Bariatric surgery is the most effective treatment for weight loss, with comorbidity control. With low complication rates, the reasons for reoperation are major complications or weight loss failure/weight regain. Nonsurgical problems can also present, such as anemia, dehydration, chronic pain, and malnutrition, among others. Our aim was to analyze the main causes of revisional surgery, reoperation, and hospital readmission, at a specialized bariatric center.
MethodsA retrospective study was conducted on patients that underwent bariatric surgery within the time frame of 2012 and 2019. The baseline analysis included demographic, anthropometric, and perioperative data, as well as a sub-analysis of the main readmission causes and complications.
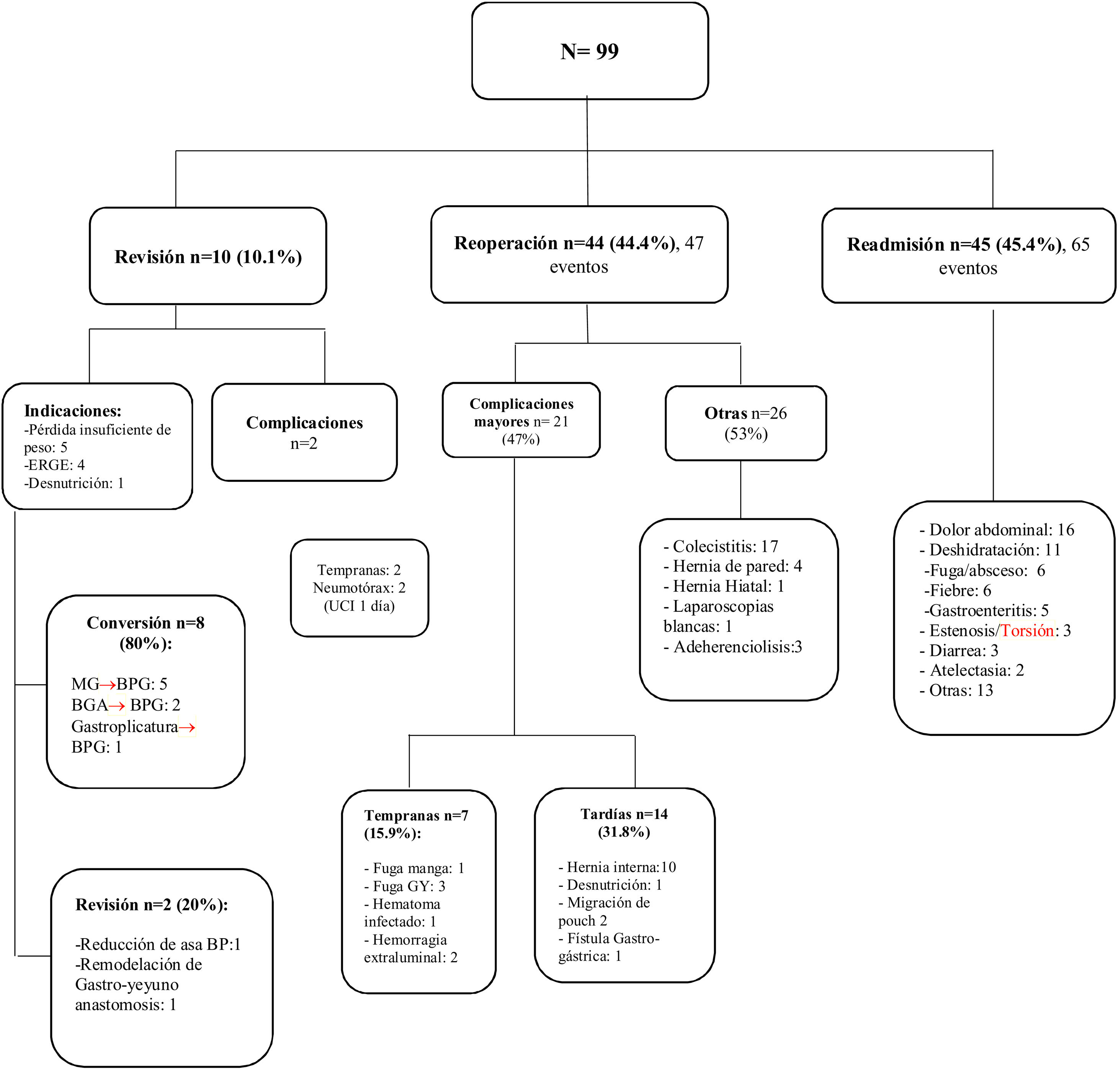
ResultsA total of 776 primary surgeries were performed (649 RYGBP, 127 SG, and 10 revisional surgeries), and 99 patients were identified for the study: 10 revisional surgeries, 44 reoperations, and 45 readmissions. The incidence of revisional surgery was 1.2%, reoperation was 5.6%, and readmission 5.8%. Fifty percent of the revisional surgeries were performed due to insufficient weight loss or weight regain; the most frequent causes of reoperation were cholecystitis (38.6%) and internal hernias (9.1%); and the most common causes of readmission were nonspecific abdominal pain (35.5%) and dehydration (24.4%).
ConclusionThe most frequent causes of postoperative readmission were nonsurgical events, followed by non-bariatric reoperations, and finally revisional surgeries. There was a low incidence of early reoperations. Knowledge of the abovementioned data is important for identifying higher-risk patients, to prevent major complications.
La cirugía bariátrica es el tratamiento más efectivo para la pérdida de peso, con control de comorbilidades. Con bajas tasas de complicaciones, las razones para una reintervención pueden ser complicaciones mayores o falla/reganancia de peso. También se presentan problemas no quirúrgicos como anemia, deshidratación, dolor crónico y desnutrición, entre otros. El objetivo fue analizar las principales causas de cirugía revisional, reoperación y readmisión en un centro bariátrico de referencia.
MétodosEstudio retrospectivo de pacientes sometidos a cirugía bariátrica entre 2012 y 2019. Se realizó un análisis basal incluyendo datos demográficos, antropométricos y perioperatorios y un subanálisis con las principales indicaciones de readmisión y complicaciones.
ResultadosSe realizaron 776 cirugías primarias (649 BPGYR, 127 MG y 10 cirugías de revisión), incluyendo 99 pacientes para el estudio: 10 de cirugía revisional, 44 reoperaciones y 45 readmisiones. La incidencia de cirugía revisional fue 1,2%, reoperación y readmisión 5,6% y 5,8% respectivamente. El 50% de las cirugías revisionales fue por pérdida insuficiente o reganancia de peso. Las causas más frecuentes de reoperación fueron: colecistitis (38.6%) y hernias internas (9.1%); las causas de readmisión más comunes fueron dolor abdominal inespecífico (35.5%) y deshidratación (24.4%).
ConclusiónLas causas más frecuentes de readmisión poscirugía fueron enfermedades no quirúrgicas, seguido de reoperaciones no bariátricas y, finalmente, cirugías de revisión. Las reoperaciones tempranas por complicaciones tienen una incidencia baja. Es importante conocer lo previo para identificar a los pacientes con mayor riesgo y así prevenir complicaciones mayores.
Obesity has become an important health problem and a priority worldwide.1 Bariatric surgery is an effective treatment for inducing substantial and lasting weight loss.2–4 Safety has increased, since the improvement of laparoscopic techniques and accelerated recovery protocols. The current approximate calculations are a 10% morbidity rate and a mortality rate from 0.1-0.3%.5–7 The incidence of reoperations after Roux-en-Y gastric bypass (RYGBP) and sleeve gastrectomy (SG) is calculated at between 4.9% and 9.8%, respectively,8 with an overall readmission rate of ≈ 5.2%.9 Said variations largely depend on the primary procedure, patient selection, type of approach, and learning curve, among other factors.10 With respect to etiology, the most common causes that lead to reoperation are major complications (early and late), or weight loss failure/weight regain.11,12 Regarding hospital readmission, causes can also be nonsurgical, such as anemia, dehydration, chronic pain, and malnutrition, to name a few.13,14 In addition, it is important to know that 15-35% of patients that undergo bariatric surgery will not lose more that 50% of their excess weight, resulting in an increase in the number of overall revisional surgeries worldwide.15,16 The American Society of Metabolic and Bariatric Surgery (ASMBS) reported that of the 252,000 bariatric surgeries performed in 2018 in the United States, 15.4% were revisional surgeries.8
It is vitally important to know the causes of readmission (surgical and medical) in patients that underwent bariatric surgery, given that obesity is a chronic condition that entails complex and life-long management. In the present study, we analyzed the causes of revisional surgery, reoperation, and hospital readmission at a specialized bariatric center.
MethodsA retrospective study (with prospective data collection) was conducted on all patients that underwent bariatric surgery at a single institution, within the time frame of 2012 and 2019. The primary aim was to identify the patients that underwent revisional surgery (revision, conversion, or reversal), reoperation (diagnostic/therapeutic laparoscopies, cholecystectomies, internal and abdominal wall hernias) and patients that required nonsurgical intrahospital management (readmission). The baseline analysis included demographic, anthropometric, and perioperative data, and a sub-analysis was carried out that reported the indications for revisional surgery, reoperation, and readmission, as well as the main complications. Patients that came for re-evaluation, but were not hospitalized, or those that stayed fewer than 24 h, were excluded.
Statistical analysisDescriptive statistics were expressed using means, averages, and standard deviation and the qualitative variables were expressed, using frequencies and percentages. The SPSS version 21 software was employed.
Ethical considerationsThe authors declare that informed consent was requested from the patients to receive treatment and participate in the research described.
The authors declare that the work follows the current regulations in bioethical research and was authorized by the research ethics committee and registered as CONBIOÉTICA-09-CEI-001-20160404, with the institutional registration number of 212-110-05-20.
The authors declare that this article contains no information that could identify the patients.
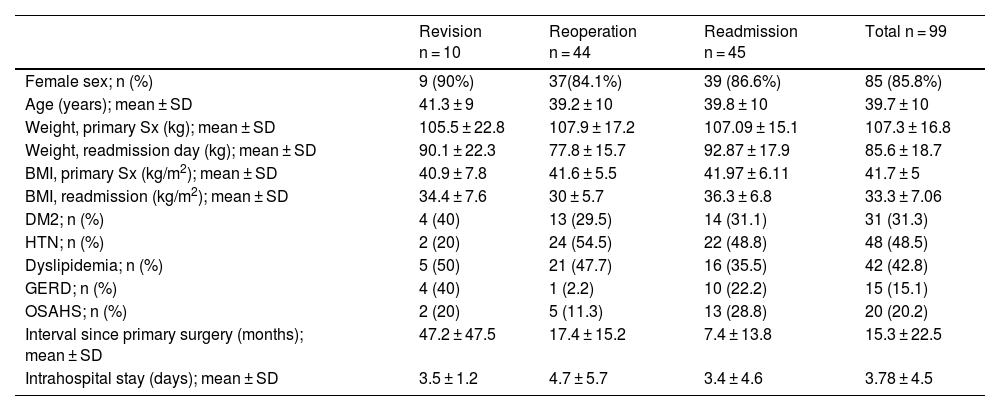
ResultsWithin the study period, 776 primary bariatric surgeries were performed, of which 649 (83.6%) were RYGBP surgeries, 127 (16.3%) were SGs, and 10 (1.5%) were revisional surgeries. Ninety-nine patients were identified for the study: 10 (10.1%) had revisional surgery, 44 (44.4%) were reoperated on, and 45 (45.4%) were nonsurgical readmissions. The total distribution of revisional surgeries was 1.2%, the distribution of reoperations was 5.6%, and that of surgery-related hospital readmissions was 5.8%. Mean patient age was 39.7 ± 10 years, 85.8% of the patients were women, and preoperative body mass index (BMI) was 41.7 ± 5.9 m/kg². The time interval from the primary procedure to the secondary event, without distinguishing between groups, was 15.3 ± 22.5 months, but there were important variations when those values were studied per group, with the revisional surgery group having the widest margin. Table 1 shows the complete analysis.
Demographic, anthropometric, comorbidity, and intrahospital characteristics.
| Revision n = 10 | Reoperation n = 44 | Readmission n = 45 | Total n = 99 | |
|---|---|---|---|---|
| Female sex; n (%) | 9 (90%) | 37(84.1%) | 39 (86.6%) | 85 (85.8%) |
| Age (years); mean ± SD | 41.3 ± 9 | 39.2 ± 10 | 39.8 ± 10 | 39.7 ± 10 |
| Weight, primary Sx (kg); mean ± SD | 105.5 ± 22.8 | 107.9 ± 17.2 | 107.09 ± 15.1 | 107.3 ± 16.8 |
| Weight, readmission day (kg); mean ± SD | 90.1 ± 22.3 | 77.8 ± 15.7 | 92.87 ± 17.9 | 85.6 ± 18.7 |
| BMI, primary Sx (kg/m2); mean ± SD | 40.9 ± 7.8 | 41.6 ± 5.5 | 41.97 ± 6.11 | 41.7 ± 5 |
| BMI, readmission (kg/m2); mean ± SD | 34.4 ± 7.6 | 30 ± 5.7 | 36.3 ± 6.8 | 33.3 ± 7.06 |
| DM2; n (%) | 4 (40) | 13 (29.5) | 14 (31.1) | 31 (31.3) |
| HTN; n (%) | 2 (20) | 24 (54.5) | 22 (48.8) | 48 (48.5) |
| Dyslipidemia; n (%) | 5 (50) | 21 (47.7) | 16 (35.5) | 42 (42.8) |
| GERD; n (%) | 4 (40) | 1 (2.2) | 10 (22.2) | 15 (15.1) |
| OSAHS; n (%) | 2 (20) | 5 (11.3) | 13 (28.8) | 20 (20.2) |
| Interval since primary surgery (months); mean ± SD | 47.2 ± 47.5 | 17.4 ± 15.2 | 7.4 ± 13.8 | 15.3 ± 22.5 |
| Intrahospital stay (days); mean ± SD | 3.5 ± 1.2 | 4.7 ± 5.7 | 3.4 ± 4.6 | 3.78 ± 4.5 |
BMI: body mass index; DM2: type 2 diabetes mellitus; GERD: gastroesophageal reflux disease; HTN: hypertension; OSAHS: obstructive sleep apnea/hypopnea syndrome; SD: standard deviation; Sx: surgery.
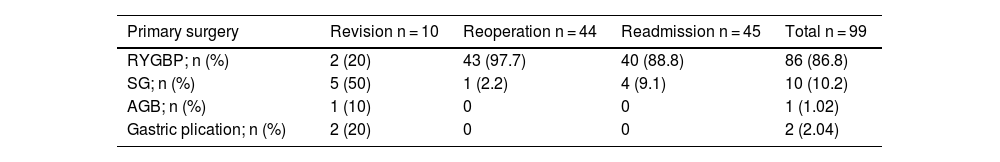
Table 2 lists the total distribution, with percentages, of the primary bariatric procedures performed on each group and on the total population. The majority (50%) of the revisional surgeries were due to insufficient weight loss/weight regain (conversion of SG to RYGBP), followed by gastroesophageal reflux disease in 40% (conversion of adjustable gastric banding or SG to RYGBP), and one patient with revisional surgery due to malnutrition (the biliopancreatic limb was shortened).
Distribution of primary bariatric procedures per group.
| Primary surgery | Revision n = 10 | Reoperation n = 44 | Readmission n = 45 | Total n = 99 |
|---|---|---|---|---|
| RYGBP; n (%) | 2 (20) | 43 (97.7) | 40 (88.8) | 86 (86.8) |
| SG; n (%) | 5 (50) | 1 (2.2) | 4 (9.1) | 10 (10.2) |
| AGB; n (%) | 1 (10) | 0 | 0 | 1 (1.02) |
| Gastric plication; n (%) | 2 (20) | 0 | 0 | 2 (2.04) |
AGB: adjustable gastric banding; RYGBP: Roux-en-Y gastric bypass; SG: Sleeve gastrectomy.
Of the total of operated patients, the percentage of complications requiring early reoperation (< 30 days) was 0.9%, and the most frequent cause was gastrojejunal anastomosis leak (Fig. 1). The rate of the late reoperations associated with the primary surgery was 1.8%, and the most common procedure was diagnostic laparoscopy for internal hernia repair (Fig. 1). The sub-analysis of the reoperation group included the procedures performed to treat complications related to the primary surgery. Regarding the early reoperations (15.9%), the main causes were gastrojejunal anastomosis leaks and postoperative bleeding. The rest of the reoperations were late, and the most frequent were cholecystectomies (38.6%) and the correction of internal hernias (22.7%).
Complete analysis of the 3 study groups: revisional surgery, reoperation, and nonsurgical readmission. The main causes of readmission and complications are described.
AGB: adjustable gastric banding; BP: bypass; GERD: gastroesophageal reflux disease; GBP: gastric bypass; ICU: intensive care unit; SG: sleeve gastrectomy.
There were 65 events in 45 patients of the readmission group. The main cause was nonspecific abdominal pain (24.6%), followed by dehydration (16.9%). Gastrojejunal anastomosis fistulas were also identified and were resolved through conservative management or interventional radiology, as were SG strictures, that were resolved through endoscopic dilations. Fig. 1 shows the complete analysis of the 3 groups.
DiscussionThe present study identified the multiple causes of early or late hospital readmission in patients that underwent bariatric surgery. Said causes can be grouped into surgical readmissions (due to direct/indirect complications of the primary surgery or revisional surgery) and nonsurgical readmissions. The rates in all the areas analyzed coincided with those reported at academic centers worldwide, as did the overall early and late complication rates.
Bariatric surgery has shown a success rate superior to that of medical treatment in the resolution and improvement of obesity and its associated comorbidities.17 With laparoscopic technique enhancement, adequate patient selection, and accelerated recovery protocols, bariatric surgery surpasses more widespread procedures (colectomies, prostatectomies, hysterectomies, and even cholecystectomies due to acute cholecystitis) in safety.18 Nevertheless, surveillance of those patients should be strict and long term, given that there is a considerable rate of both early and late complications. Previous studies have identified the main causes of bariatric revision and reoperation,10 but there is scant literature on the causes of hospital readmission after those types of procedures in Latin American populations.19 Whatever the reason for readmission, it accounts for greater costs for the institution (or patient), and so it is important to know the main causes, frequency, and therapeutic options, to develop strategies that enable improved and opportune care.
In a cohort of more than 50,000 patients, the main causes of early readmission (< 30 days) were abdominal pain, oral diet intolerance, and dehydration.20 In our population, those were also the main causes of nonsurgical readmission. Among the preoperative factors that have been associated with higher risk for readmission are the type of surgery (RYGBP > SG), the surgery center (accredited and volume level), the presentation of complications, the sociodemographic characteristics (race and sex), and the lack of adherence to the multidisciplinary follow-up.21
The development of innovative programs directed at high-risk patients could result in a significant and achievable reduction in healthcare costs.22 A current initiative of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) of the ASMBS is the Decreasing Readmissions through Opportunities Provided (DROP) project.23 It focuses on the components of patient education, discharge planning, and postoperative care coordination, to identify patients at high risk for complications.
With respect to revisional surgery, a recent systematic review9 reported that the majority of cases were secondary to insufficient weight loss or weight regain, which concurs with our findings. Importantly, causes vary according to the type of primary procedure. For example, the increase in frequency of gastroesophageal reflux after adjustable gastric banding and SG leads to conversions, regardless of BMI. Other types of indirect complications that have been frequently observed are gallstones and internal hernias.24,25 Both were the main causes of non-bariatric reoperation in our case series, as well as in the overall literature.19
Finally, a theme not widely covered has been the increase in the prevalence of addictions (reported to affect up to one-third of surgery candidates). The risk of self-inflicted injuries and suicide after bariatric surgery is also higher in the surgical population, compared with paired controls.26 However, the real impact on hospital readmissions is not known. The hospital readmission of many of those patients is most likely underestimated, given that they tend to take place at institutions that specialize in those types of disorders. For example, at our institution, we have only known of 2 patients with self-inflicted injuries, but they were not hospitalized.
With the current knowledge of the different strategies for reducing readmission rates, we implement rigorous preoperative planning and education (medical-psychologic-nutritional) at our center and exclude patients with untreated psychiatric disorders and mandatory weight loss. After the surgery, we maintain a close channel of communication between the patients and the multidisciplinary team, with follow-up appointments starting one week after the operation, then at 3, 6, 9, and 12 months, followed by every 6 months for life. Likewise, 24-hour emergency telephone lines are available, as well as emergency attention, if needed. Said strategies have enabled us to detect early complications, to act swiftly and specifically, according to the case, thus achieving a 0% mortality rate. Finally, the availability 24/7 of an ICU, blood bank, and radiologic imaging studies (especially computed tomography), plus the support of interventional radiology and endoscopy (diagnostic and therapeutic) are key for achieving the proposed goals.
In summary, with the data obtained herein, we can see that the causes of revision, reoperation, and readmission after bariatric surgery in our Mexican population are similar to those reported in the international literature. 20,27,28 One of the present study’s limitations is the question of reproducibility of the results in nonspecialized centers, given that our study was exclusively conducted at a bariatric center. Another limitation was the exclusion of patients that were readmitted for medical management but not hospitalized for more than 24 h (for iron infusions, nonspecific gastrointestinal problems, and the performance of diverse studies).
ConclusionsThere is a considerable number of hospital readmissions after bariatric surgery. The most frequent causes are nonsurgical events, followed by non-bariatric reoperations, and revisional surgeries, respectively. There is a low rate of complication-related early reoperations. Knowledge of the factors described herein is important for identifying patients at higher risk, thus preventing major complications.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Hernández LA, Guilbert L, Sepúlveda EM, Rodríguez F, Peñuñuri F, García VH, et al. Causas de cirugía revisional, reoperaciones y readmisión posterior a cirugía bariátrica. Rev Gastroenterol Méx. 2023;88:232–237.