data were presented as median and interquartile range (IQR). For the continuous variables, the differences between the two groups were evaluated using the Mann–Whitney U test. All tests were two-sided, and statistical significance was set at a p < 0.05.
Ethical considerationsInformed consent was requested from the patients to receive the treatment and participate in the research. In the case of the underage patients, their parents or guardians provided the informed consent. The present research complies with the current regulations of the Research and Ethics Committees of the NHTMRI and the Faculty of Medicine, Cairo University. The authors declare that this article contains no personal information that could identify the patients.
ResultsThe age of the patients included in the study ranged from 19 to 73 years (mean 31.5 ± 20), with a predominance of females (female/male ratio, 1:0.56). UC (88%) was more common than CD (12%) (Fig. 1). The sociodemographic comparison between UC and CD showed that patients with CD were significantly younger than patients with UC (median and IQR values were 31 vs 36, respectively, [p = 0.03]). Regarding the past history of the patients with UC and CD, more patients with CD had undergone tonsillectomy (33.3% vs 14.1%, respectively, p = 0.01). There was a family history of UC in 6.8% of the patients with UC, whereas none of the patients with CD had a family history of CD. The endoscopic findings are presented in Table 3. The histologic findings of the study groups were evaluated, as described by DeRoche et al.12 Most of the UC specimens were mild (59.7%), with the lamina propria expanded by lymphocytes and plasma cells, the surface/crypt epithelium infiltrated by neutrophils, and/or crypt abscesses in less than 50% of the crypts. In moderately active cases (25.28%), cryptitis and crypt abscesses involved more than 50% of the crypts. Severely active cases (14.9%) were defined by the presence of erosion or ulceration. Regarding the CD specimens, granuloma was found in 9.5% of the patients. The extraintestinal manifestations are presented in Table 4. The clinical severity of UC and CD was assessed by the Mayo score and the CDAI, respectively (Tables 5 and 6).
Regarding medication use in our study, steroids were employed more in the UC patients than in the CD patients. Biologic treatment was prescribed to 15.4% of the UC patients and 20.8% of the patients with CD. Finally, 12.5% of the patients were hospitalized, and 5.5% underwent surgery. A total of 2.5% of the surgical patients had stoma placement and 3% were operated on for treatment of CD.
Discussion and conclusionsIn the present study, patient age ranged from 19 to 73 years (mean 31.5 ± 20), with an IQR of 17 years. Patients with CD were significantly younger than those with UC (the median and IQR values were 31 vs 36, respectively, p = 0.03). That finding concurs with the results of a 2016 Canadian study that included 34,819 patients, 19,713 of whom had CD and 14,683 of whom had UC. Those authors reported that patients with CD were more likely to be younger at diagnosis13. The age of disease onset appears to vary between patients with UC and CD14. Around 25% of patients with IBD are diagnosed within the first two decades of their lives15. However, younger populations in urban industrialized societies are usually more affected16. In our cohort, females predominated. Studies from different countries vary in their findings, regarding the association between sex and IBD. A Malaysian study on IBD reported a predominance of males, whereas an Iranian study reported a predominance of females in UC and males in CD17,18. A predominance of males has also been reported in China, Japan, and Korea, in relation to CD19–21. On the other hand, the female/male ratio of UC was nearly equal in Saudi Arabia22.
In our study, IBD was more common in urban residents. That coincides with the findings of previous investigators who stated that the urbanization and industrialization of societies are associated with changes in microbial exposures, sanitation, occupations, diet, lifestyles, medications, and pollutant exposures, all of which have been implicated as potential environmental risk factors for IBD23.
The results of our study, with a time frame of a little over two years, showed that more patients were diagnosed with UC (88%) than with CD (12%). A previous study, with a time frame of 15 years (1995–2009), was conducted in Cairo on a total of 157 patients with IBD, 135 of whom were diagnosed with UC (86%) and 22 with CD3.
The similarity of the UC/CD ratios between our study and that of the Cairo group described above, despite the differences in the time period of diagnoses and recruitment, could be due to the increasing medical and public awareness of IBD and the improvement in its diagnostic methods in Egypt. Worldwide findings have shown comparable findings, but there was a 6-fold increase in UC in our study, whereas a 2-fold increase has been reported in Europe. Likewise, Asia and some Middle Eastern countries have shown a slight increase in UC patients. Inversely, more patients with CD than with UC have been reported in North American studies17,24,25.
IBD is a complex disease whose endoscopic characterization is based on its mucosal features that aid in determining disease extent and activity. The mucosal changes are seen within a particular anatomic distribution of the colon or the small bowel. Colonoscopic evaluation of the mucosa is crucial to assessing disease activity and consequently prescribing the therapy targeted at particular segments of the colon26.
Regarding UC, most of our patients had left-sided lesions (57.8%) and the fewest presented with proctitis (18.6%). Newly diagnosed cases of UC have been reported to be confined to the rectum and the rectosigmoid colon27,28. In another study, 20–30% of patients with UC had left-sided colitis26. In our patients with CD, ileitis was the most common (37.5%) presentation, followed by extensive colitis and left-sided lesions (25%), whereas proctitis and fistulizing disease were the least common (8.3% and 4.1%, respectively). In a previous study, inspection of the terminal ileum was emphasized as being sufficient to confirm the diagnosis of CD in most patients29,30.
According to the Mayo score, the majority of our UC patients presented with a moderate degree of activity, whereas severe activity was the least common. The endoscopic results of a multicenter European study revealed that 44.3% of patients had moderate-to-severe activity31. Most of the CD patients in our study had moderate activity (60%). Only one case presented with severe activity (6.7%), according to the CDAI. Likewise, previous research has shown that the majority of patients have mild-to-moderate activity24,32.
In our study, the patients with UC had a higher incidence of diarrhea (40.9%) than the patients in the CD group (25%). Previous investigations reported an increase in the frequency of loose/watery bowel movements in UC (80%), compared with CD (60.3%), which could be related to environmental factors or the type of diet in the different populations33,34. Furthermore, the frequency of diarrhea in IBD patients differs, depending on the site and magnitude of intestinal inflammation.
Consequently, understanding the molecular mechanisms leading to diarrhea in IBD is important for proper diagnosis and management35. High calprotectin levels seen in CD could be due to colonic involvement or they could be an indication of high recurrence risk or poor treatment efficiency36.
Steroid use in the patients in the present study was slightly higher in the UC patients than in the CD patients, coinciding with the results of a previous study, in which excess steroid exposure was more common in patients with UC, compared with patients with CD37. Biologic treatment was prescribed to 15.4% of our UC patients, and 20.8% of those with CD. Other studies describe a higher prescription of biologic treatments for CD vs UC38,39. Our results could reflect the national protocol that approves one or two cycles of conventional therapy, followed by laboratory and colonoscopy assessment for a period ranging from 6 months to one year, before switching to biologic treatment.
The prevalence of IBD-related extraintestinal manifestations (EIMs) remains controversial, with various estimates dependent on geographic region, definitions, and exclusion criteria. EIMs most often affect the joints (peripheral and axial arthropathy), skin (erythema nodosum, pyoderma gangrenosum, aphthous stomatitis, and psoriasis), eyes (episcleritis, uveitis), and the hepatobiliary tract (primary sclerosing cholangitis)40. In a cohort of IBD patients with EIMs, approximately 63% presented with one manifestation and 27% presented with two41.
Peripheral arthropathy was the most common EIM (70%) in our study. Comparably, previous studies described peripheral arthropathies as the most common EIM40,42. Axial arthropathy occurs in 3–5% of patients with IBD42,43. In the present study, axial arthropathy was the least common EIM (6%). Thirty-two percent of our patients experienced mucocutaneous involvement. One case suffered from extensive psoriasis and the others presented with aphthous stomatitis. Approximately 16% of our patients had mucocutaneous EIMs43.
In conclusion, even though the clinical presentation of IBD in Egypt is comparable to that reported worldwide, the diagnoses in our study patients were delayed, with lower numbers of CD, but more mild-to-moderate disease severity. The surveillance of patients with IBD must continue and awareness of the disease in the Egyptian medical community needs to increase. A national registry must be established, multicenter studies need to be conducted, and molecular diagnostics is recommended.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
AuthorshipKamal A. El-Atrebi: concept, drafting, and design of the study, Eman Taher: data analysis and interpretation, Fayrouz Hamed El Aguizy: data acquisition and interpretation, Rahma M. Ali: participated in the study concept and design, Aza Hegazy: performed the pathologic studies, Mohammed M. El-Sayed: data analysis and interpretation, Basem Eysa: examination of patients and interpretation of data, Ahmed A. El-Atreby: examination of patients and interpretation of data, Aliaa A. Mohammed: data analysis and interpretation, Hala T. El-Bassyouni: drafting and revision the manuscript.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: El-Atrebi KA, Taher E, El Aguizy FH, Ali RM, Hegazy A, El-Sayed MM, et al. Estudio descriptivo de la enfermedad inflamatoria intestinal en un centro de atención terciario egipcio. Rev Gastroenterol Méx. 2023;88:12–18.