Report our experience in the diagnosis and treatment of Boerhaave syndrome by retrospective study from 1997 to 2013.
Patients and methodsA retrospective study was conducted covering the time frame of 1997 to 2013.
ResultsThere were a total of 5 men (71%) and 2 women (29%) and the mean age was 54 years (range: 33-80 years). Diagnosis was made through computed tomography scan in 5 cases (71%) and esophagogram in 2 cases (19%). Six patients (86%) had emergency surgery, whereas one case (14%) was managed conservatively. The surgical technique employed was primary suture and repair in 4 patients (67%) and esophageal resection and subsequent cervical esophagostomy in 2 patients (33%).
ConclusionsBoerhaave's syndrome is a clinically rare entity with an elevated mortality rate. Therefore, a high degree of suspicion is necessary for making the diagnosis and providing early treatment that can result in improved outcome.
Comunicar nuestra experiencia en el diagnóstico y tratamiento en el síndrome de Boerhaave mediante estudio retrospectivo desde 1997 hasta 2013.
Pacientes y métodosEstudio retrospectivo desde 1997 hasta 2013.
ResultadosEn total, 5 varones (71%) y 2 mujeres (29%). Media de edad de 54 años (rango 33-80). Se llegó al diagnóstico mediante tomografía computarizada en 5 casos (71%) y esofagograma en 2 casos (19%). Seis pacientes (86%) se intervinieron de forma urgente, mientras que en un caso (14%) se optó por actitud conservadora. La técnica quirúrgica empleada fue la sutura primaria y plastia en 4 pacientes (67%) y la resección esofágica y posterior esofagostoma cervical en 2 pacientes (33%).
ConclusionesEl síndrome de Boerhaave es una entidad clínica poco frecuente con una elevada mortalidad. Por ello, debe tenerse un alto nivel de sospecha clínico, con el objetivo de un diagnóstico y tratamiento precoz, mejorando de este modo el pronóstico.
Boerhaave's syndrome was first described in 1724 by Hermann Boerhaave, upon witnessing a man's death as a consequence of spontaneous esophageal perforation after the effort of vomiting. This perforation is generally located at the level of the inferior third of the esophagus, on the left side, some 3-5cm from the gastroesophageal junction. Its etiology involves a sudden increase in the intraesophageal pressure. The classic clinical symptoms are vomiting, chest pain, and subcutaneous emphysema, known as Mackler's triad. However, this combination of symptoms is not always identifiable, representing a diagnostic challenge.1–3 Despite the advances in surgery, anesthesia, and postoperative care over the last 20 years, the morbidity and mortality figures are still high.4 Therefore, there must be a high level of clinical suspicion for making the diagnosis and providing early treatment and thus improving the outcome.
The aim of the present study was to communicate our experience in the management of Boerhaave's syndrome, evaluating the different strategies employed.
MethodsA retrospective study was conducted of patients diagnosed with Boerhaave's syndrome in our center within the time frame of October 1997 and February 2013. The inclusion criteria were: patients with spontaneous esophageal perforation, above the age of 14 years, with or without surgical intervention. The exclusion criteria were: esophageal perforations due to other causes and patients under 14 years of age.
The variables analyzed were: age, sex, triggering factors, risk factors, clinical manifestations, length of time from symptom onset to diagnosis, complementary tests, perforation location and size, therapeutic decision, type of approach, surgical technique, surgical complications, intensive care unit (ICU) stay, postoperative hospital stay, and survival.
For the descriptive analysis of the different variables, frequency percentages were used for the qualitative variables and measures of central tendency for the quantitative variables.
ResultsDuring the 16 years of the study, 7 patients were diagnosed with Boerhaave's syndrome; 5 men (71%) and 2 women (29%) with a mean age of 54 years (range 33-80). Symptoms in all of them began with intense abdominal pain. One of the patients was awakened by the pain and it appeared after ingestion in 3 other patients. In 2 patients the clinical manifestation was initially catalogued as pneumonia because it was associated with respiratory symptoms. And the last case studied presented as sepsis originating in the abdomen.
Four cases (57%) had early diagnosis (< 24hours after symptom onset), whereas the other 3 cases (43%) had late diagnosis.
In regard to the diagnostic tests, a chest x-ray was taken in all the cases, detecting left pleural effusion in 6 cases (86%) and bilateral pleural effusion in one case (14%). The definitive diagnosis was reached through computerized tomography (CT) scan in 5 cases (71%), and esophagogram in 2 cases (19%). Perforation location was thoracic in 3 cases (43%) and abdominal in 4 cases (57%). The size of the perforation was<3cm in 3 cases (43%) and>3cm in 4 cases (57%).
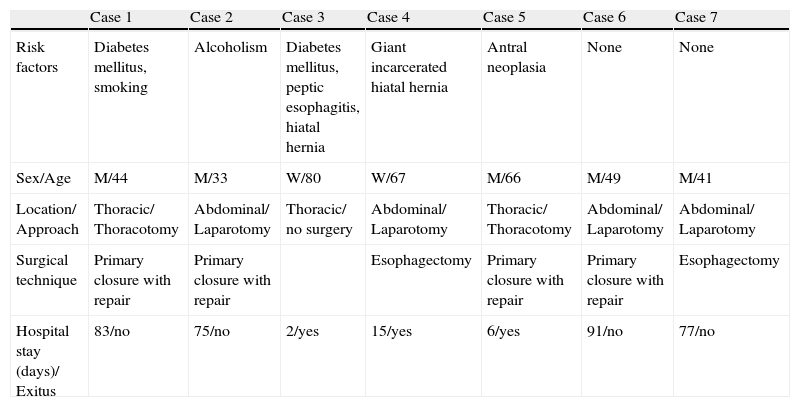
The clinical characteristics of the study sample, risk factors, perforation location, type of approach, and surgical technique employed are shown in Table 1.
Clinical characteristics of the patients.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
| Risk factors | Diabetes mellitus, smoking | Alcoholism | Diabetes mellitus, peptic esophagitis, hiatal hernia | Giant incarcerated hiatal hernia | Antral neoplasia | None | None |
| Sex/Age | M/44 | M/33 | W/80 | W/67 | M/66 | M/49 | M/41 |
| Location/ Approach | Thoracic/ Thoracotomy | Abdominal/ Laparotomy | Thoracic/ no surgery | Abdominal/ Laparotomy | Thoracic/ Thoracotomy | Abdominal/ Laparotomy | Abdominal/ Laparotomy |
| Surgical technique | Primary closure with repair | Primary closure with repair | Esophagectomy | Primary closure with repair | Primary closure with repair | Esophagectomy | |
| Hospital stay (days)/ Exitus | 83/no | 75/no | 2/yes | 15/yes | 6/yes | 91/no | 77/no |
In relation to treatment, 6 patients (86%) had emergency surgery, whereas one case (14%) was managed conservatively. All the patients that were operated on were admitted to the ICU for postoperative control. The patient that did not undergo surgery was controlled in the General and Digestive Surgery ward. The postoperative complications were pleural effusion in all the cases and suture dehiscence in 3 cases (50%); of those patients only one was reoperated on through esophagectomy plus jejunostomy, whereas the remaining 2 were treated through conservative maneuvers with the consequent appearance of esophagopleural fistula. Two patients suffered multiorgan failure (33%). Hospital stay was 2-3 months in the 4 surviving patients (57%) and from 2 days to one month in the 3 patients that died.
DiscussionBoerhaave's syndrome is a surgical emergency with a high mortality rate. The medical literature reports a 20-30% mortality rate for this pathology,5 in contrast with the 43% of our case series.
Even though there were only 7 patients in our case series, that number is high, given the low frequency of the disease; 83 is the highest number of patients reported on in a published case series.6
Coinciding with the results of our study, spontaneous esophageal perforation is more frequent in men. It has traditionally been associated with important vomiting or the Valsalva maneuver, and its clinical presentation is intense pain and emphysema, even though it can present without these symptoms. In our study, the clinical presentation appeared subsequent to vomiting in 3 cases, it was related to the effort of coughing in 2 cases, and in one case it was associated with the effort of a prior bowel movement. The triggering cause could not be identified in only one case.
With respect to imaging studies, chest x-ray is indispensible.7,8 Left pleural effusion is practically a constant factor in this event, as our study reflected. Contrast-enhanced esophagography is the best diagnostic option, although today, due to its greater availability and precision, CT has gained importance and is often the definitive diagnostic study. In fact, in our case series, 2 of the older cases were diagnosed through esophagography, whereas CT was employed in the most recent cases.
There is no defined or established therapeutic decision for Boerhaave's syndrome. The choice between surgery or conservative treatment depends on many factors. Conservative treatment is indicated in hemodynamically stable patients with contained perforations that do not show any signs of sepsis or have the placement of a stent, thoracic tube, or feeding gastrostomy or jejunostomy.9,10 In our study, conservative management was only decided upon in one of the 7 cases and it was due to the fact that the patient's age and comorbidities were high surgical risk factors.
The surgical options are primary closure, reinforced primary closure (intercostal muscle, pleura, diaphragm, stomach, omentum, and lung) and esophageal exclusion or resection. Reinforced primary closure is the treatment of choice when progression is less than 24hours. More aggressive procedures, such as esophageal exclusion or resection, are indicated in cases of long perforations, extensive contamination, associated esophageal disease, primary closure failure, or persistent sepsis.10 In our study, primary suture was the option of choice and was performed in all of the cases, except for 2, one of which presented with sepsis of abdominal origin, and another that presented with extensive mediastinic contamination that had progressed >24hours. Reoperation in the form of partial esophagectomy was required in another patient due to failed primary suture.
As study conclusions, we emphasize the importance of early diagnosis, which is related to outcome. Complementary studies are essential given the inconsistency of the clinical presentation, and abdominopelvic CT scan was stressed in our study. With respect to management, surgical treatment currently appears to be the option that provides the best results.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Granel-Villach L, Fortea-Sanchis C, Martínez-Ramos D, Paiva-Coronel GA, Queralt-Martín R, Villarín-Rodríguez A, et al. Síndrome de Boerhaave: revisión de nuestra experiencia en los últimos 16 años. Revista de Gastroenterología de México. 2014;79:67–70.