Blue rubber bleb nevus syndrome (BRBNS) is characterized by the forming of multiple vascular malformations and hemangiomas that compromise different organs of the body, mainly the skin and digestive tract.1 Gastrointestinal BRBNS is a rare disease, with fewer than 100 cases reported in the literature.2 The small bowel is the most affected region in the digestive tract, followed by the colon.3 It manifests as gastrointestinal bleeding and severe anemia.4 BRBNS is usually diagnosed at birth or in the pediatric age range, but it can begin in adulthood.5 We present herein 2 cases of gastrointestinal BRBNS diagnosed through capsule endoscopy (CE) in geriatric patients (> 65 years of age).
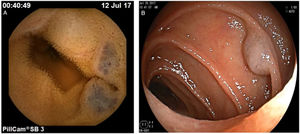
The first case was a 68-year-old woman with a history of osteoarthrosis and nonsteroidal anti-inflammatory drug (NSAID) use, mainly ketorolac and diclofenac, at least 5 times per week over the past 6 months. The patient presented with melenic stools and a decrease in hemoglobin to 9g/dl, for which she underwent gastroscopy and colonoscopy on 2 occasions, without identifying the bleeding site. CE was performed that revealed multiple hemangiomas in the jejunum, measuring 3–8mm in diameter. Anterograde double-balloon enteroscopy (DBE) was carried out, with argon plasma coagulation (APC) of the identified lesions (Fig. 1). The patient remained asymptomatic for 3 months, when she presented with gastrointestinal bleeding. She underwent a repeat anterograde DBE with APC of the observed lesions and the largest lesion (8mm) was removed by loop resection. The patient modified her analgesic regimen, utilizing paracetamol, instead of an NSAID. During the one-year follow-up she has not presented with bleeding or anemia.
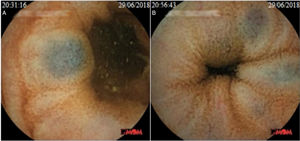
The second case was an 80-year-old man that had a history of infra-renal aortic aneurysm, measuring 7.5cm in diameter, and left gonarthrosis, under treatment with meloxicam for 2 months. The patient presented with melenic stools and symptoms of anemia associated with a decrease in hemoglobin to 10g/dl (baseline hemoglobin 14.9g/dl). Gastroscopy and colonoscopy were performed, without identifying the cause of bleeding. CE was then carried out and showed multiple hemangiomas, measuring 4–6mm in diameter, located in the proximal jejunum, with no signs of active bleeding (Fig. 2). Given the size of the aortic aneurysm, DBE was not performed. NSAIDs were suspended and follow-up with hemogram was conducted for 6 months, with no new bleeding events, and the patient’s hemoglobin level normalized.
A systematic review that included 120 patients with BRBNS showed that only 4% of the patients presented with the disease in adulthood but did not state whether they were geriatric cases. The oldest patient reported was 82 years old at the time of diagnosis.6 The 2 patients described herein presented with BRBNS as older adults. In both cases, the hemangiomas observed were smaller than those seen by the authors in pediatric patients. Another relevant datum is that both patients were taking NSAIDs before the bleeding event. The smaller size of the hemangiomas could have contributed to their late presentation, with NSAID use the potential trigger for bleeding. CE is a useful tool for diagnosing patients with gastrointestinal BRBNS.7
Ethical disclosuresThe authors declare that no experiments were performed on humans or animals for this study. Informed consent was obtained and is in the possession of the corresponding author. The authors have followed the protocols of their work center in relation to the publication of patient data, preserving patient confidentiality and anonymity at all times. Because the study had a retrospective design that included the review of case records of patients that underwent capsule endoscopy, approval of the study protocol by the corresponding ethics committee was not necessary.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Blanco-Velasco G, Zamarripa-Mottú R, Solórzano-Pineda OM, Murcio-Pérez E, Hernández-Mondragón OV. Síndrome de blue rubber-bleb nevus en pacientes geriátricos. Revista de Gastroenterología de México. 2020;85:215–216.