Non-cardiac chest pain (NCCP) is mainly related to oesophageal disease, and in spite of being a common condition in Mexico, information regarding it is scarce.
AimTo assess the clinical characteristics and health-related quality of life of patients with NCCP of presumed oesophageal origin.
Material and methodsPatients with NCCP of presumed oesophageal origin with no previous treatment were included in the study. Associated symptoms were assessed and upper gastrointestinal endoscopy and 24-hour oesophageal pH monitoring were performed to diagnose gastroesophageal reflux disease, while oesophageal manometry was used to determine oesophageal motility disorders. The SF-36 Health-Related Quality of Life (HR-QoL) questionnaire was completed and its results compared to a control group without oesophageal symptoms.
ResultsThe study included 33 patients, of which 61% were women, and the mean age was 46.1 (±11.6) years. Causes of NCCP were gastroesophageal reflux disease in 48%, achalasia in 34%, and functional chest pain in 18%. The average progression time for chest pain was 24 (2-240) months, with≤3events/week in 52% of the patients. The most frequent accompanying symptoms were: regurgitation (81%), dysphagia (72%) and heartburn (66%). Patients with NCCP show deterioration in HR-QoL compared to the control group (P=.01), regardless of chest pain aetiology. The most affected areas were general perception of health, emotional issues, and mental health sub-scale (P>0.05).
ConclusionsIn our population, patients with NCCP show deterioration in HR-QoL regardless of the aetiology, frequency, and accompanying symptoms.
El dolor torácico no cardiaco (DTNC) se relaciona principalmente con enfermedades del esófago, y aunque se considera una condición común, en México la información aún es escasa.
ObjetivoEvaluar las características clínicas y la calidad de vida relacionada con salud en pacientes con DTNC de presunto origen esofágico.
Material y métodosSe incluyeron en el estudio pacientes con DTNC de presunto origen esofágico, sin tratamiento previo. Se evaluaron los síntomas asociados, se realizó endoscopia alta y monitorización de pH esofágico de 24h para establecer el diagnóstico de enfermedad por reflujo gastroesofágico, y para descartar trastornos en la motilidad esofágica se llevó a cabo manometría esofágica. Se aplicó el cuestionario de calidad de vida SF-36, y los resultados se compararon con un grupo control de sanos.
ResultadosSe incluyeron 33 pacientes, el 61% mujeres, y la edad promedio fue 46.1 (±11.6) años. Las causas de DTNC fueron: enfermedad por reflujo gastroesofágico 48%, acalasia 34% y dolor torácico funcional 18%. El tiempo promedio de progresión del dolor torácico fue 24 (2-240) meses, con≤3 eventos/semana en el 52%. Los síntomas acompañantes más frecuentes fueron: regurgitaciones (81%), disfagia (72%) y pirosis (66%). Los pacientes con DTNC muestran deterioro en su calidad de vida comparado con el grupo control, independientemente de la etiología del dolor torácico. Los dominios más afectados son la percepción general de salud, problemas emocionales y la subescala de salud mental, sin diferencia estadística significativa (P > 0.05).
ConclusionesEn nuestra población, los pacientes con DTNC muestran deterioro en su calidad de vida independientemente de la etiología, frecuencia y síntomas que acompañan al dolor torácico.
Non-cardiac chest pain (NCCP) is defined as episodes of non-burning, recurrent retrosternal pain that is unrelated to cardiac disease, and frequently originates in the gastrointestinal tract. It is a common disorder affecting approximately one third of the general population at some point in their lives, is equally prevalent in both sexes, and can appear from childhood to adulthood.1,2
NCCP has several known causes of presumed esophageal origin; of these, gastroesophageal reflux disease (GERD) is the most frequent, producing more than 60% of the cases. Others are motor disorders of the esophagus and visceral hypersensitivity, which include psychiatric disorders. According to the Rome III criteria, chest pain (CP) is considered functional (functional CP [FCP]) once GERD and motor disorders have been ruled out as its causes.3–9
Although the natural history of the disease is still not well known, it has been reported that patients with NCCP have a good prognosis, with 10-year mortality rates below 1%. However, morbidity is high as a result of daily activity limitations and absenteeism in the workplace, which have a negative impact on quality of life.8,10–13 It has been calculated that in the United States, a large number of resources in the health sector are used for the study and treatment of NCCP.14
Studies that have analyzed NCCP and quality of life in the past report that, in general, quality of life is poor and the scales with the greatest impact are related to physical function (physical performance), the perception of health, and mental health.14 Nevertheless, the relation between etiology and quality of life deterioration has yet to be studied.
The aim of the present study was to evaluate clinical characteristics and quality of life regarding the health of patients with NCCP of presumed esophageal origin.
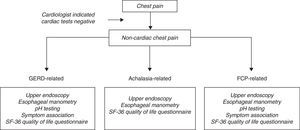
MethodsAll patients diagnosed with NCCP of presumed esophageal origin arriving at the Gastroenterology and Endoscopy Services of the “Hospital de Especialidades, Centro Médico Nacional Siglo XXI” between June 2007 and June 2009 were invited to participate in the study. Four groups were included: 1) patients with NCCP associated with GERD: a) as diagnosed by abnormal 24-h esophageal pH-monitoring (total time with pH < 4 in 24h ¿ 4.2% and/or Johnson-DeMeester index >14.72),15 plus endoscopy data indicating GERD (erosion of the distal esophagus or chronic complications such as Barrett's metaplasia), and b) patients with an abnormal 24-h esophageal pH-monitoring in the absence of endoscopically visible esophageal mucosal injuries (nonerosive reflux disease [NERD] patients); 2) patients with FCP as defined by the Rome III criteria when endoscopy of the upper gastrointestinal tract, esophageal manometry, and ambulatory 24-h pH monitoring were normal;9 3) patients diagnosed with classic achalasia without previous treatment (classic achalasia is defined by incomplete lower esophageal sphincter [LES] relaxation and aperistalsis of the esophagus);16,17 and 4) a control group including 51 healthy subjects with a mean age of 35 (± 13.5) years; 31 women and 20 men. All controls had a complete medical history and none of the volunteers had a history of esophageal symptoms, surgery of the digestive tract, or the ingestion of any medication that could affect gastrointestinal function. They were recruited in the same time period and completed the SF-36 questionnaire on quality of life.
All patients underwent a complete medical history and answered the SF-36 quality of life questionnaire.
NCCP was defined by the presence of at least two episodes of non-burning retrosternal CP per week, within the last 3 months,9 once acute coronary disease had been ruled out as the cause of CP by electrocardiogram, the Bruce protocol stress test, thallium stress test, and coronarography referred by a cardiologist.
Exclusion criteria were as follows: treatment with proton pump inhibitors (PPIs) or H2 receptor antagonists, calcium channel blockers, beta-blockers and/or nitrates seven days before the study; a history of previous esophageal surgery; a history of serious neurologic or psychiatric disease under current treatment; vigorous achalasia, and refusal to participate in the study. All patients that agreed to participate in the study gave their written consent. The study was approved by the Ethics Committee of the Hospital de Especialidades del Centro Médico Nacional Siglo XXI, IMSS, in Mexico City and was carried out according to the health research norms of the Department of Health.
Study ProtocolAll patients were assessed by a gastroenterologist who questioned them and determined the frequency and time of progression for each of the symptoms (CP, dysphagia, heartburn, regurgitation, odynophagia, nocturnal cough, dysphonia, and weight loss). The following scale was employed:
Frequency: 0) Absent; 1) Present ≤ once a month; 2) Present ≤ once a week; 3) Present ≤ 3 times a week; 4) Present ≥ 3 times a week or every day; and 5) Present at every meal.
Weight loss was calculated in kilograms and was determined from the period of symptom onset to the time of diagnosis. Time of disease progression was reported in months for each of the symptoms present.
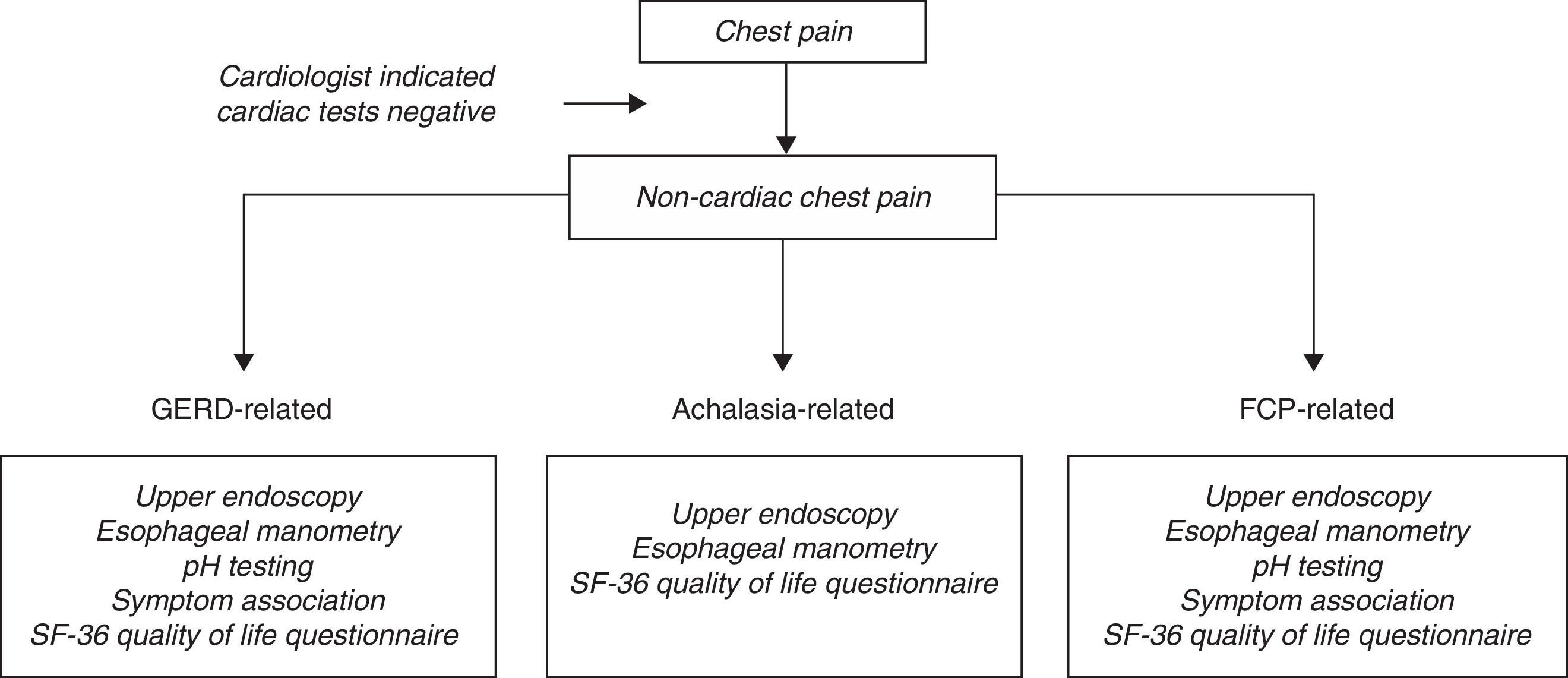
Patients were protocolized as shown in figure 1:
Upper Gastrointestinal EndoscopyUpper gastrointestinal endoscopy was performed and interpreted by the same group of gastroenterology endoscopists. Fujinon® EG 201FP video-endoscopic equipment was used. Each patient had been fasting for six hours and was placed in the left lateral decubitus position, while the endoscopic examination was performed with the standard technique.18 The distal esophagus was carefully examined to detect the presence of lesions in the esophageal mucosa and its continuity was graded according to the Los Angeles Classification.19
Stationary esophageal manometryEach patient arrived at the Motility Laboratory having fasted for 6h; the study was performed with the stationary pull-through technique.20 In all cases, a water perfusion system was placed through the nose. It consisted of a catheter made of 4 radially oriented channels with diameters of 3.5mm that were situated at a distance of 50mm from each other (Alpine BioMed Manometric Catheter, Alpine Biomed, Corp, 17800 Newhope St, Suite B, Fountaine Valley, CA, 92708 USA and Zinetics Manometric Catheter, Medtronic A/S, Tonsbakken 16-18, DK-2740 Skovunde, Denmark). The catheter was continuously perfused at 0.5mL/min by a hydro-pneumatic infusion pump connected to the Solar UPS-2020 polygraph measurement system (PO Box 580, 7500 AN Enschede, The Netherlands). Changes in intraesophageal pressure were converted into an electric signal by a transducer and then recorded on the computer (stationary motility systems, software version 8, GI Manometry, MMS b.v.). The manometric tracings were interpreted by a specialist and motor disorders were evaluated according to the 2001 Classification Criteria of Esophageal Motility Disorders.16,21
24-h ambulatory pH monitoringPortable equipment (Digitrapper pH 400 Medtronic 2003, Denmark) and an antimony sensor catheter (VersaFlex® Disposable pH catheter, Internal Reference, single sensor, Alpine Biomed, Corp, 17800 Newhope St, Suite B, Fontaine Valley, CA, USA) were used. The catheter was placed in the stomach via the nose and the sensor was positioned 5cm above the LES as determined by manometry. The electrode catheter was connected to the portable unit and recording was started. The patients were told to use the Digitrapper event button to record the start and duration of each painful episode, mealtimes, and whether they were in supine position. For the data analysis, the Digitrapper was transferred to a personal computer and processed using Polygram NetTM Version: 4.01.525.45 software (Copyright© 2001–2003 Medtronic A/S). Gastroesophageal reflux was determined to be present when the total percentage time with pH < 4 in 24h was > 4.2% and/or the Johnson-DeMeester composite score was > 14.72.15 The temporal relation between CP and acid reflux episodes was considered positive with a symptom index > 50%.22 A positive correlation with symptom association probability was considered when the symptom index was > 95%.23,24 The relation interval with the CP event was considered for 2min before and after the symptom.
SF-36 Quality of Life QuestionnaireThe SF-36 Quality of Life Questionnaire consists of 36 questions that cover 8 health items: 1) physical functioning, 2) role limitations due to physical health problems, 3) bodily pain, 4) general health, 5) vitality, 6) social functioning, 7) role limitations due to emotional problems, and 8) mental health. These are grouped into the 2 general subscales of mental health summary and physical health summary. Low scores reflect a poor perception of health, loss of functioning, and the presence of pain, whereas high scores reflect a good perception of health, no functional deficit, and no pain.25
Statistical analysisResults were expressed as frequencies, medians (intervals), and means (± SD). Dichotomous variables were compared by chi-square or Fisher's exact tests. Quality of life scores were compared by non-parametric tests (Kruskal-Wallis and Mann Whitney U tests). Spearman's correlation coefficient was used to assess the correlation between quantitative variables. A value of p < 0.05 was considered significant. The analysis was performed by means of the SPSS for Windows statistical package (version 17.0; SPSS, Chicago, IL, USA).
ResultsForty-eight patients with NCCP of presumed esophageal origin were evaluated and 33 of them, 20 women and 13 men with a mean age of 46.1 (±11.6) years, were included in the study. Fifteen patients were excluded; 7 that were under PPI treatment and 8 that did not agree to take part in the study.
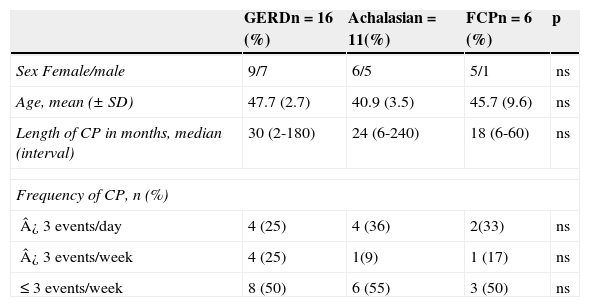
The causes of NCCP were GERD in 48% (n=16) of the subjects, classic achalasia in 34% (n=11), and FCP in 18% (n=6). Frequency of CP events and their duration are shown in Table 1.
Basal traits of the study group.
| GERDn = 16 (%) | Achalasian = 11(%) | FCPn = 6 (%) | p | |
|---|---|---|---|---|
| Sex Female/male | 9/7 | 6/5 | 5/1 | ns |
| Age, mean (± SD) | 47.7 (2.7) | 40.9 (3.5) | 45.7 (9.6) | ns |
| Length of CP in months, median (interval) | 30 (2-180) | 24 (6-240) | 18 (6-60) | ns |
| Frequency of CP, n (%) | ||||
| ¿ 3 events/day | 4 (25) | 4 (36) | 2(33) | ns |
| ¿ 3 events/week | 4 (25) | 1(9) | 1 (17) | ns |
| ≤ 3 events/week | 8 (50) | 6 (55) | 3 (50) | ns |
CP: chest pain; GERD: Gastroesophageal reflux disease; FCP: Functional chest pain; ns: not significant; SD: Standard deviation.
*T test to evaluate differences among means; ** Z or F test to evaluate difference among frequencies; ***Test of medians to evaluate their differences.
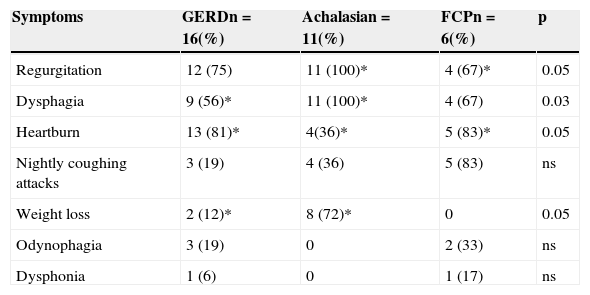
The associated symptoms most commonly referred in each of the 3 groups were regurgitation, dysphagia, and heartburn. Heartburn was the prevailing symptom in patients with GERD and FCP, whereas dysphagia and regurgitation were the main symptoms in patients with achalasia. Weight loss was found in 30.3% of the patients, clearly predominating in the group with achalasia, where it was reported in 72% of the cases with a mean of 9kg (± 2.4) (Table 2).
Clinical data of the study population.
| Symptoms | GERDn = 16(%) | Achalasian = 11(%) | FCPn = 6(%) | p |
|---|---|---|---|---|
| Regurgitation | 12 (75) | 11 (100)* | 4 (67)* | 0.05 |
| Dysphagia | 9 (56)* | 11 (100)* | 4 (67) | 0.03 |
| Heartburn | 13 (81)* | 4(36)* | 5 (83)* | 0.05 |
| Nightly coughing attacks | 3 (19) | 4 (36) | 5 (83) | ns |
| Weight loss | 2 (12)* | 8 (72)* | 0 | 0.05 |
| Odynophagia | 3 (19) | 0 | 2 (33) | ns |
| Dysphonia | 1 (6) | 0 | 1 (17) | ns |
FCP: Functional chest pain; GERD: Gastroesophageal reflux disease; ns: not significant.
Z or F test to evaluate difference among frequencies; *: group with statistically significant results.
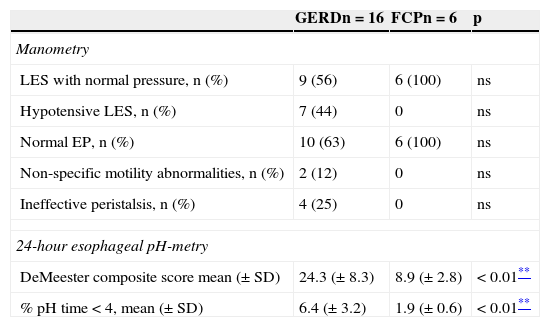
In the group of subjects with GERD, endoscopy revealed various degrees of esophagitis in 4 of the 16 patients (A = 2; B = 1; and D = 1), one patient had intestinal metaplasia confirmed by histopathology, and 11 patients were diagnosed with NERD. Twenty-five percent of the patients had failed peristalsis and 12% mild distal esophageal hypomotility, whereas peristalsis was normal in 63% of the cases. During 24-h pH monitoring, 19% of the patients reported CP. Manometric and pH-metry findings are shown in Table 3.
Findings of esophageal manometry and 24-hour esophageal pH-metry in patients with functional NCCP secondary to GERD.
| GERDn = 16 | FCPn = 6 | p | |
|---|---|---|---|
| Manometry | |||
| LES with normal pressure, n (%) | 9 (56) | 6 (100) | ns |
| Hypotensive LES, n (%) | 7 (44) | 0 | ns |
| Normal EP, n (%) | 10 (63) | 6 (100) | ns |
| Non-specific motility abnormalities, n (%) | 2 (12) | 0 | ns |
| Ineffective peristalsis, n (%) | 4 (25) | 0 | ns |
| 24-hour esophageal pH-metry | |||
| DeMeester composite score mean (± SD) | 24.3 (± 8.3) | 8.9 (± 2.8) | < 0.01** |
| % pH time < 4, mean (± SD) | 6.4 (± 3.2) | 1.9 (± 0.6) | < 0.01** |
EP: Esophageal peristalsis; FCP: Functional chest pain; GERD: Gastroesophageal reflux disease; LES: Lower esophageal sphincter; NCCP: non-cardiac chest pain; ns: not significant; SD: standard deviation.
* Z or F test to evaluate difference among rates.
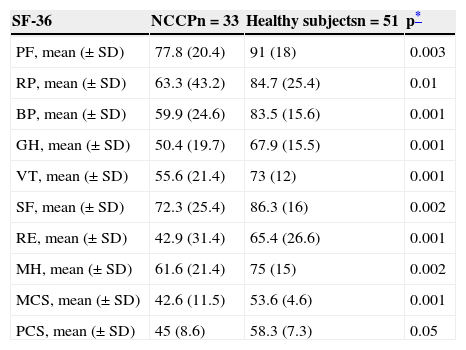
Patients with NCCP of presumed esophageal origin showed deterioration in quality of life, affecting all items in the SF-36 questionnaire, compared with the control group of subjects with no esophageal symptoms (p = 0.01). The most affected items were perception of general health (GH) and limitations due to emotional problems. The subscale with the greatest change was mental health summary, as shown in Table 4.
Results of the SF-36 Health Survey in patients with NCCP (n = 33) and the control group (n = 51).
| SF-36 | NCCPn = 33 | Healthy subjectsn = 51 | p* |
|---|---|---|---|
| PF, mean (± SD) | 77.8 (20.4) | 91 (18) | 0.003 |
| RP, mean (± SD) | 63.3 (43.2) | 84.7 (25.4) | 0.01 |
| BP, mean (± SD) | 59.9 (24.6) | 83.5 (15.6) | 0.001 |
| GH, mean (± SD) | 50.4 (19.7) | 67.9 (15.5) | 0.001 |
| VT, mean (± SD) | 55.6 (21.4) | 73 (12) | 0.001 |
| SF, mean (± SD) | 72.3 (25.4) | 86.3 (16) | 0.002 |
| RE, mean (± SD) | 42.9 (31.4) | 65.4 (26.6) | 0.001 |
| MH, mean (± SD) | 61.6 (21.4) | 75 (15) | 0.002 |
| MCS, mean (± SD) | 42.6 (11.5) | 53.6 (4.6) | 0.001 |
| PCS, mean (± SD) | 45 (8.6) | 58.3 (7.3) | 0.05 |
BP: Bodily pain; GH: General health; MCS: Mental component summary; MH: Mental health; NCCP: Non-cardiac chest pain; PCS: Physical component summary; PF: Physical functioning; RE: Role limitations due to emotional problems; RP: Role limitations due to physical health problems; SF: Social functioning; VT: Vitality.
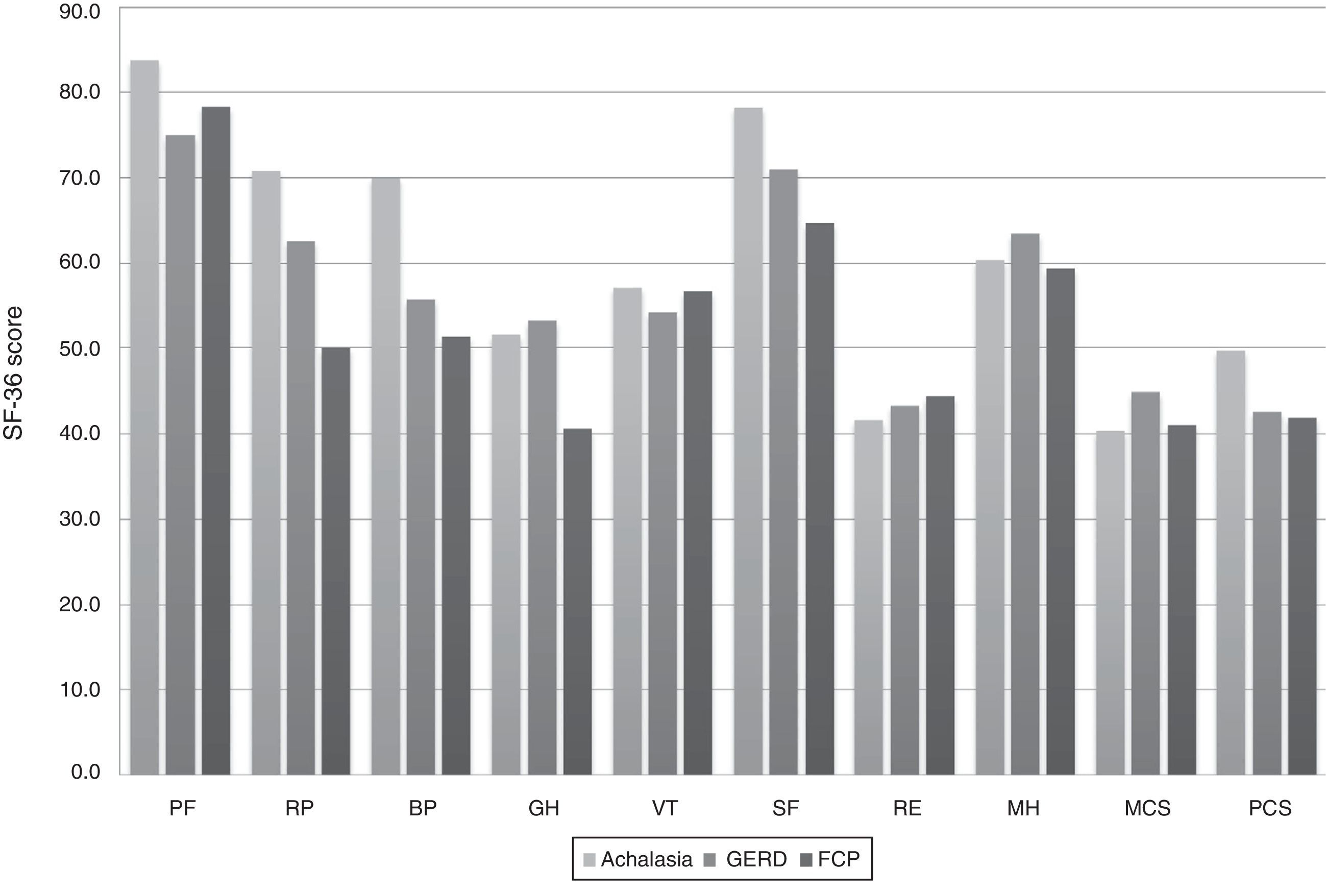
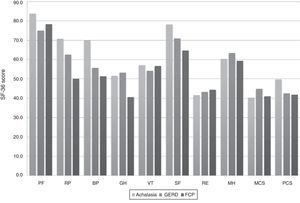
Regarding assessment of quality of life in relation to NCCP etiology, we observed differences in role physical, bodily pain, and social functioning, although they were not statistically significant (fig. 2). When evaluating subscales, we found that patients with GERD and FCP were mostly affected in the physical health summary subscale than in the group with achalasia, although, again, there was no statistical significance (p = 0.08).
Results of the SF-36 Health Survey in patients with NCCP.
The mean score for each of the 8 items and 2 subscales of the SF-36 questionnaire in patients with NCCP secondary to achalasia, GERD, and FCP are shown. High values reflect a perception of good health. The difference in means between groups was assessed by the Kruskal-Wallis test. BP: Bodily pain; FCP: Functional chest pain; GERD: Gastroesophageal reflux disease; GH: General health; MCS: Mental component summary; MH: Mental health; NCCP: Non-cardiac chest pain; PCS: Physical component summary; PF: Physical functioning; RE: Role limitations due to emotional problems; RP: Role limitations due to physical health problems; SF: Social functioning; VT: Vitality.
We found no correlation between quality of life and the frequency and duration of CP events.
DiscussionThe findings in our study showed that treatment-naïve patients with NCCP of presumed esophageal origin presented with deterioration in quality of life, regardless of CP etiology (GERD, achalasia, and FCP), and there were clinical differences that may suggest the cause of CP.
NCCP is a complex disorder and consequently it has been defined in a number of ways. A recent revision provides 2 commonly used definitions;26 the first is “CP that is not angina and is not due to ischemic coronary disease”, while the second states “recurring substernal CP or discomfort that must be diagnosed only after exclusion of non-esophageal causes such as heart, musculoskeletal, and pleuritic diseases and other disorders”. These definitions are clearly different, and there is still no definition that seems to adequately classify NCCP. Fass and Achem recently defined NCCP as recurring CP episodes that cannot be distinguished from ischemic heart pain after having reasonably ruled out a cardiac cause.27 In our study we defined NCCP as recurrent, non-burning episodes of retrosternal chest pain that is unrelated to heart disease.
Worldwide epidemiology of NCCP is relatively limited. It was recently reported that CP is the second most common event that is assessed at emergency services; however, only 25% of the subjects experiencing CP seek hospital care. Annual average prevalence, as evaluated in 6 different populations, was 25%. NCCP is found in similar proportions in both sexes, although women tend to seek medical care more often.27 Among the Mexican population, the prevalence and distribution by sex are unknown. In our study we found a predominance of women of up to 61%, and when analyzed by subgroup, we found they clearly predominated (83%) in the FCP group. It has been previously described that females with functional digestive disorders seek medical care more frequently,28 which may explain the high prevalence of women with FCP.
Identifying the cause of NCCP is still a problem in clinical practice, and because little is known regarding its pathophysiology, its mechanisms are numerous and overlapping. The main causes of NCCP are esophageal and psychiatric disorders, as well as musculoskeletal alterations.29 The most frequent cause of NCCP of presumed esophageal origin is GERD, present in approximately 60% of the cases.30 In contrast, only a minority of patients with CP show a motor esophageal disorder.31 Therefore, the empirical use of therapeutic testing with acid secretion inhibitors has been suggested as an initial diagnostic and therapeutic maneuver in patients with NCCP.27 In our population, 48% of the subjects had GERD as determined by endoscopy and/or 24-h esophageal pH-metry. The typical symptoms of reflux, heartburn, and regurgitation were found in more than 75% of the patients, with a clear predominance of heartburn in 81%. The incidence of abnormalities in the esophageal mucosa consistent with GERD was 25% and there was only one case of intestinal metaplasia. In the various populations studied, esophagitis associated with NCCP was reported in 10-70% of the cases.32 During ambulatory 24-h pH monitoring, only 19% of the patients reported CP, lower than the 21-44% previously described.33
The relation between NCCP and esophageal dysmotility is still a highly controversial topic. Several studies have shown that approximately 30% of patients with NCCP show alterations in esophageal manometry. However, information regarding alterations in esophageal motility in patients with NCCP that is not associated with GERD is still scarce. Dekel et al. identified hypotension of the LES, found in 61%, as the most frequent motor disorder in this population, followed by hypertension of the LES, non-specific motor disorders, and nutcracker esophagus.34 In contrast, Katz et al. reported that the most frequent motor disorder was nutcracker esophagus, followed by non-specific motor disorders, diffuse esophageal spasm, hypotension of the LES, and achalasia.35 In our analysis, the only esophageal motor disorder evaluated was classic achalasia, due to the low frequency of the other primary motor disorders of the esophagus in the study population. In patients with classic achalasia, we noticed that the symptoms most frequently observed were regurgitation and dysphagia in 100% of the subjects, along with significant weight loss in up to 72%; both of these findings were significantly different between the study populations.
In the most recent revision of the Rome Criteria for Functional Gastrointestinal Disorders, the definition of FCP of presumed esophageal origin was modified.9 In our study, patients with NCCP unrelated to GERD or primary esophageal motor disorders were classified as FCP in agreement with the Rome III criteria,17,36 which presented several symptoms associated with CP.
Although the most common cause of NCCP is reported to be esophageal, ruling out psychiatric disorders during the initial evaluation is recommended. More than one study reports that patients with NCCP secondary to GERD and FCP have disorders associated with anxiety and depression, which generally overlap. In a previous study we found that 51% of patients with NCCP had a psychopathological disorder. Among these, depression was the most prevalent with 33%; more than 50% of these cases required management and follow up by a psychiatrist. Anxiety disorders, including panic attacks and general anxiety, were present in 6.5% of the cases.37
It is accepted that NCCP has an impact on the quality of life of the subjects suffering from it; however, studies to assess quality of life in this group of patients are still limited. The scant information currently available indicates that the effect is universal and does not differ between those that arrive at emergency services and those that live with NCCP in the community. It has been reported that the severity of CP is important and that quality of life deteriorates as its severity increases.3
Wong et al. compared quality of life between healthy subjects and those with NCCP and found that patients with NCCP were affected in all items of the SF-36, compared with healthy subjects, especially in regard to physical functioning, role limitations due to physical health problems, and perception of GH.38 In our study we found a negative impact on quality of life in all areas of the SF-36 when compared with healthy subjects (those without esophageal symptoms) and the most affected areas were perception of GH and limitations due to emotional problems. Nevertheless we found no correlation between quality of life and the intensity of pain, as has been previously described.3
Quality of life has also been assessed in patients with NCCP and CP of cardiac origin and differences have been reported. However, we have not found reports in the literature where quality of life is compared according to NCCP etiology. We evaluated and compared quality of life in relation to etiology in patients with NCCP of presumed esophageal origin and found that those with GERD, achalasia, and CP had significant deterioration in quality of life, and that the various items of the SF-36 were similarly affected. This suggests that there may be no difference in the perception of the disease at either a physical and emotional level; however, our results must be confirmed by studies on a larger group of subjects.
The limitations of the study include the following: 1) the number of subjects evaluated per group was small, thus limiting our conclusions, 2) a general quality of life survey was used and it was not possible to administer a specific questionnaire per NCCP etiology; 3) we only included patients with classic achalasia, excluding other primary motor disorders of the esophagus, such as vigorous achalasia, in which CP has clinical and pathophysiologic characteristics that differ from the other primary motor disorders of the esophagus; and 4) no proton pump inhibitor therapeutic trial was performed.
The findings of the study suggest that patients with NCCP in our population have a poor quality of life regardless of the etiology, frequency, and symptoms that are associated with CP; the most affected items were perception of general health and limitations due to emotional problems. Prompt diagnosis and multidisciplinary treatment could improve patient quality of life.
Ethical responsibilitiesProtection of persons and animalsThe authors declare the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ortiz-Garrido O, Ortiz-Olvera NX, González-Martínez M, Morán-Villota S, Vargas-López G, Dehesa-Violante M, et al. Evaluación clínica y de la calidad de vida relacionada con la salud en pacientes con dolor torácico no cardiaco. Revista de Gastroenterología de México. 2015;80:121–129.
See related content at DOI: http://dx.doi.org/10.1016/j.rgmx.2015.06.001, Malamood M, Schey R. Diminished quality of life in non-cardiac chest pain: A cause as much as an effect. Revista de Gastroenterología de México. 2015;80(2):119–20.