Primary lymphoma of the appendix is an extremely rare entity that accounts for approximately 0.015% of the lymphomas of the gastrointestinal tract. There are very few published reports of the pathology. Burkitt's lymphoma is more frequent in children, whereas the majority of cases in adults correspond to large B-cell non-Hodgkin lymphoma.1–4
The majority of articles found in the international literature correspond to case reports. In the case series by Marcelo Zamorano et al., from a total of 7626 appendectomy specimens, there were only 25 appendiceal tumors and just 2 of them were primary lymphomas.5 In another case series that included 5307 appendectomy specimens, Daniel Esmer et al. found a total of 31 cases (0.58%) of appendiceal tumor, none of which corresponded to appendiceal lymphoma.4 A total of 1060 appendectomy specimens were reviewed over a 10-year period at the Kamineni Hospitals in India and only one case of appendiceal lymphoma was found,1 illustrating the rareness of the pathology.
We present herein the case of a 40-year-old woman with unremarkable past history/comorbidities. She arrived at the emergency department with 10-day progression of abdominal pain that began insidiously and gradually became more intense in the right iliac fossa, accompanied by anorexia, nausea, vomiting, and undetermined fever. Physical examination revealed a mass in the right lower quadrant that measured approximately 10cm in diameter. It was semisolid, with poorly-defined borders, and was painful upon superficial palpation.
Laboratory work-up results were: hemoglobin 10.4g/dl, hematocrit 33.3%, platelets 332,000, leukocytes 12,400, neutrophils 77%, glucose 100mg/dl, uric acid 3.9mg/dl, cholesterol 124mg/dl, triglycerides 67mg/dl, creatinine 0.64mg/dl, urea 23.5mg/dl, ureic nitrogen 11mg/dl, PT 18.4seconds, INR 1.45, and PTT 42.2seconds.
No preoperative imaging studies were carried out, given that symptoms were highly suggestive of acute appendicitis.
Exploratory laparotomy revealed a tumor that was dependent on the cecal appendix at its middle and distal third, measuring approximately 5 x 3cm. It had an irregular appearance and was friable and bloody (figs. 1 and 2). Appendectomy was performed with primary closure employing the modified Pouchet technique. The patient was released on the following day with no complications.
At the check-up 2 weeks after surgery, the patient's general condition was good, with no postoperative complications.
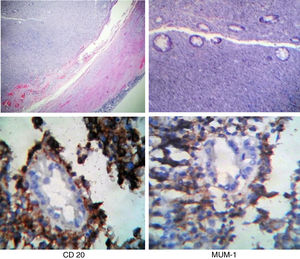
The histopathologic report stated large B-cell non-Hodgkin lymphoma. A postoperative CAT scan showed no tumor activity at another level and immunohistochemistry was positive for CD20, MUM-1, and CD 138 and positive for Ki67 in 70% of the specimen (fig. 3). The patient was referred to the medical oncology service and received CHOP chemotherapy plus 8 cycles of rituximab and complementary radiotherapy.
In the majority of cases, appendiceal lymphomas, like all tumors of the appendix, present with symptoms of acute appendicitis.1,6 Other less frequent symptoms are anorexia, weight loss, gastrointestinal bleeding, and intussusception.6
Appendiceal tumor is generally an intraoperative diagnosis. When suspected preoperatively, CAT is a useful study that can reveal a diffuse enlargement of the appendix, maintaining its vermiform shape with thickening of the wall and periappendiceal tissue, which can signify periappendiceal inflammation or lymphomatous infiltration. There can also be an increase in the focal size of the appendix.7–9 However, all those findings are not specific for appendiceal lymphoma, given that they can also be found in other neoplasias, and even in a true case of acute appendicitis. Thus, histopathologic study is essential for diagnosis.
When lymphoma of the appendix is diagnosed, its presence at another level must be ruled out through imaging studies, as well as through immunohistochemistry that is positive for CD20, CD5, CD10, and Bel6. In addition, it aids in ruling out more common neoplasias, such as neuroendocrine carcinoma and poorly differentiated adenocarcinoma.9
Immunocompromised patients, especially those with HIV, can present with atypically located lymphoma, and therefore it is necessary to perform ELISA and Western Blot tests for ruling out another possible diagnosis.10
The surgical conduct to follow regarding appendiceal tumors is a subject of debate.11 Some authors state that right hemicolectomy with lymph node extirpation is necessary in cases of appendiceal tumors larger than 2cm, tumors infiltrating the mesoappendix, when the cecum is compromised, or when there is a high mitotic index,12 whereas others believe that simple appendectomy with stump closure should be performed, holding off definitive treatment until there is a histopathologic result.13
In our case, appendectomy was performed, and postoperative chemotherapy was applied, once we had the histopathologic result of primary lymphoma of the appendix. Medical treatment should be carried out according to clinical stage and histologic type.
Diagnosis of primary lymphoma of the appendix is usually made through postoperative histopathologic study and therefore its routine performance is indispensable in all cases of extirpated cecal appendix.5
Primary lymphoma of the appendix is an extremely rare pathology. It is diagnosed once the presence of lymphoma in another location has been ruled out. Its presentation in the majority of cases is in the context of acute appendicitis, which is why it is diagnosed postoperatively through histopathologic study.9 Approximately 2 to 6% of patients with acute appendicitis have a palpable mass, described as a phlegmon or abscess, of which 6 to 12% correspond to an appendiceal tumor,14 as occurred in our patient. There is still controversy about the surgical treatment of tumor of the appendix. We decided to perform simple appendectomy and wait for the histopathologic result to determine the definitive treatment. That appears to be a good alternative for managing a well-defined appendiceal tumor that is an intraoperative finding and no accurate histopathologic diagnosis has been made.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: García-Norzagaray JC, Villalobos-López JA, Flores-Nájera H, Valle Leal JG, García Torres CD. Linfoma primario de apéndice: reporte de un caso y revisión de la literatura. Revista de Gastroenterología de México. 2019;84:255–257.