Eosinophilic esophagitis (EoE) has been a well-recognized pathologic entity in adults since 1978. Its clinical characteristics, treatment, and progression have been extensively studied over the last years. However, it has recently been described to form part of a group of clinical entities characterized by the infiltration of eosinophils in the esophageal mucosa together with gastroesophageal reflux disease (GERD) and proton-pump inhibitor-responsive esophageal eosinophilia (PPI-REE). Based on the above, we decided to present herein the case of a patient with esophageal eosinophilic infiltration diagnosed with PPI-REE, given his favorable response to these drugs.
A 50-year-old man sought medical attention due to intermittent dysphagia, retrosternal pain, and heartburn. He had a past history of hemorrhoidectomy and appendectomy years before and seafood allergy. Six months earlier, he had been seen by another gastroenterologist for the same symptoms, underwent endoscopy with no esophageal biopsy, was diagnosed with esophageal candidiasis, and prescribed oral nystatin. His blood count and biochemical profile were normal.
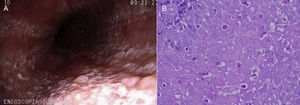
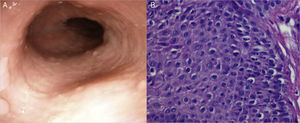
We decided to perform another endoscopy and it revealed an abundant whitish mottled pattern in the esophageal mucosa with some areas of exudate and edema (Fig. 1A). No hiatal hernia or erosions were observed and the junctional epithelium had a normal aspect. Eight biopsy samples were taken from the mucosa of the upper and lower third of the esophagus and the pathologist reported the presence of an abundant eosinophilic infiltrate in the epithelium (from 18 to 52 per high power field [HPF]) (Fig. 1B). Twenty-four hour esophageal pH impedance monitoring was normal. The patient was treated with 40mg of oral pantoprazole every 12h for 2 months. After that treatment, endoscopy with biopsy was repeated, which showed endoscopic improvement of the mucosa (Fig. 2A), and in the biopsy there was significant reduction of the eosinophilic infiltrate (1 to 3 eosinophils per HPF) (Fig. 2B). The patient stated that he had a significant decrease in the intensity of the dysphagia and heartburn (from 9 to 1 on the Visual Analogue Scale). Four months after proton pump inhibitor (PPI) suspension the patient was asymptomatic.
A) Aspect of endoscopy performed before PPI treatment, showing edema, erythema of the mucosa, with a whitish mottled pattern and exudates. B) Aspect of the esophageal mucosa biopsy before PPI treatment. Note the large quantity of eosinophils infiltrating the epithelium. The count was 18 to 52 per HPF.
In prospective studies conducted in Mexico, the prevalence of EoE in patients that undergo endoscopy and biopsy due to diverse esophageal symptoms or refractory GERD is low, from 4 to 6%.1,2 In our country, this disease is rarely diagnosed, as it is still not taken into consideration as a probable diagnosis, as could have occurred with our patient. The number of cases diagnosed would possibly increase if esophageal biopsies were taken in those patients with risk factors (young males with dysphagia, impaction, and/or atopy).2
In the 2007 consensus, the following were established as EoE diagnostic criteria: the presence of symptoms, with>15 eosinophils per HPF in the esophageal biopsy and the clinical and histologic non-response to PPI treatment. The purpose of the latter measure was to rule out GERD.3 It has recently been demonstrated that only 50 to 65% of the cases of esophageal eosinophilia in adults are due to EoE, and in the others, the cause is not only GERD, but also a new entity identified as PPI-REE.4,5 In these patients, outpatient esophageal pH monitoring is useful (as was the case with our patient) for ruling out GERD.
In the 2011 Consensus, PPI-REE was recognized as a condition that was probably different from EoE and GERD.6 Recent studies in Europe and the U.S. have confirmed the presence of PPI-REE as a phenotype among patients suspected of having EoE. The prevalence in these case series is from 35 to 43%, strengthening the importance of PPI administration before establishing an EoE diagnosis.7 It is thought that GERD could be a triggering event of the disease by damaging the esophageal epithelial barrier and allowing the exposure of the mucosa to food allergens, which would explain its sensitivity to PPIs.8 On the other hand, it has been suggested that PPIs could have an anti-inflammatory effect unrelated to acid secretion. It has been demonstrated that PPIs reduce eotaxine-3 expression, blocking the inflammatory cytokines of the Th2 pathway (IL4 and IL13) in the esophagus in a similar manner to what occurs in EoE after administrating topical steroids.9
PPI-REE is clinically and endoscopically indistinguishable from EoE and the importance of recognizing it lies in preventing the over-diagnosis of EoE and administrating unnecessary treatments that are not exempt from toxicity, such as topical steroids, or placing patients on elimination diets, as happened in the case of our patient. Nevertheless, it is not known whether the progression of this illness is similar to that of EoE in relation to recurrence and esophageal remodeling, and thus its long-term treatment is not yet known.10
Our case demonstrates the fact that in all patients with esophageal eosinophilia, GERD must initially be ruled out through ambulatory esophageal pH monitoring. If that test is negative, PPIs should be administered for a period of 2 months, after which esophageal endoscopy and biopsy should be repeated to discern between EoE and PPI-REE. Future prospective studies should confirm the effectiveness of this diagnostic and treatment strategy.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: García-Compeán D, González-González JA, González-Moreno EI, Barrera-Villarreal E, Maldonado-Garza HJ. Eosinofilia esofágica sensible a inhibidores de la bomba de protones. ¿Nueva entidad en busca de reconocimiento? Revista de Gastroenterología de México. 2016;82:113–115.