Internal hernias consist of the protrusion of an organ through a congenital or acquired mesenteric or peritoneal opening. Their incidence is estimated at 0.5–4.1 % and they are responsible for 5.8 % of small bowel obstructions. The mortality rate is above 50 % when there is vascular involvement.1,2 Foramen of Winslow hernias account for close to 8 % of internal hernias. They present in patients of either sex between 20 and 60 years of age.3,4 Identifying an omental foramen in the preoperative evaluation is a diagnostic challenge and is achieved in less than 10 % of cases that are confirmed in the intraoperative findings.5
We present herein a clinical case to describe the clinical presentation, diagnostic approach, and definitive management of that rare entity.
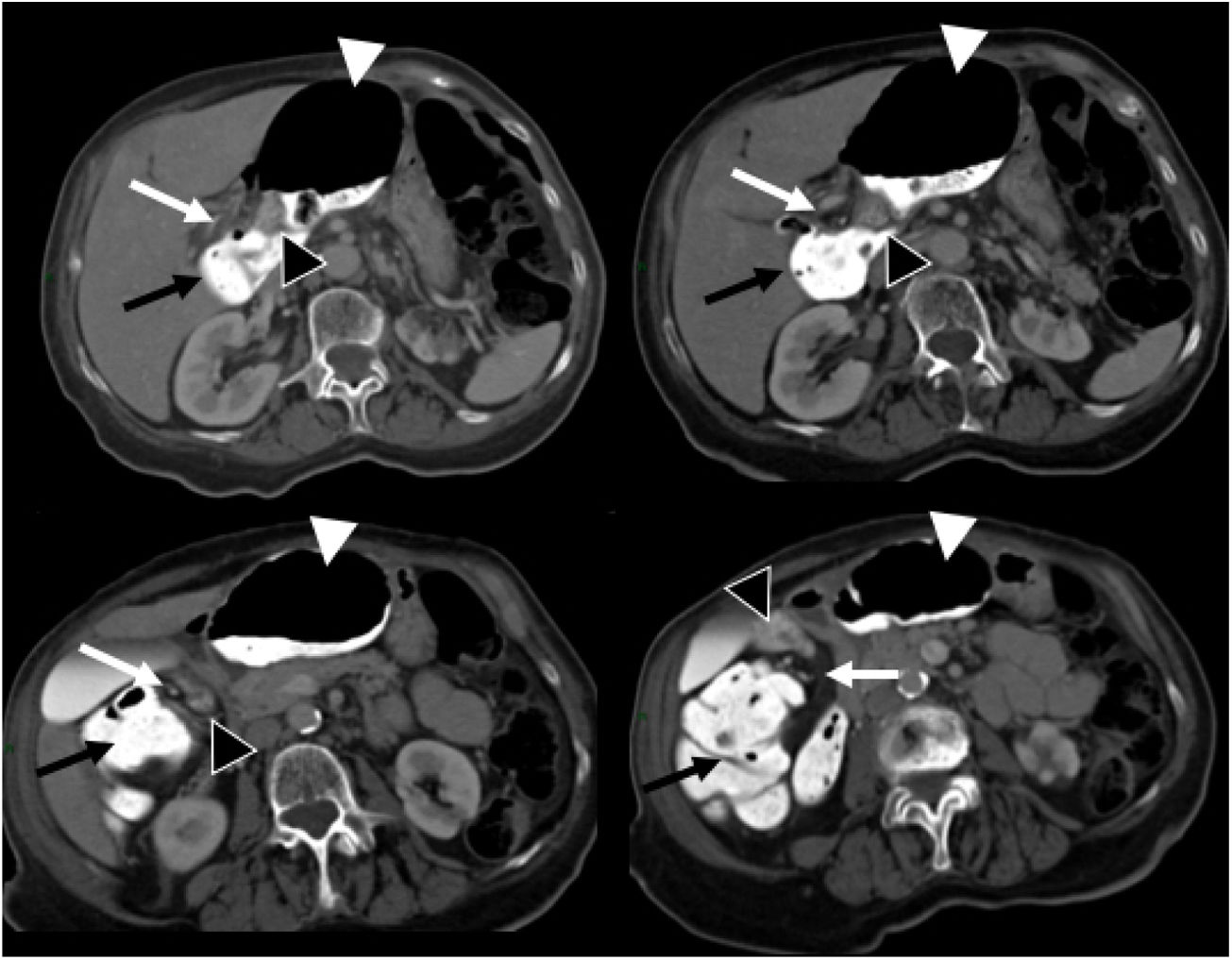
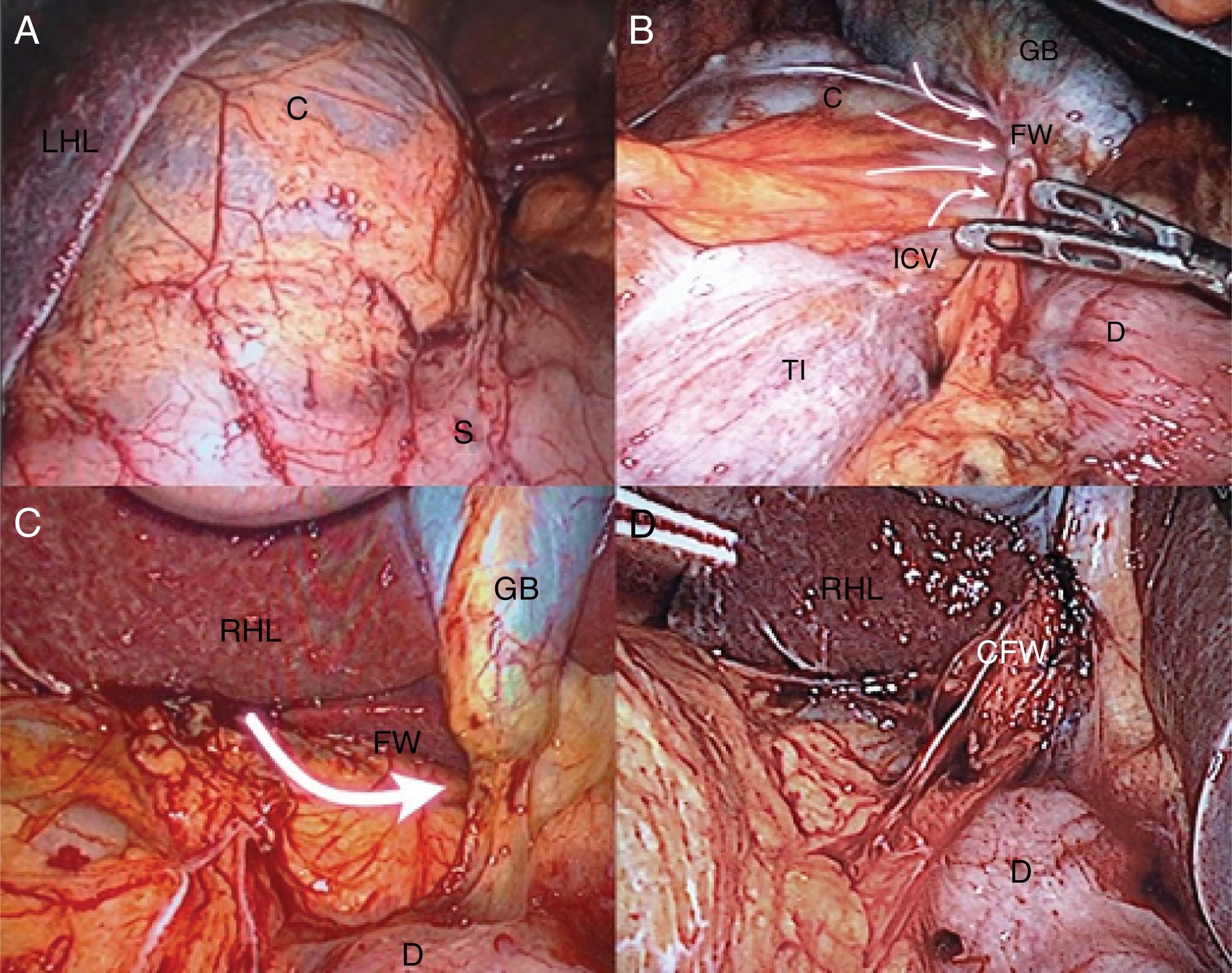
An 80-year-old woman, with a history of high blood pressure and open appendectomy at 35 years of age, sought medical attention at the emergency service for symptoms of 24-h progression characterized by progressive, colicky abdominal pain located in the mesogastrium, radiating into the right dorsolumbar region. She had no other associated symptomatology, nor clinical signs suggesting bowel obstruction. Physical examination revealed unaltered vital signs, a soft tumor in the epigastrium, reduced peristaltic sounds, pain in the right hemiabdomen upon palpation, and no signs of peritoneal irritation. The laboratory test results showed: hemoglobin, 11.1g/dl; leukocytes, 16.2×103/mm3; neutrophils, 91.7 %; and lymphocytes, 5.9 %. An abdominal computed tomography (CT) scan with oral and intravenous contrast medium showed findings related to a herniation of the ileocecal valve and cecum through the foramen of Winslow, with no signs of intestinal segment compromise (Fig. 1). A diagnostic laparoscopy was performed, revealing a foramen of Winslow hernia whose content included the ileocecal valve and cecum (Fig. 2). The herniated content was reduced, and viable intestinal segments were found. The foramen was closed utilizing interrupted sutures with nonabsorbable monofilament. The patient had satisfactory postoperative progression and was released from the hospital 48h after surgery.
Computed tomography superior to inferior sequential axial views of the abdomen in the venous phase with oral contrast medium. Fat and mesenteric vessels (white arrow) protruding through the foramen of Winslow into the hepatogastric space, together with the terminal ileum and ileocecal valve (black arrowhead), cecum (white arrowhead), and ascending colon (black arrow) in the hepatogastric space, displacing the stomach to the left. Findings are consistent with an internal hernia through the foramen of Winslow.
A) Bulging over the hepatogastric ligament (lesser sac). C: cecum; LHL: left hepatic lobe; S: stomach. B) Hernia of the cecum and ileocecal valve through the foramen of Winslow (arrows). C: cecum; D: duodenum; FW: foramen of Winslow; GB: gallbladder, ICV: ileocecal valve, TI: terminal ileum. C) View of the foramen of Winslow after the reduction of the herniated content (arrow). D: duodenum; FW: foramen of Winslow; GB: gallbladder; RHL: right hepatic lobe. D) Surgical closure of the foramen of Winslow. CFW: closed foramen of Winslow; D: duodenum; RHL: right hepatic lobe.
Foramen of Winslow hernias are a variant of abdominal internal hernias that occur upon the displacement of intra-abdominal visceral content through the orifice communicating the abdominal cavity per se with the lesser sac. The etiopathogenesis of that anatomic abnormality is associated with 4 factors: a) an increase in the diameter of the foramen of Winslow, b) a lax and mobile ascending colon due to the lack of fusion of the colon with the posterior abdominal wall, c) the presence of a common mesentery in the entire intestine, and d) a lax and mobile small bowel due to the abnormalities in the length of the mesentery.6 Since the first report by Blandin in 1834, approximately 200 cases have been registered in the medical literature.3,7 Foramen of Winslow hernias more frequently affect the small bowel (60–70 %), followed by the cecum and ascending colon (25–30 %).8 Their clinical presentation depends on the compromised organ and can be accompanied by abdominal pain, nausea, and vomiting, as signs of bowel obstruction. Physical examination and laboratory test findings tend to be nonspecific.5 CT is considered the imaging study of choice and can reveal the absence of the ascending colon in the right paracolic gutter, the anterolateral displacement of the stomach, signs of small bowel obstruction, and air-fluid levels in the lesser sac, among other findings.7 Surgical treatment consists of the careful reduction of the herniated content when tissues are found to be viable, and if they are not, resection of the affected segment is required. Fixation of the right colon and cecopexy to the lateral wall of the abdomen have been reported as part of the management, as well as the definitive closure of the foramen of Winslow.9 In 2011, Van Daele et al.10 described the first laparoscopic treatment, and since then, 11 cases of successful laparoscopic management have been reported, suggesting that approach as an initial alternative in the treatment of those patients.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have treated all patient data with confidentiality and anonymity, following the protocols of their work center.
Right to privacy and informed consent. The authors have followed the protocols of their work center in relation to the publication of patient data, preserving patient confidentiality and anonymity.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Bautista-Álvarez FE, Pérez-Soto RH, Clemente-Gutiérrez U, Hernández-Villegas AC, Sierra-Salazar M. Hernia del foramen de Winslow: causa poco frecuente de abdomen agudo. Revista de Gastroenterología de México. 2020;85:360–362.