Endoscopic retrograde cholangiopancreatography (ERCP) is a complex procedure. Clinical guidelines assess competence in ERCP through a defined number of procedures, but multiple factors are involved. Our aim was to analyze the morphology of the papilla of Vater as an independent factor in selective common bile duct cannulation during resident training.
Material and methodsPatients that underwent ERCP were studied consecutively. All ERCPs were begun by a resident in training. The type of papilla was classified according to Haraldsson, including those with previous sphincterotomy. Cannulation difficulty and success and their relation to the type of papilla were documented. The analysis was divided into three 4-month periods.
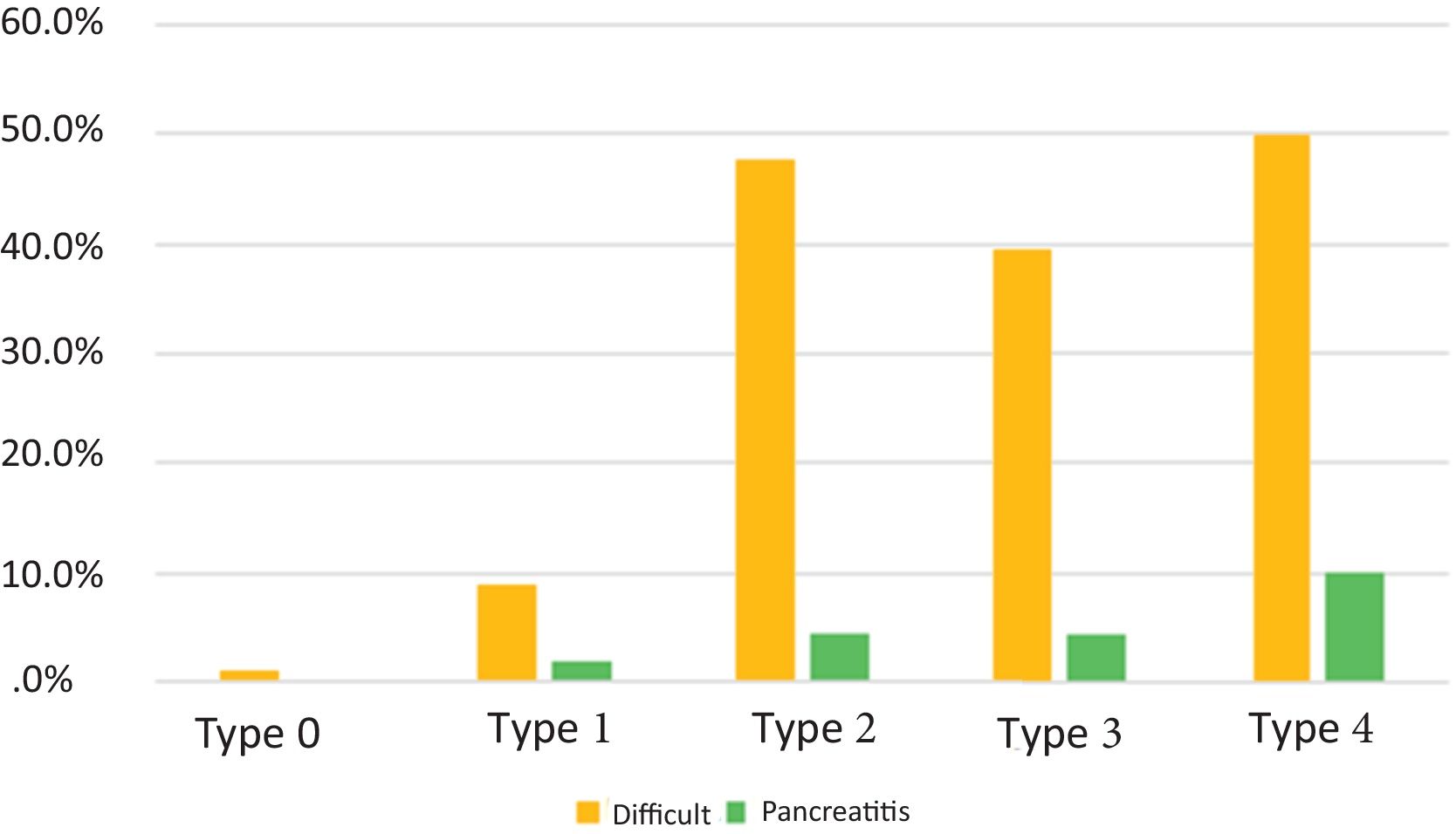
ResultsOf the 429 patients, cannulation was difficult in 101 (23.5%). The residents achieved selective cannulation of the common bile duct in 276 (64.3%) and the cannulation success rate at the end of their training was 81.7%. Cannulation was performed with the least difficulty in papillae with previous sphincterotomy (2.8%), unlike the type 4 papilla, which was difficult to cannulate in 50% of the cases. The lowest overall cannulation success was in the type 2 papilla (81.8%).
ConclusionPapilla type can influence cannulation success, but it is not the only related factor. Patients that underwent previous sphincterotomy appear to be the cases in whom ERCP training can be started.
La colangiografía retrograda endoscópica (CPRE) es un procedimiento complejo. Las guías clínicas evalúan la competencia en CPRE mediante un número definido de procedimientos, sin embargo, existen múltiples factores que influyen en ello. El objetivo fue analizar la morfología de la papila de Vater como factor independiente en la canulación selectiva del colédoco durante el entrenamiento del residente.
Material y métodosSe estudiaron pacientes sometidos a CPRE de manera consecutiva. Todas las CPRE fueron iniciadas por el residente. Se clasificó el tipo de papila según Haraldsson, incluyendo a las papilas con esfinterotomía previa. La dificultad, el éxito en la canulación y su relación con el tipo de papila fueron documentados. El análisis se dividió en tres períodos de cuatro meses.
ResultadosDe los 429 pacientes se determinó canulación difícil en 101 (23.5%). Los residentes lograron una canulación selectiva del colédoco en 276 (64.3%) y su éxito de canulación al final de su entrenamiento fue del 81.7%. La papila con esfinterotomía previa representó la menor dificultad en la canulación (2.8%), a diferencia de la papila tipo 4 que fue de canulación difícil en 50% de los casos. La papila tipo 2 presentó el menor éxito global de canulación (81.8%).
ConclusiónEl tipo de papila puede influir en el éxito de canulación, sin embargo, no es el único factor relacionado al éxito del mismo. Los pacientes con esfinterotomía previa parecen ser los indicados para iniciar el entrenamiento en CPRE.
Endoscopic retrograde cholangiopancreatography (ERCP) is a complex procedure with a significant risk for adverse events. There are numerous questions as to how basic and/or advanced ERCP training should be carried out, how to evaluate it, and what program meets the requirements for professors and facilities or resources for training physicians, as well as the requisites for the physician to be accepted into a program, how long the training should last, and which cannulation success percentage should be considered acceptable at the end of the training.1,2 The American Society for Gastrointestinal Endoscopy (ASGE) defines competence as the minimum level of knowledge and/or experience derived from training that is required to safely and efficiently perform a procedure. Currently, clinical guidelines grant competence in ERCP when a set number of procedure performances is reached.3–5 However, reaching a defined number of procedures does not guarantee clinical competence, making a curriculum with diverse variables and data before, during, and after the procedures necessary.6,7 The essential and often most complex step in ERCP is the selective cannulation of the bile ducts and/or pancreatic duct. Therefore, the aim of the present study was to evaluate the influence of the morphology of the papilla of Vater on the difficulty involved in the selective cannulation of the common bile duct during the ERCP training of two residents, in a prospective cohort of patients.
Material and methodsStudy designA prospective, observational study was conducted at the Hospital Universitario “Dr. José E. González”. The total number of ERCPs carried out within the time frame of March 1, 2020 to February 28, 2022 were consecutively counted.
Study subjectsThe advanced specialty program in advanced endoscopy is a one-year program and consists of a director (JAGG, with more than 20 years of experience in ERCP) and two professors (AGG, with > 15 years of experience and JJQ, with > 8 years of experience in ERCP), all of whom are certified by the relevant medical board. To be accepted into the advanced endoscopy program, residents must have completed a formal three-year program in gastroenterology, be board-certified, and possess basic knowledge, regarding upper endoscopy and colonoscopy.
All ERCPs were consecutively performed as part of the daily medical attention provided by the Gastroenterology and Endoscopy Service. The procedures were begun by the resident, and if necessary, continued by the professor. During the ERCP, the patient was placed in the left ventral decubitus position and given conscious sedation by an anesthesiologist. Fluoroscopy, a Fuji or Pentax duodenoscope, a wire-guided sphincterotome, contrast medium at 50%, and ERBE VIO 300 electrocautery were utilized in all the procedures. In addition, stones were extracted with a balloon extractor as a first choice and/or a Dormia basket, depending on the preference of the physician, and other accessories were used as needed. All patients in whom access during cannulation was difficult were given 100 mg of rectal indomethacin, during the procedure.
The variables analyzed were frequency of cannulation by the resident or cannulation by the professor, ERCP duration (time interval to cannulation – time interval to entrance of the cannulation device), and cannulation time (over or under 5 minutes). The type of papilla was classified, according to Haraldsson, arbitrarily modifying the classification to include papillae with previous sphincterotomy, as follows: type 0, previous sphincterotomy; type 1, regular papilla; type 2, small papilla (under 3 mm); type 3, a bulging and/or protruding papilla; and type 4, creased or ridged papilla8 (Fig. 1). Papilla type was defined by the professor in each of the procedures. The adverse events that occurred during and after the procedure were systematically documented. The training of each resident was divided into three four-month periods and the abovementioned variables were analyzed for each period.
According to the standards of the European Society of Gastrointestinal Endoscopy (ESGE) difficult cannulation is defined as that with one or more of the following variables: > 5 cannulation attempts; the cannulation attempt after visualization of the papilla takes > 5 min; and more than 1 unintended cannulation or opacification of the pancreatic duct.9 Overall cannulation success arbitrarily included the procedures in which both the resident and professor participated. Post-sphincterotomy bleeding was defined as immediate, when it occurred during the procedure; as early, when it occurred within the first 24 h after the procedure; and as late, when it occurred 24 hours post-ERCP. The diagnosis of post-ERCP pancreatitis was made utilizing the previously established criteria.10,11
Statistical analysisThe descriptive analysis was carried out through the evaluation of frequencies (%) and medians (q25-q75) or mean ± SD, accordingly. The comparison of the categorical variables was carried out through the chi-square test. SPSS version 22.0 (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY) software was used for the statistical analysis and statistical significance was set at a p < 0.05.
Ethical considerationsThe authors declare that this article contains no personal information that could identify the patients.
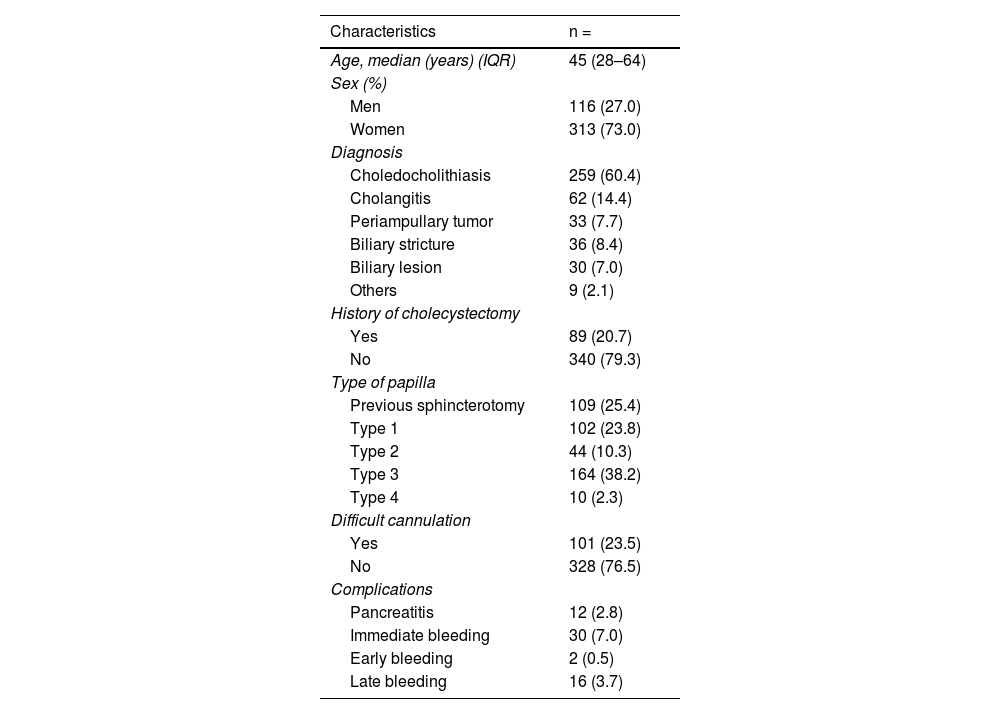
ResultsA total of 457 patients were evaluated. Twenty-eight patients were excluded for having unclassifiable papillae, leaving 429 patients to be studied. The median age was 45 years (range: 28-64) and 313 (73.0%) of the patients were women. The most frequent indication for ERCP was choledocholithiasis, present in 259 (60.4%) patients. Table 1 shows the clinical characteristics, diagnoses, papilla type, and complications.
Clinical characteristics of the 429 patients that underwent ERCP at a university center hospital in Northeast Mexico.
| Characteristics | n = |
|---|---|
| Age, median (years) (IQR) | 45 (28–64) |
| Sex (%) | |
| Men | 116 (27.0) |
| Women | 313 (73.0) |
| Diagnosis | |
| Choledocholithiasis | 259 (60.4) |
| Cholangitis | 62 (14.4) |
| Periampullary tumor | 33 (7.7) |
| Biliary stricture | 36 (8.4) |
| Biliary lesion | 30 (7.0) |
| Others | 9 (2.1) |
| History of cholecystectomy | |
| Yes | 89 (20.7) |
| No | 340 (79.3) |
| Type of papilla | |
| Previous sphincterotomy | 109 (25.4) |
| Type 1 | 102 (23.8) |
| Type 2 | 44 (10.3) |
| Type 3 | 164 (38.2) |
| Type 4 | 10 (2.3) |
| Difficult cannulation | |
| Yes | 101 (23.5) |
| No | 328 (76.5) |
| Complications | |
| Pancreatitis | 12 (2.8) |
| Immediate bleeding | 30 (7.0) |
| Early bleeding | 2 (0.5) |
| Late bleeding | 16 (3.7) |
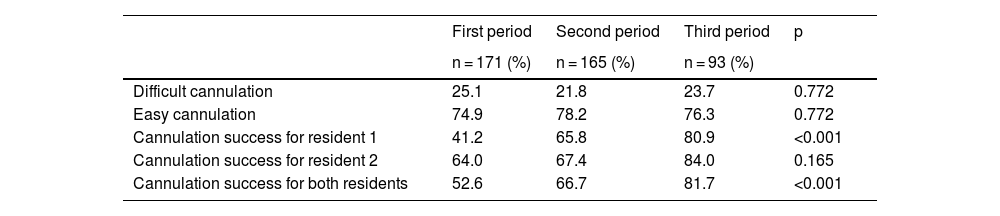
Of the 429 procedures, selective cannulation of the common bile duct was achieved by the residents in 276 (64.3%) and their successful cannulation (including papillae with previous sphincterotomy) in the first, second, and third periods was 90/171 (52.6%), 110/165 (66.7%), and 76/93 (81.7%), respectively (p < 0.001). Difficult cannulation was determined in 101 patients (23.5%) and the residents achieved cannulation in 13.9% of them. Of the 328 cases considered easy, the residents achieved selective cannulation of the common bile duct in 79.9% (p < 0.001). Table 2 shows the percentages of easy cannulation and difficult cannulation, as well as successful cannulation, in the three evaluation periods.
Percentage of difficult cannulation, cannulation success for each resident, and overall cannulation success in 429 cholangiographies in the 3 periods.
| First period | Second period | Third period | p | |
|---|---|---|---|---|
| n = 171 (%) | n = 165 (%) | n = 93 (%) | ||
| Difficult cannulation | 25.1 | 21.8 | 23.7 | 0.772 |
| Easy cannulation | 74.9 | 78.2 | 76.3 | 0.772 |
| Cannulation success for resident 1 | 41.2 | 65.8 | 80.9 | <0.001 |
| Cannulation success for resident 2 | 64.0 | 67.4 | 84.0 | 0.165 |
| Cannulation success for both residents | 52.6 | 66.7 | 81.7 | <0.001 |
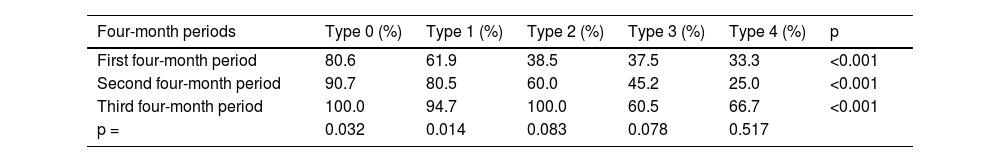
The most frequent papilla was type 3 (bulging, protruding, or Shar-Pei), with 164 (38.2%) cases, of which 60.4% were difficult cannulations. Cannulation success per resident was higher in the third training period (60.5% of the cases) and reached 93.4% when the professor intervened. A total of 109 (25.4%) cases had a type 0 papilla, or with previous sphincterotomy, with cannulation difficulty in 2.8%. The cannulation percentage of the residents in that type of papilla was 80% in the first period and 100% in the third period. Cannulation difficulty and success were different between the type of papilla and the period analyzed (tables 3 and 4).
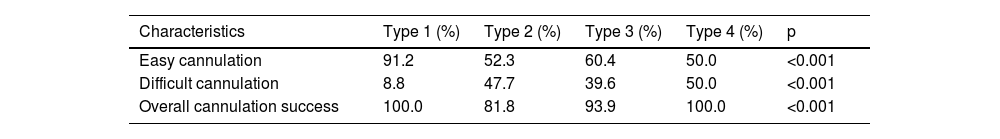
Percentage of difficult cannulation, easy cannulation, and overall successful cannulation in each type of papilla.
| Characteristics | Type 1 (%) | Type 2 (%) | Type 3 (%) | Type 4 (%) | p |
|---|---|---|---|---|---|
| Easy cannulation | 91.2 | 52.3 | 60.4 | 50.0 | <0.001 |
| Difficult cannulation | 8.8 | 47.7 | 39.6 | 50.0 | <0.001 |
| Overall cannulation success | 100.0 | 81.8 | 93.9 | 100.0 | <0.001 |
Percentage of resident cannulation success in each type of papilla over the 3 periods.
| Four-month periods | Type 0 (%) | Type 1 (%) | Type 2 (%) | Type 3 (%) | Type 4 (%) | p |
|---|---|---|---|---|---|---|
| First four-month period | 80.6 | 61.9 | 38.5 | 37.5 | 33.3 | <0.001 |
| Second four-month period | 90.7 | 80.5 | 60.0 | 45.2 | 25.0 | <0.001 |
| Third four-month period | 100.0 | 94.7 | 100.0 | 60.5 | 66.7 | <0.001 |
| p = | 0.032 | 0.014 | 0.083 | 0.078 | 0.517 |
Post-ERCP pancreatitis was diagnosed in 13/429 patients. In the first period, the frequency of post-ERCP pancreatitis was 8 (4.7%), in the second period it was 4 (2.4%), and in the third period it was 1 (0.2%) (p = 0.079). No patient with post-ERCP pancreatitis died and the mean hospital stay was five days. There was no statistically significant difference between post-ERCP frequency and type of papilla (p = 0.130) (Fig. 2).
Immediate post-sphincterotomy bleeding occurred in 30 patients, all of whom responded to endoscopic treatment. Early post-sphincterotomy bleeding presented in two patients and late bleeding in 18. All of those patients were treated conventionally; five of them required blood transfusion and none of them required radiologic and/or surgical intervention. There was no statistically significant difference in the frequency of bleeding by evaluation period (p = 0.523). However, upon analyzing the subgroup of patients with immediate post-sphincterotomy bleeding, depending on papilla type, that adverse event was more frequent in the type 3 papilla (20/164 [12.2%]) (p = 0.002).
Comparison between the two residents and cannulation success
Upon comparing the success of selective cannulation of the common bile duct between resident 1 and resident 2, for all three periods and in the last four-month training period, successful cannulation was 61.1% vs. 68% (p = 0.139) and 80.9% vs. 84%, respectively (p = 0.668). Cannulation was considered difficult in 26.2% of the procedures performed by resident 1 vs. 20.5% performed by resident 2 (p = 0.165). There was no statistically significant difference, with respect to the number of post-ERCP pancreatitis events (p = 0.721) or post-procedure bleeding between the two residents (p = 0.130).
DiscussionThe physician in advanced endoscopy training must fulfill certain standards to be considered qualified to perform ERCP.12 Gavin J et al. reported that an 80% success rate and less than a 10% post-ERCP pancreatitis rate is the desired goal in resident training.12 Despite the COVID-19 pandemic, it was possible to continue training residents, achieving an average of 228 ERCPs in one year and resulting in a successful cannulation rate of 80% and a post-ERCP pancreatitis rate of 3% at the end of training.
Selective cannulation of the papilla of Vater during ERCP is the greatest challenge in resident training. Recent studies have described the usefulness of different models that attempt to improve resident skills during their training.13 The anatomic characteristics and the position of the papilla of Vater can influence the success of bile duct cannulation and the complications of the procedure.14 Some studies have associated papilla morphology with selective cannulation success.15 We found that cannulation was less difficult in patients with previous sphincterotomy (2.8%), and together with similar results reported in other studies,6,16,17 starting training on those types of patients appears to be indicated.
In the first and third training periods, cannulation was more difficult in type 3 papillae, at close to 50% in both periods. Those findings are similar to results reported in the literature, showing that cannulation is difficult in 70% of cases with a type 2 or type 3 papilla.18
The type 3 papilla has a longer intramural length, and the common bile duct, because it has valves and folds, makes its cannulation more difficult, as was reported in 39.6% of cases.19 Upon finishing their training, the residents in our study achieved cannulation in 60% of the type 3 papillae. Difficult cannulation was most frequent in type 4 papillae (50%) and the residents achieved cannulation in 66% of those cases upon finishing their training. In cases of type 3 and type 4 papillae, the professor must carefully guide the resident, with respect to the approach and maneuvers that can facilitate the cannulation and reduce trauma in those papilla types.
The most frequent and dreaded complication in performing ERCP is pancreatitis, hence the importance of identifying both patient and procedure risk factors. In a recent study, a long/short axis ratio ≥ 1.5 in the morphology of the papilla and the absence of a periampullary diverticulum were reported to have a statistically significant impact on the development of post-ERCP pancreatitis.20 Interestingly, in our work, there was no statistically significant difference between episodes of post-ERCP pancreatitis and papilla type. However, it should be noted that a higher incidence of post-ERCP pancreatitis was documented in the first training period, suggesting that post-ERCP pancreatitis could be influenced by the experience of the endoscopist. Immediate post-sphincterotomy bleeding was more frequent in type 3 papillae, probably due to the longer intramural length of that type, requiring more extensive cutting in the sphincterotomy.
The strengths of our study are the fact that the residents completed an adequate number of procedures and that the different variables analyzed for attempting to determine whether papilla type influenced cannulation were obtained prospectively. The weaknesses of our analysis include the fact that only two residents were evaluated, an already established curriculum for evaluating the performance of the residents was not applied, and there was no information on patient progression at 30 days.
ConclusionPapilla type can influence cannulation success, but it is not the only related factor. Our study showed that the cannulation success of the residents, in each papilla type, improved over time. Understanding the factors that influence advanced endoscopy training will lead to better development of academic programs and strategies for improving resident training.
Financial disclosureNo financial support was received.
Conflict of interestThe authors declare that there is no conflict of interest.