Primary biliary cholangitis (PBC) is an autoimmune cholestatic disease associated with the presence of antimitochondrial antibodies (AMA). It exhibits an extensive number of extrahepatic autoimmune manifestations and a subgroup of patients present with other autoimmune skin diseases.1
We present herein the case of a 45-year-old woman diagnosed with PBC of 10-year progression, in advanced stage, with cirrhosis identified through ultrasound and a Child-Pugh grade C classification (11 points). She had been treated with ursodeoxycholic acid with adequate biochemical response according to the Paris criteria up to the age of 43 years. The patient presented with a progressive increase of AST, ALT, bilirubin, and alkaline phosphatase, with disease progression and change in the Child-Pugh grade (A: 6 points; C: 11 points). She had lichen planus in childhood and was diagnosed with breast cancer in 2002. She underwent radical mastectomy, chemotherapy, and radiotherapy, and had total disease remission since 2008.
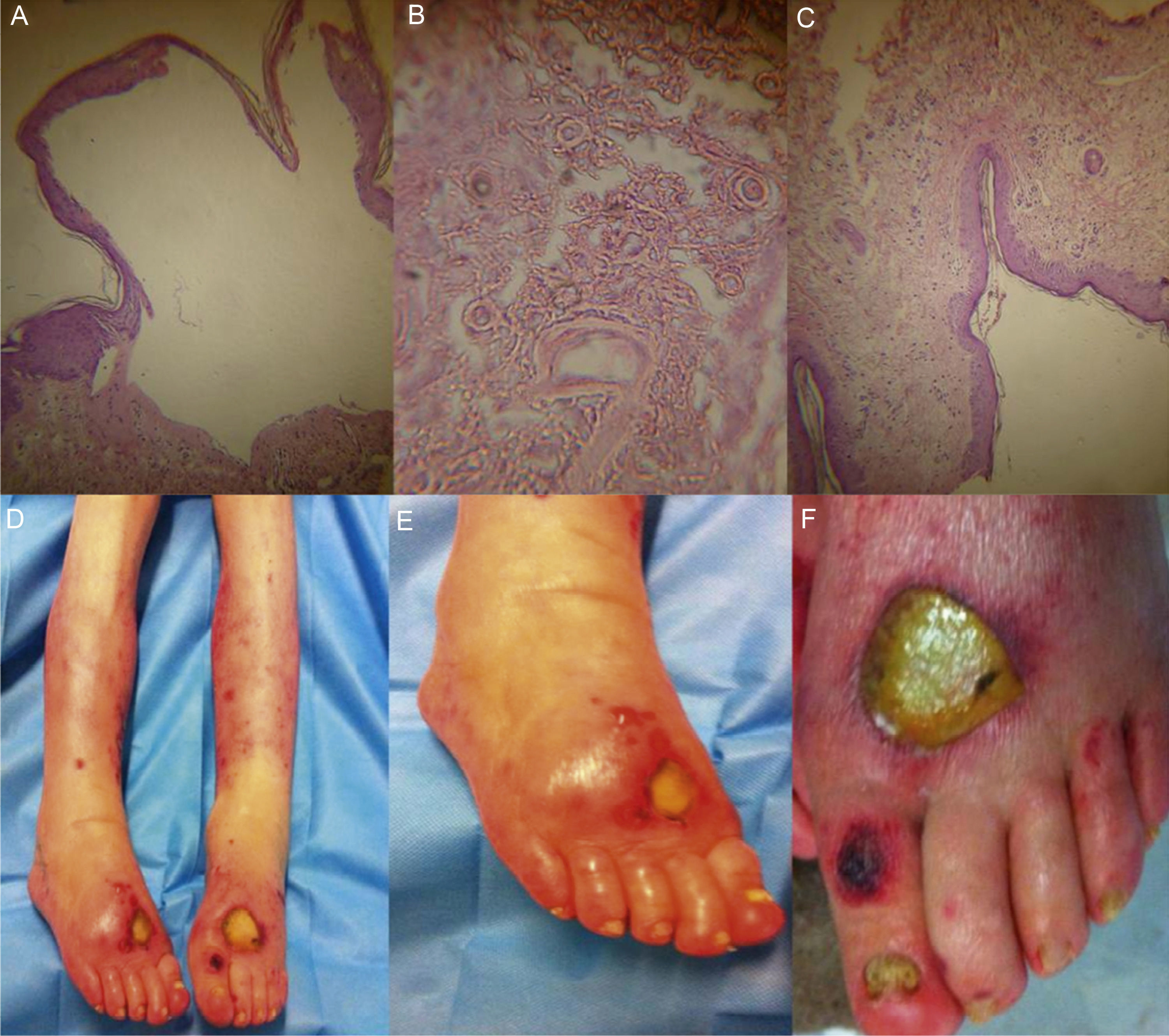
The patient sought medical attention at the emergency department for dermatosis of 21-day progression, characterized by fragile, blistering vesicular lesions with an erythematous halo. They initially appeared on the right upper limb and disappeared spontaneously. They later appeared in a generalized manner on the two lower extremities. Dermatologic examination revealed large denuded blisters with a fibrin-covered base (fig. 1) (some with necrotic edges), negative Nikolsky's sign, no mucosal involvement. In addition, there was paronychia and subungual hyperkeratosis, consistent with the diagnosis of tinea pedis. She presented with lymphedema of the right upper extremity and ipsilateral mastectomy. The skin biopsy report was subepidermal blister with a superficial, mixed, perivascular, inflammatory infiltrate consistent with bullous pemphigoid (BP). The skin lesions were not cultured and viral inclusions were not found in the biopsy. While hospitalized, the patient presented with a bladder catheter-related urinary tract infection, acute renal lesion, and spontaneous bacterial peritonitis, followed by septic shock attributed to the urinary infection, which ended in her death 5 days after hospital admission.
A-C) Histologic slides showing a subepidermal blister with a mixed superficial perivascular inflammatory infiltrate consistent with bullous pemphigoid; D-F) These images correspond to dermatologic lesions made up of large, denuded blisters with a fibrin-covered base, some of which have necrotic edges.
The dermatologic manifestations commonly associated with PBC are: nonspecific xanthomatous lesions and melanosis. Less frequent manifestations are lichen planus, scleroderma, and CREST syndrome (calcinosis cutis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia). PB only appears in case reports.2
PB is a frequent autoimmune skin disease representing 70% of the cases of primary autoimmune dermatosis. It is characterized by the presence of autoantibodies that are directed against the BP180 antigenic proteins, also known as bullous pemphigoid antigen 2 (BPAG2) or type XVII collagen, and BP230 or BPAG1 found in hemidesmosomes located along the basement membrane zone. Its clinical characterization is the initial appearance of very pruriginous urticaria-like or eczema-like lesions. Tense blisters can appear over them that are very large with a serous and hemorrhagic content. They are mainly located on the trunk of the body and the flexor surface of the extremities. Diagnosis is clinical, histologic, and immunologic.3
The association of BP with other autoimmune diseases has been previously referred to, but a common etiopathogenic pathway has not been demonstrated.4
Six cases of BP and PBC have been reported in the medical literature over the last 36 years and at present their association is considered coincidental. The prognosis for survival is poor in patients with BP and no other autoimmune disorders, reaching 30% at one year. Death is frequent within the first 12 weeks after treatment onset and its causes include adverse effects of therapy, superimposed infections, and complications related to the underlying disease.5
The habitual behavior of patients with coincident PBC and PB is unknown. Previous reports 6–8 refer to patients recently diagnosed with PBC and there are short-term reports on treatment response. Despite its rareness, it is important to begin opportune and multidisciplinary management. The recommended treatment in the majority of the guidelines includes prednisone (0.75mg/kg), dapsone (100mg/24h), or azathioprine (100-150mg/day). The aim is to prevent complications such as disease extension and severity and the development of infections that negatively affect prognosis, as in the present case.
The unfortunate case of our patient reflects the delay in seeking medical attention that resulted in a fatal outcome. In addition, early disease onset is associated with a worse prognosis and a higher failed treatment rate.
Even though this was not a case of multiple autoimmune diseases, we decided to report on the association of the two pathologies, given its unusual presentation, and thus increase clinical awareness in regard to these entities.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Guerra-Uribe NB, González-Huezo MS. Pénfigo bulloso y cirrosis biliar primaria, una asociación infrecuente. Reporte de caso. Revista de Gastroenterología de México. 2016;82:174–176.