Colonoscopy is considered a procedure with a low risk for complications. The most common of the severe complications are perforation and bleeding1. Acute cholecystitis is a rare complication that should be suspected when there is fever and abdominal pain. We present herein a case of acute cholecystitis after colonoscopy.
A 77-year-old man had a past medical history of adenocarcinoma of the rectum (T3N2M0), diagnosed in March 2004, and was treated through anterior resection of the rectum and adjuvant chemotherapy. A metachronous adenocarcinoma (T1N1aM0) at the splenic flexure was detected in a control colonoscopy in June 2016 and was treated through left hemicolectomy and adjuvant chemotherapy. Follow-up was disease-free.
In March 2021, a follow-up colonoscopy was performed that was well tolerated, with no need for sedative-analgesic medication. A 2 mm sessile polyp (Paris Is) was identified in the fundus of the cecum, with no other findings. The polyp was extirpated with a biopsy forceps and the histology study reported tubular adenoma with low-grade dysplasia.
On post-colonoscopy day one, the patient presented with abdominal pain located in the right hypochondrium and epigastrium, together with abdominal distension. Seventy-two hours after the colonoscopy, he presented with fever of 38 °C and increased abdominal pain, causing him to go to the emergency department. Physical examination revealed low blood pressure (BP: 99/63 mmHg) and a positive Murphy sign. Laboratory work-up showed signs of sepsis, with important elevation of the inflammatory parameters (CRP 402 mg/l, PCT 2.5 ng/mL, leukocytosis of 21,000/mm3 with left shift), acute kidney function deterioration (creatinine 1.5 mg/dl and GFR 43 mL/min), worsened hemostasis (IQ: 63%, INR 1.32), elevated lactate (3.3 mmol/l) and liver function tests within normal limits (total bilirubin 1.08 mg/dl, AST/ALT: 13/9 U/l).
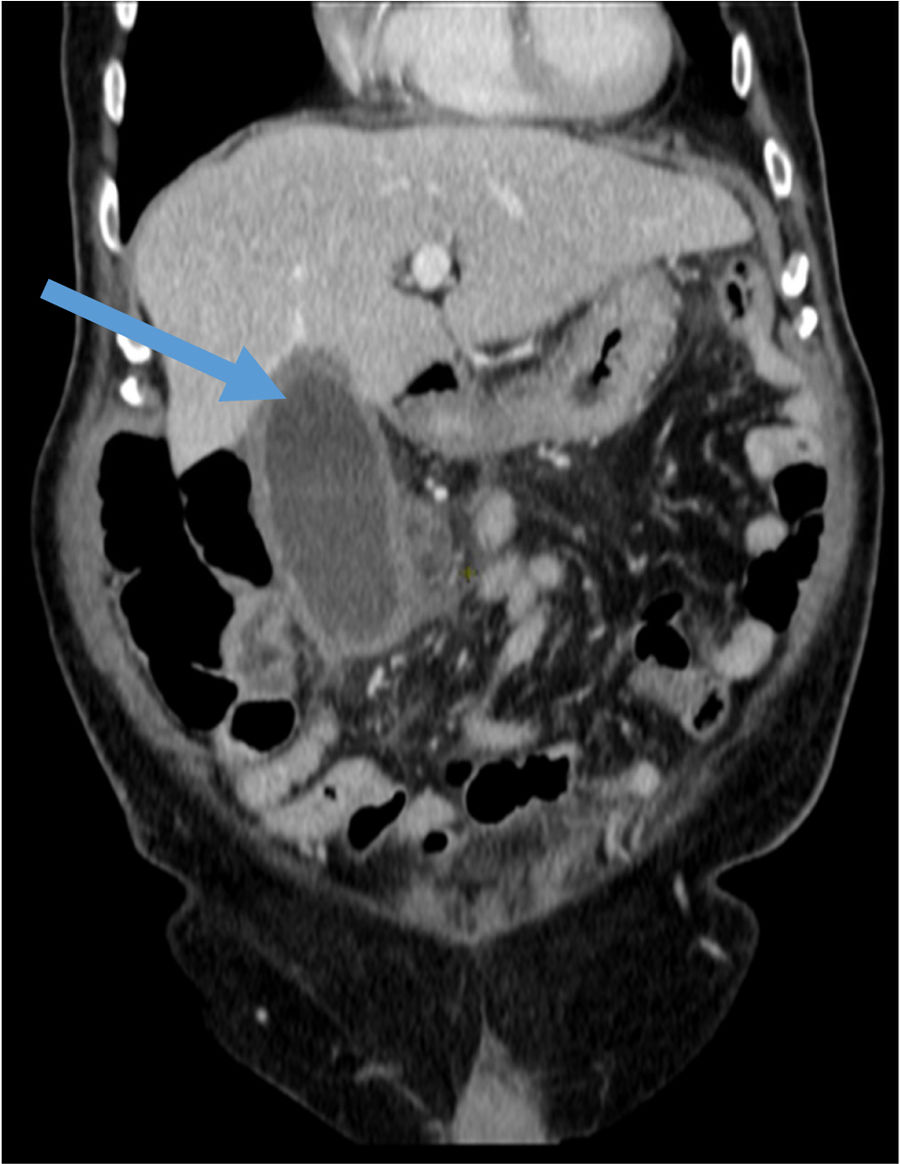
Given the clinical and laboratory findings, an intravenous contrast-enhanced abdominal and pelvic computed tomography (CT) scan was carried out, with findings of acute cholecystitis and no identification of pneumoperitoneum or abdominal free fluid (Fig. 1).
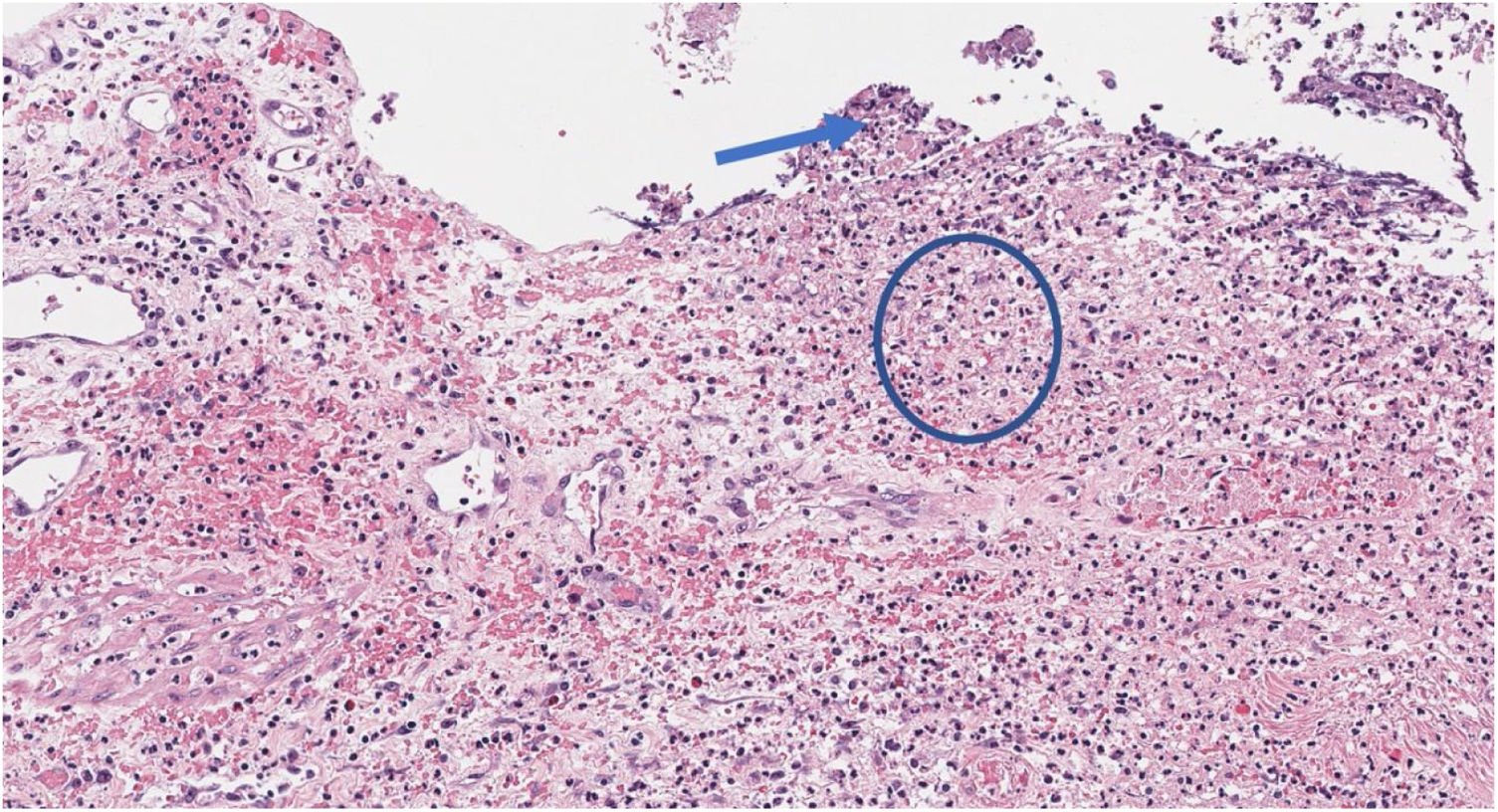
Emergency laparoscopic cholecystectomy was performed, with intraoperative findings of gangrenous cholecystitis, a large gallbladder, and marked adhesion of the gallbladder to the omentum and segments of the small bowel and colon. The pathology study of the surgical specimen reported ulcerative, phlegmonous acute cholecystitis (Fig. 2) with gallstones in the interior. Postoperative progression was satisfactory, with adequate progressive oral tolerance and reestablished bowel transit. The patient was released 48 h after the intervention and outpatient controls have been good.
Currently, 14 cases of post-colonoscopy acute cholecystitis have been described. Various hypotheses on its etiopathogenesis have been suggested, but the exact mechanism by which the entity is produced cannot be established by the evidence based on case series2. The relative dehydration caused by bowel preparation can cause biliary stasis, increasing the risk for a local inflammatory reaction3. Those changes can favor the impaction of a pre-existing gallstone in the neck of the gallbladder or in the cystic duct3,4. In fact, the majority of reported cases, like ours, presented with concomitant gallstones. Other possible mechanisms are bacterial translocation due to enteric pathogens and the trauma or inflammatory response after polypectomy3–6.
Our patient underwent colonoscopy and had no immediate complications. He developed cholecystitis within the first 72 h following the procedure. All the presently described cases of post-colonoscopy cholecystitis have occurred within that same time frame.
Therefore, we presented herein a rare case of acute cholecystitis after colonoscopy and a review of the literature. Our case supports the presentation pattern of the entity within 72 h following the procedure, as well as the hypothesis of a possible increase in lithogenesis as a pathophysiologic mechanism. Even though perforation and bleeding are the most frequent severe complications, the present case emphasizes the need to consider acute cholecystitis in the differential diagnosis of abdominal pain and fever after colonoscopy.
Ethical considerationsThe authors declare that this article contains no personal information that can identify the patient.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ladrón Abia P, Mínguez Sabater A, García-Campos M, Del Hoyo F. Colecistitis aguda tras colonoscopia: Una complicación infrecuente. Rev Gastroenterol Méx. 2022;87:491–492.