Fournier's gangrene is a necrotizing fasciitis of the genital area. It progresses rapidly and its etiology is polymicrobial. The bacteria, aerobic and anaerobic, act synergically, causing great tissue destruction, and Escherichia coli is the most frequently identified microbe.1 We present herein a case of Fournier's gangrene due to Streptococcus anginosus, an exceptional microorganism in this pathology.
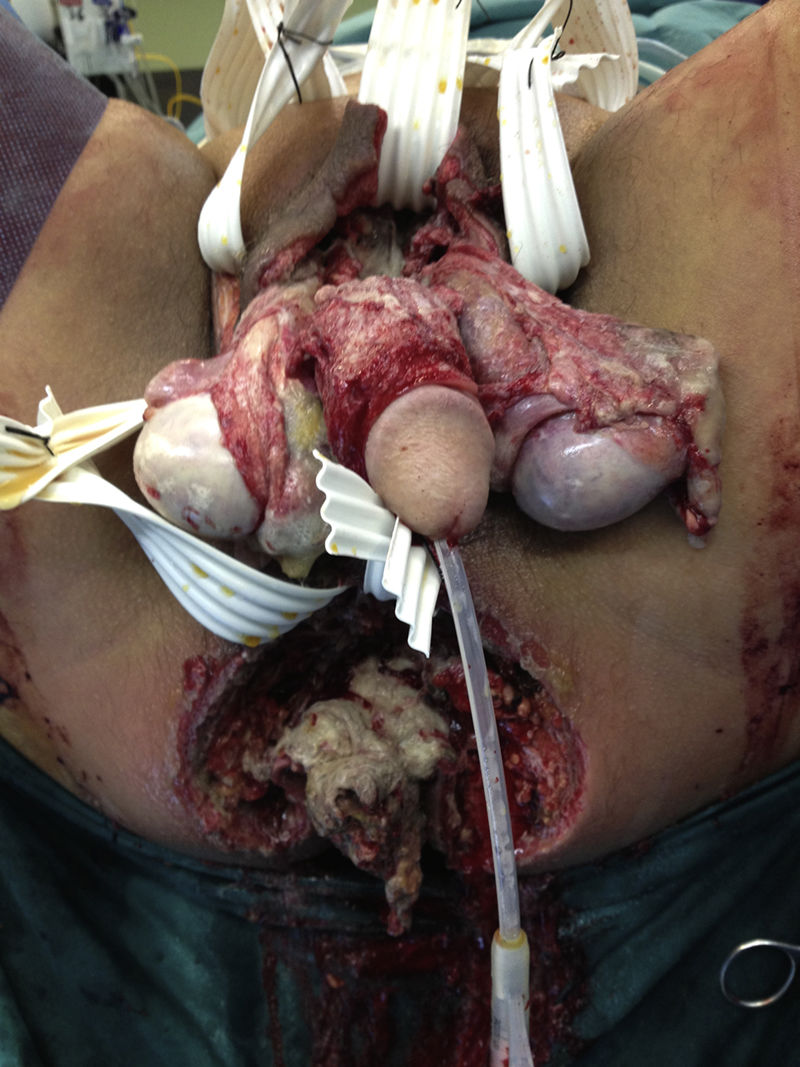
A 56-year-old man, a smoker and occasional drinker, had a past medical history of meningoencephalitis of probable herpetic origin. In 2006, he was seen at the internal medicine department for gastric and duodenal ulcers and secondary iron-deficiency anemia (normal colonoscopy in 2006). In relation to his present illness, he came to the emergency department for pain in the perianal and genital area and increased scrotal volume associated with fever of 38°C. Upon physical examination, the patient was hemodynamically stable, afebrile, and he had scrotal and perianal necrotic plaque in a horseshoe formation, with scrotal and penile edema and cellulitis that extended to the hypogastrium. The laboratory work-up results were leukocytosis (23,600 mm3) with left shift and C-reactive protein (CRP) of 38. An abdominopelvic computed axial tomography scan showed an increase in soft tissue in the anal region related to an infectious inflammatory process, with a great quantity of air in the right ischioanal fossa and root of the corpora cavernosa that extended into the perianal soft tissue and both sides of the scrotal sac, as well as into the subcutaneous cellular tissue in the area of the right gluteus and anterior abdominal wall at the level of the hypogastrium. He also presented with diffuse edema of the subcutaneous cellular tissue of the anterior, posterior, and left lateral abdominal wall. The patient was diagnosed with severe sepsis secondary to Fournier's gangrene. His fluid and electrolyte balance was restored and broad-spectrum antibiotic therapy was begun. Emergency surgery was performed via perineal access and right iliac fossa (RIF) incision. During the procedure, abscess-cellulitis and necrosis at the level of both ischioanal fossae were found that extended to the testes and penis, causing ample plaques of cutaneous and soft tissue necrosis, also extending to both sides of the groin and to the pubis with fetid, subcutaneous necrosis. The perianal involvement separated the anterior rectal surface that presented with fat necrosis. The external genitalia were edematous, with necrotic plaques on both testes. Cellulitis was present in the proximal ends of the lower limbs, abdomen, and abdominal flanks, and reached the umbilical region. Ample cutaneous and subcutaneous debridement of the entire affected area was performed, a silastic drain was placed in the suprapubic region, and diverting loop colostomy in the left iliac fossa (LII) was carried out to isolate the perineum and enable better control of the septic focus at that level (figs. 1 and 2).
The patient was postoperatively admitted to the intensive care unit, continuing the restoration of fluid and electrolyte balance and hemodynamic support with vasopressors. He had good diuretic response and adequate peripheral perfusion. The antibiotics daptomycin, metronidazole, and imipenem were empirically administered to eradicate the polymicrobial flora and there was good control of the signs of sepsis. Multisensitive Streptococcus anginosum (an uncommon microbe in this pathology) was isolated from the wound exudate. Antibiotic treatment was adjusted (the antibiogram showed sensitivity to cefotaxime, ceftriaxone, clindamycin, vancomycin, erythromycin, and penicillin), completing the 12-day treatment cycle with imipenem as monotherapy. The patient had good respiratory progression, with a gradual decrease in respiratory support, and was extubated after 9 days of mechanical ventilation.
Once the patient had adequate sepsis control and his wounds were properly cleaned and debrided and had negative cultures, partially thick skin grafts were applied in a joint intervention with the plastic surgery department. The remainder of the postoperative period was unremarkable, and the patient was released from the hospital 41 days after his admission.
Fournier's gangrene is an infrequent pathology that has a 10:1 predominance in males.2
Patients with alcoholism, diabetes, malnutrition, or neoplasias are more highly predisposed to develop this pathology and its entryway tends to be a mild wound at the genital level. Symptoms also frequently develop from anal abscesses or fistulas, bowel perforations (of any etiology), or hidradenitis. Prognosis is worse when the focus is anal or rectal.3
Surgical treatment in cases of Fournier's gangrene should be early and aggressive and reconstruction is dependent on the degree of tissue destruction. In severe cases, it is done through free skin grafts, and musculocutaneous grafts are used to cover deep defects.4
Etiology is polymicrobial. In the majority of patients, multiple aerobic and anaerobic microorganisms that often act synergically are isolated. According to a study by Cohen MS, the most frequently isolated aerobic pathogens are Gram-negative (E. coli, 47%), and Bacteroides (44%) are the most frequently isolated anaerobic pathogens. Streptococcus anginosus was the microorganism isolated in our case.5,6
The anginosus group streptococci are catalase-negative Gram-positive cocci in chains that belong to the genus Streptococcus.
Streptococcus anginosus forms part of the resident flora of the oronasopharynx, gingival sulci, gastrointestinal tract, and vagina and it can migrate from those sites and cause different pyogenic infections. Its role in severe pyogenic infections is recognized, unlike the rest of the microbes in the viridans streptococci group, but varies in accordance with different clinical symptoms. Its presentation as a causal agent of Fournier's gangrene is exceptional.7
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Soto-Sánchez A, Hernández-Barroso M, Hernández-Hernández G, Gambra-Michel L, Barrera-Gómez M. Gangrena de Fournier por Streptococcus anginosus, un agente etiológico poco habitual. Revista de Gastroenterología de México. 2018;83:348–350.