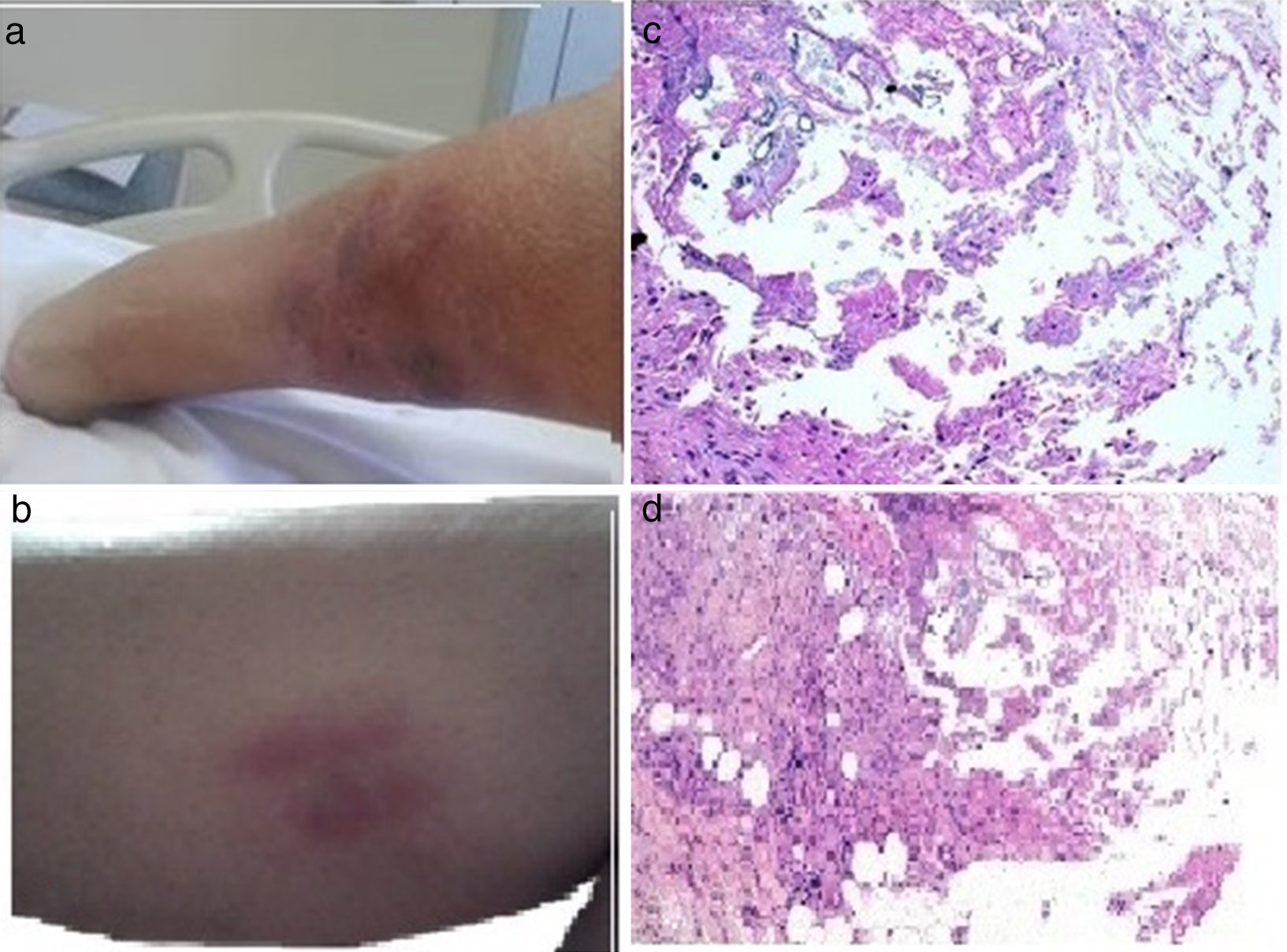
A 42-year-old woman with a past history of kidney transplantation due to probable post-streptococcal glomerulopathy sought medical attention for painful erythematous nodules on her legs of 2-month progression (Figure 1 a and b). She had no fever or other symptoms and was referred to the dermatology department. Biopsy was carried out and the report stated fat necrosis of pancreatic origin (Figure 1c and d). The appearance of the nodules coincided with the loss of kidney graft function and re-initiation of hemodialysis. The patient was transferred to the gastrointestinal service due to high amylase and lipase levels (more than triple the normal rate). Upon her admission she had no abdominal pain, jaundice, choluria, fever, or chills.
a and b) Image of the lower limb showing painful, purplish, erythematous, subcutaneous, nodular lesions consistent with panniculitis, some with oleous secretions. c and d) Pathologic anatomy image (hematoxylin-eosin) of cutaneous lesions showing fibrosis covering some fatty zones with inflammatory cells and other histiocytes, as well as areas of non-cellular amorphous basophilic material. Fat necrosis with difficult-to-distinguish adipocytes and microcalcifications can be seen in other areas.
Physical examination revealed only dermatosis located on the lower limbs, characterized by pinkish macules and purplish subcutaneous nodules, some of which were oozing oleous matter. The patient's past history included a kidney transplantation in 1998, secondary hyperparathyroidism, chronic hepatopathy due to HCV with F2 liver fibrosis in the transitional elastography study, and cutaneous B cell lymphoma with no evidence of extracutaneous activity. The patient had undergone parathyroidectomy and cholecystectomy. Her ongoing treatment was: prednisone, mycophenolate, telmisartan, sotalol, darbepoetin, folic acid, atorvastatin, calcium, hidroferol, calcitriol, magnesium, AAS, and pantoprazole.
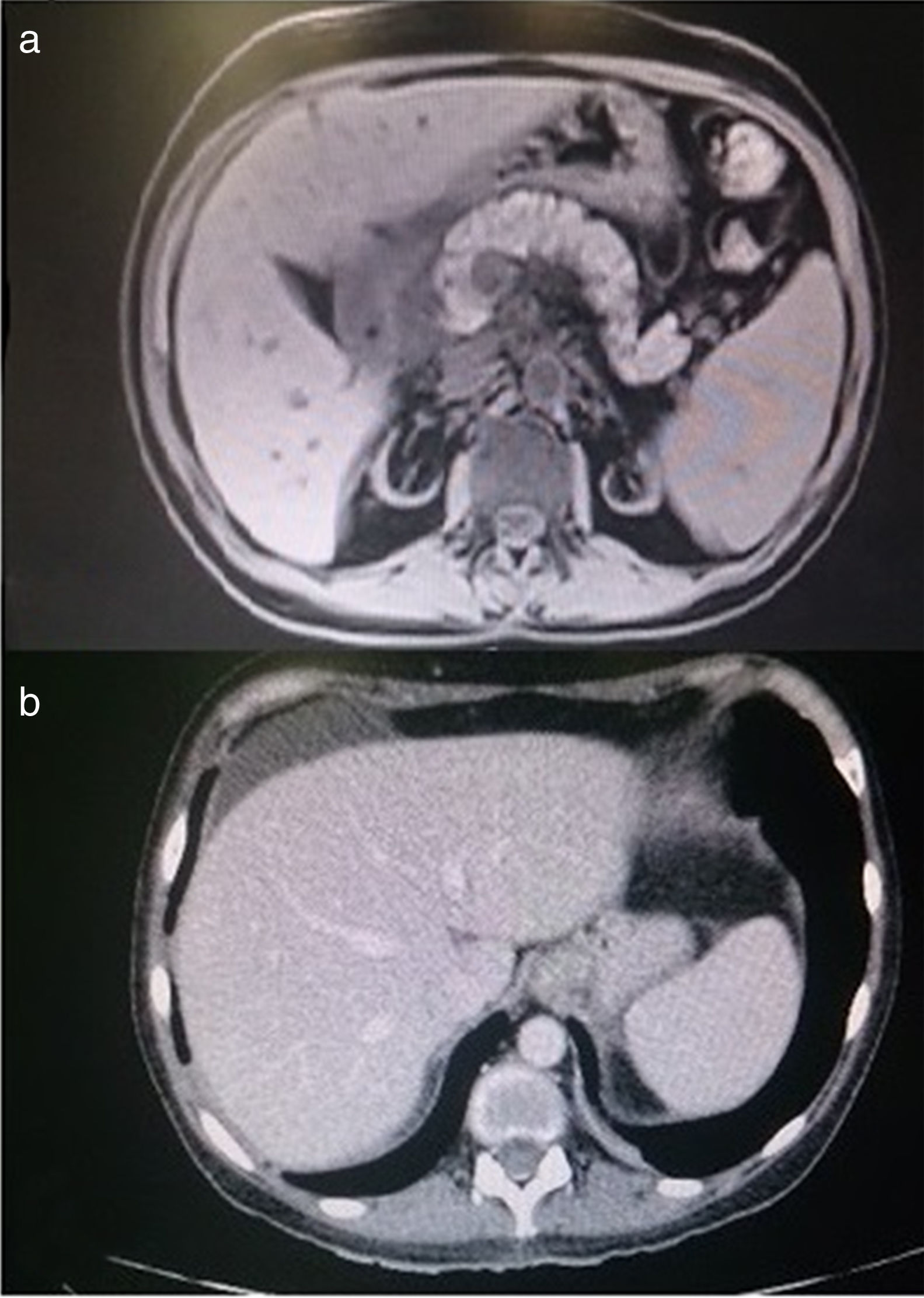
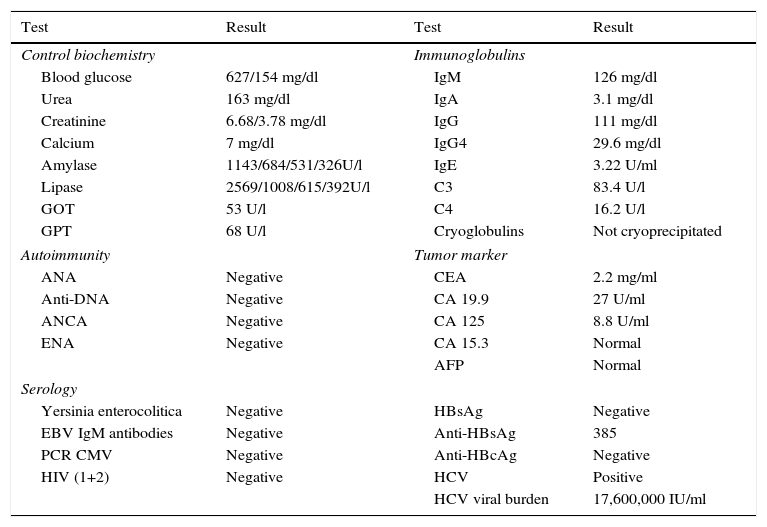
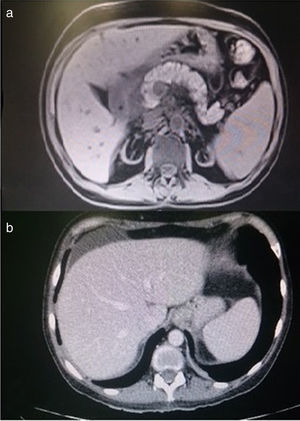
Complementary tests: Blood chemistry: glucose 106mg/dl, urea 163mg/dl, creatinine 3.74mg/dl, amylase 631 IU/l, lipase 1027 U/l, GOT 53 U/l, GPT 68 U/l, GGT 196 U/l, ALP 80 U/l, LDH 676 U/l, calcium 6.3mg/dl, CRP 1.07mg/l, and normal sodium, potassium, and coagulation. Hemogram: Hb 12.1g/dl, Htc 38.5%, MCV 99 fl, leukocytes 10,050μl, neutrophils 8,610μl, and platelets 100,000μl. PCR CMV was negative. HCV viral load 17,600,000 IU/ml. Autoimmunity and tumor markers were normal (Table 1). Abdominal CAT, NMR of the pancreas, and MR cholangiography of the bile ducts: consistent with acute interstitial pancreatitis with a low severity index (Figure 2a and b). Endoscopic ultrasound was normal. The patient's blood chemistry and imaging results were consistent with mild interstitial acute pancreatitis, according to the Atlanta criteria. Exudate cultures from the lower extremities were negative for bacteria and fungi.
Laboratory test results.
| Test | Result | Test | Result |
|---|---|---|---|
| Control biochemistry | Immunoglobulins | ||
| Blood glucose | 627/154 mg/dl | IgM | 126 mg/dl |
| Urea | 163 mg/dl | IgA | 3.1 mg/dl |
| Creatinine | 6.68/3.78 mg/dl | IgG | 111 mg/dl |
| Calcium | 7 mg/dl | IgG4 | 29.6 mg/dl |
| Amylase | 1143/684/531/326U/l | IgE | 3.22 U/ml |
| Lipase | 2569/1008/615/392U/l | C3 | 83.4 U/l |
| GOT | 53 U/l | C4 | 16.2 U/l |
| GPT | 68 U/l | Cryoglobulins | Not cryoprecipitated |
| Autoimmunity | Tumor marker | ||
| ANA | Negative | CEA | 2.2 mg/ml |
| Anti-DNA | Negative | CA 19.9 | 27 U/ml |
| ANCA | Negative | CA 125 | 8.8 U/ml |
| ENA | Negative | CA 15.3 | Normal |
| AFP | Normal | ||
| Serology | |||
| Yersinia enterocolitica | Negative | HBsAg | Negative |
| EBV IgM antibodies | Negative | Anti-HBsAg | 385 |
| PCR CMV | Negative | Anti-HBcAg | Negative |
| HIV (1+2) | Negative | HCV | Positive |
| HCV viral burden | 17,600,000 IU/ml | ||
Diagnosis was pancreatic panniculitis secondary to idiopathic mild acute pancreatitis (autoimmune, neoplastic, or paraneoplastic pancreatic disease were ruled out) in a kidney transplantation patient with graft function loss and chronic hepatitis from HCV infection.
The patient progressed favorably with analgesic and prednisone treatment and was released on day 20. She presented with the following complications: Enterobacter cloacae infection of the inferior limb lesions, transitory hyperglycemia, and herpes keratitis that responded to acyclovir. Together with the resolved pancreatitis, the patient had a gradual decrease in the pancreatic enzyme levels and disappearance of the skin lesions. Pancreatic panniculitis or pancreatic fat necrosis is a rare complication (2-3%) of certain pancreatic diseases and is often lethal. It has been described in the course of acute pancreatitis, chronic pancreatitis, and pancreatic carcinoma, and less frequently in pancreatic pseudocyst, vascular-pancreatic fistulas, pancreas divisum, and certain drugs (corticoids, thiazides, azathioprine, cyclosporine, oral contraceptives, NSAIDs).1–3 Cases of pancreatic panniculitis associated with solid organ transplants or digestive tract neoplasias have been published.4 It presents with greater frequency between the 4th and 6th decades of life, more often in men. The cases associated with pancreatic carcinoma usually present at more advanced ages. Clinical manifestation is the appearance of painful purplish-erythematous nodules in the decubitus compression areas. A high degree of suspicion is necessary, given that it is clinically indistinguishable from other types of panniculitis, such as nodular erythema. The pancreatic panniculitis nodules can ulcerate and produce a sterile and oleous discharge. They tend to involute, leaving cutaneous hyperpigmentation. The cutaneous manifestations frequently precede the gastrointestinal ones. Systemic symptoms can be fever, polyarthritis, serositis, eosinophilia and/or abdominal pain, and nervous system involvement with demyelinating lesions. The cases due to neoplasia have a more florid clinical presentation, with altered blood chemistry tests showing eosinophilia, and torpid progression. Amylase and lipase levels can be normal or elevated. Pathogenesis is uncertain and it is postulated that the pancreatic enzymes released into the blood are responsible for the necrosis of the distant subcutaneous cellular tissue. There could be previous damage to the walls of the blood vessels from an infection or the immunologic mechanism mediated by immune complexes. Histopathology is characteristic and essential for diagnosis. Lobulillar panniculitis tends to be observed in the first period, then vasculitis, infiltrates, ghost cells (adipocytes partially digested by the enzymes), and calcifications. Management consists of supportive measures and the search for the underlying disease for its treatment. Neoplasia must always be ruled out. We present the case herein, due to the low frequency of the disease and the importance of its diagnosis for treatment. Our patient had undergone a kidney transplantation. She developed pancreatic panniculitis that presented with asymptomatic pancreatitis and kidney transplantation dysfunction and she was treated with furosemide, corticoids, and mycophenolate. We found 5 cases of pancreatic panniculitis in kidney transplantation patients in the literature,5–7 2 of which also had transplantation of the pancreas.8,9 They coincided with the clinical features of graft dysfunction or rejection, supporting the immunologic mechanism in its pathogenesis that could be considered an alarm symptom for a probable graft rejection. Increased levels of pancreatic enzymes have been observed in HCV positive patients, which we postulate as another possible pathogenesis in the present case.10 Currently, treatment of kidney transplant HCV patients is proposed.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank all the Internal Medicine personnel of the Hospital Torrecárdenas, Almería, the Pathologic Anatomy personnel of the Hospital Torrecárdenas and the Centro de Salud, Almería, as well as all our patients.
Please cite this article as: Ramírez-Arriola MG, Moreno-Barón M, Ruz-Legaza M, Casado-Martín M, Abad Vivás-Pérez JJ. Nódulos eritematosos en miembros inferiores en paciente trasplantada renal. Revista de Gastroenterología de México. 2017;82:353–356.