Functional gastrointestinal disorders (FGIDs) are complex illnesses characterized by gastrointestinal symptoms, with no underlying organic pathology. They are common, chronic, recurrent, and disabling disorders that significantly impair quality of life (QoL). The aim of the present cross-sectional analytical study was to assess QoL and its correlates in adult patients with FGIDs.
Materials and methodsA cross-sectional, observational, hospital-based study was conducted at the gastroenterology outpatient department of a tertiary care teaching hospital. The ROME IV diagnostic criteria were used to identify the FGIDs. Anxiety, depression, coping strategies, social support, and QoL were assessed by the hospital anxiety and depression scale, the coping strategies inventory, the multidimensional scale of perceived social support, and the functional digestive disorders quality-of-life questionnaire, respectively.
ResultsOf the 52 consecutive patients diagnosed with FGIDs, functional dyspepsia (51.92%) and irritable bowel syndrome (40.38%) were the most common. There were no significant associations between sociodemographic variables (age, sex, marital status, socioeconomic status, educational level, employment, occupation, dietary pattern) and QoL scores (all p values >0.05). Duration and social support were not significantly associated with QoL (all p values >0.05). In contrast, psychological variables, such as disengagement coping (r=–0.344, p=0.012), depression (r=–0.600, p=0.000), and anxiety (r=–0.590, p=0.000), were significantly correlated with QoL.
ConclusionsDespite advances in neurogastroenterology, patients continue to be disabled by FGIDs. Psychological factors, especially depression, significantly contribute to poor QoL in those patients and should be addressed in a holistic, multidisciplinary way. The biopsychosocial framework, as it applies to FGIDs, should lead to the inclusion of psychosocial assessments in the clinical management and research of those disorders.
Los trastornos gastrointestinales funcionales (TGIF) son enfermedades complejas caracterizadas por síntomas gastrointestinales, desprovistos de una patología orgánica subyacente. Son trastornos comunes, crónicos, recurrentes, y discapacitantes, que disminuyen de manera significativa la calidad de vida (CdV). El objetivo del presente estudio transversal analítico fue evaluar la CdV y sus correlatos en pacientes adultos con TGIF.
Materiales y métodosSe realizó un estudio transversal, observacional, basado en hospital, en el departamento de gastroenterología ambulatoria en un hospital universitario de tercer nivel. Se utilizaron los criterios de diagnóstico de ROMA IV para identificar los TGIF. La ansiedad, depresión, estrategias de afrontamiento, apoyo social y CdV fueron evaluados con el índice de ansiedad y depresión en hospital, el inventario de estrategias de afrontamiento, el índice multidimensional del apoyo social percibido y el cuestionario de calidad de vida en trastornos digestivos funcionales, respectivamente.
ResultadosDe los 52 pacientes consecutivos diagnosticados con TGIF, la dispepsia funcional (51.92%) y el síndrome de intestino irritable (40.38%) fueron los más comunes. No existieron asociaciones significativas entre las variables sociodemográficas (edad, sexo, estado civil, nivel socioeconómico, nivel educativo, empleo, ocupación, patrón alimenticio) y las puntuaciones de CdV (todos los valores de p>.05). La duración y el apoyo social no estuvieron significativamente asociados con la CdV (todos los valores de p>.05). Por otro lado, las variables psicológicas, como el afrontamiento de distanciamiento (r = –0.344, p=.012), la depresión (r = –0.600, p=.000), y la ansiedad (r = –0.590, p=.000), estuvieron significativamente asociados con la CdV.
ConclusionesA pesar de los avances en la neurogastroenterología, los pacientes continúan siendo afectados por los TGIF. Los factores psicológicos, en especial la depresión, contribuyen de manera significativa a una mala CdV en dichos pacientes. Esto debe ser abordado de manera holística y multidisciplinaria. El marco biopsicosocial, en la manera en que es aplicable a los TGIF, debe llevar a la inclusión de evaluaciones psicosociales en el manejo clínico e investigación de dichos trastornos.
Functional gastrointestinal disorders (FGIDs), or disorders of the gut–brain interaction, represent a continuum of motility disorders that are diagnosed in the absence of structural gastrointestinal pathology. They are believed to be caused by multifactorial pathophysiology, such as psychosocial stress, genetics, diet, neuro-hormonal influences, immune-mediated mechanisms, and low-grade infections of the gastrointestinal tract1.
The ROME foundation has been pioneering education and research on FGIDs. It is an independent international organization of researchers and clinicians, whose aim is to improve the lives of people with FGIDs2. The ROME classification of FGIDs (currently ROME IV) is based on the symptoms associated with a particular anatomic gastrointestinal site, and they are broadly classified into esophageal, gastroduodenal, bowel, gallbladder, sphincter of Oddi, and anorectal disorders.
FGIDs impact nearly all spheres of those patients’ biopsychosocial milieu3. Their chronic course, fluctuating symptoms, absence of specific diagnostic biomarkers, taboos related to bowel control, inconvenience in socializing, dietary restrictions (either self-imposed or indicated by the physician), direct and indirect economic costs, psychological stress, and poor awareness (even among clinicians), all contribute to the poor quality of life (QoL) of its sufferers.
The psychosocial determinants of QoL in FGIDs have not received their due importance, despite evidence suggesting that they impact every aspect of the disease process4. Significant among the social factors are educational level, employment, economic status, and social support5,6. Coping mechanisms, levels of stress, comorbid depression, and anxiety are prominent among the psychological factors5,6. Thus, a holistic understanding of FGIDs would be incomplete, without an analysis of its biopsychosocial determinants and its impact on QoL.
Although FGIDs are common and disabling, there is a paucity of studies that have explored QoL and its determinants in that population. Such studies are limited to focusing on selected FGIDs (irritable bowel syndrome [IBS]7, functional dyspepsia8), are restricted to the pediatric population9, have relied on clinical diagnosis or a questionnaire-based symptom survey10 (as opposed to a structured criteria-based diagnosis), or have explored only a few psychosocial variables11. Despite those limitations, evidence from international research suggests that psychosocial factors significantly impact QoL in FGIDs3.
There is little research conducted on the impact of FGIDs on QoL in patients on the Indian subcontinent12,13. In addition, it is solely focused on functional dyspepsia and IBS or is limited to studying the prevalence and clinical features of FGIDs14–16. The present study is an effort to address that knowledge gap.
The aims of our research were to a) estimate QoL related to FGIDs and b) determine the sociodemographic, psychological (anxiety, depression, coping styles), and social (social support) correlates of QoL in Indian adults with FGIDs.
Materials and methodsThe present cross-sectional study was conducted at the outpatient gastrointestinal department of a medical college teaching hospital in Sikkim, after being approved by the Institutional Ethics Committee. Patients were recruited over a 3-month period.
Inclusion criteria: all the consecutive patients over 18 years of age, seen at the gastroenterology clinic.
Exclusion criteria: refusal to provide consent for participating in the study, undergoing treatment for a psychiatric illness, and having previously received treatment for FGIDs.
The following questionnaires were applied:
- •
A sociodemographic questionnaire to assess age, sex, educational level, marital status, socioeconomic status, occupation, and dietary pattern (vegetarian, mixed diet).
- •
The ROME IV diagnostic questionnaire (R4DQ): an algorithm-based diagnostic tool that incorporates a specific clinical interview, clinical findings, and investigations to generate an FGID diagnosis based on the ROME IV diagnostic criteria.17 The adult version of the R4DQ that was used for the present study required 25−35min to administer and has acceptable sensitivity17. The specificity of the questionnaire is 97.1% for IBS, 93.3% for functional dyspepsia, and 93.6% for functional constipation18. The questionnaire responses were entered into an algorithm that dictated the relevant physical examination and investigations to be carried out to generate an FGID diagnosis.
- •
The Coping Strategies Inventory-short form (CSI-SF): a 16-item scale that assesses coping strategies across 2 dimensions: engagement vs disengagement19. An engagement strategy involves taking actions to directly confront problems, which is associated with good adaptive tolerance. A disengagement strategy means that individuals seek to avoid problems, which can produce long-term problems. The scale has been successfully tested in 9 languages in 13 countries and has excellent reliability and validity20.
- •
The Hospital Anxiety and Depression (HAD) scale: a widely used instrument to assess anxiety and depression in non-psychiatric medical patients in general hospital settings.21 It consists of 14 items divided into 2 subscales; one for anxiety (7 items) and one for depression (7 items), in which the patient rates each item on a 4-point Likert scale. Higher scores are indicative of greater psychopathology. The scale possesses acceptable validity and reliability, as reported in the literature21.
- •
The Multidimensional Scale of Perceived Social Support (MSPSS): a widely used measure to evaluate the perceived adequacy of social support22. Twelve items assess the support from friends, family, and significant others, rated on a 7-point Likert scale ranging from “very strongly disagree” to “very strongly agree”. The total scores range from 12 to 84, with high scores indicative of greater social support. The scale possesses high internal consistency (α=0.88), stability, and construct validity22.
- •
The Functional Digestive Disorders Quality of Life Questionnaire (FDDQL): a disorder-specific scale that measures aspects of life affected by FGIDs, including daily activities (8 items), discomfort (9 items), sleep (3 items), diet (6 items), anxiety (5 items), coping with the disease (6 items), perceived control over disease (3 items), and impact of stress (3 items), on a 5-point Likert scale23. The raw scores are transformed into a range from 0 (poor QoL) to 100 (good QoL). The global score is the mean of all the domain scores, except the impact of stress. The FDDQL has excellent reliability (Cronbach’s alpha 0.94) and validity24.
The data were analyzed using MINITAB 17 statistical software25. The descriptive statistics of mean, standard deviation, and percentages were used to describe the distribution of the variables. The Student’s t-test and ANOVA were utilized to find significant differences in QoL scores in the categorical variables. Correlation statistics were used to assess the association between the continuous variables and QoL scores. A multiple regression analysis was utilized to quantify the relative contribution of predictor variables to the QoL in FGIDs.
Ethical considerationsWritten statements of informed consent were obtained from all the participants. The study complies with the 2017 revised National Ethical Guidelines for Biomedical and Health Research Involving Human Participants of the Indian Council of Medical Research. The study was approved by the Ethics Committee of the Sikkim Manipal Institute of Medical Sciences. This article contains no personal information or identifiers of research participants.
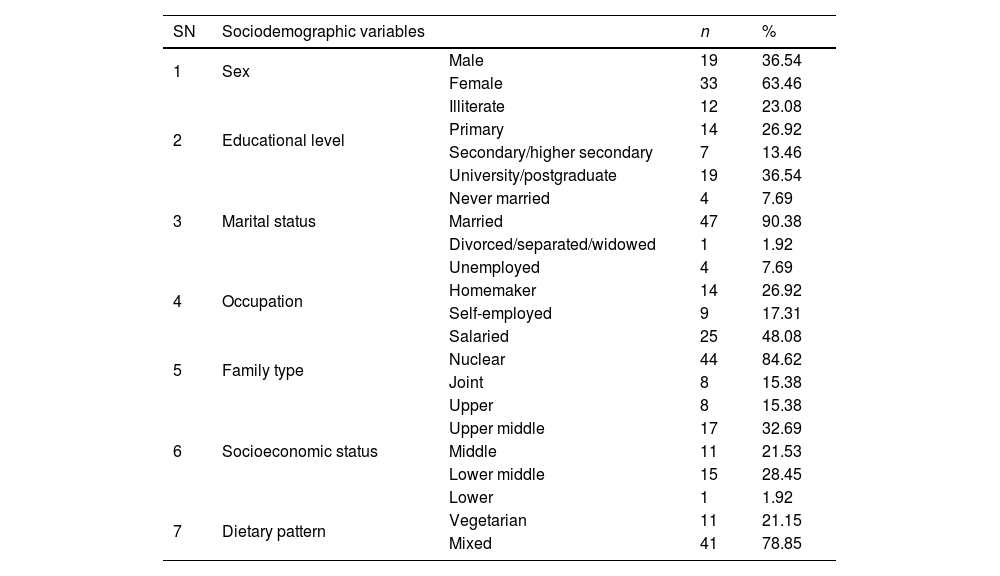
ResultsA total of 52 consecutive adult FGID patients met the inclusion and exclusion criteria of the study. Table 1 illustrates the distribution of the sociodemographic characteristics of the sample. The mean age of the patients was 40.56 years (SD 12.41). Patients suffered from FGIDs for a mean duration of 24.92 months (SD 26.69).
Distribution of the sociodemographic variables of FGID patients (n=52).
| SN | Sociodemographic variables | n | % | |
|---|---|---|---|---|
| 1 | Sex | Male | 19 | 36.54 |
| Female | 33 | 63.46 | ||
| 2 | Educational level | Illiterate | 12 | 23.08 |
| Primary | 14 | 26.92 | ||
| Secondary/higher secondary | 7 | 13.46 | ||
| University/postgraduate | 19 | 36.54 | ||
| 3 | Marital status | Never married | 4 | 7.69 |
| Married | 47 | 90.38 | ||
| Divorced/separated/widowed | 1 | 1.92 | ||
| 4 | Occupation | Unemployed | 4 | 7.69 |
| Homemaker | 14 | 26.92 | ||
| Self-employed | 9 | 17.31 | ||
| Salaried | 25 | 48.08 | ||
| 5 | Family type | Nuclear | 44 | 84.62 |
| Joint | 8 | 15.38 | ||
| 6 | Socioeconomic status | Upper | 8 | 15.38 |
| Upper middle | 17 | 32.69 | ||
| Middle | 11 | 21.53 | ||
| Lower middle | 15 | 28.45 | ||
| Lower | 1 | 1.92 | ||
| 7 | Dietary pattern | Vegetarian | 11 | 21.15 |
| Mixed | 41 | 78.85 |
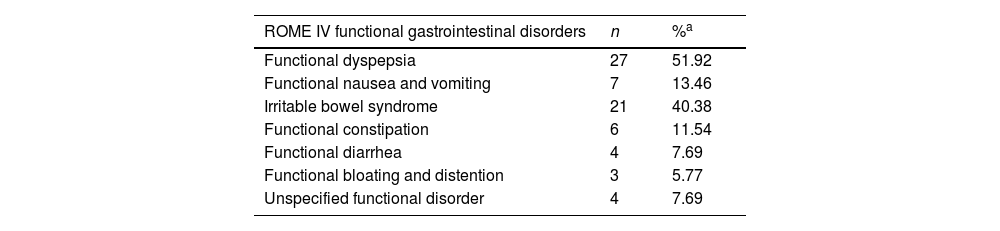
Table 2 shows the distribution of the FGIDs in the sample. Functional dyspepsia was the most prevalent (51.92%, n=27), followed by IBS (40.38%, n=21). For the IBS patients, based on predominant bowel habit, 7 had IBS-constipation, 6 had IBS-diarrhea, 4 had IBS-mixed, and 4 had IBS-unspecified disease. A total of 38.5% patients had more than one FGID. The most common co-occurrence was between functional dyspepsia and IBS (n=9), followed by functional dyspepsia and functional nausea/vomiting (n=3).
Distribution of functional gastrointestinal disorders in the sample.
| ROME IV functional gastrointestinal disorders | n | %a |
|---|---|---|
| Functional dyspepsia | 27 | 51.92 |
| Functional nausea and vomiting | 7 | 13.46 |
| Irritable bowel syndrome | 21 | 40.38 |
| Functional constipation | 6 | 11.54 |
| Functional diarrhea | 4 | 7.69 |
| Functional bloating and distention | 3 | 5.77 |
| Unspecified functional disorder | 4 | 7.69 |
The mean score on the Multidimensional Scale of Perceived Social Support was 4.67 (SD 0.60). On the Coping Strategies Inventory, an engagement strategy (mean 13, SD 1.90) was used more than a disengagement style (mean 11.65, SD 2.08) of coping. On the Hospital Anxiety and Depression scale, the mean depression subscale score was 5.06 (SD 4.58) and the anxiety subscale score was 7.12 (SD 4.92).
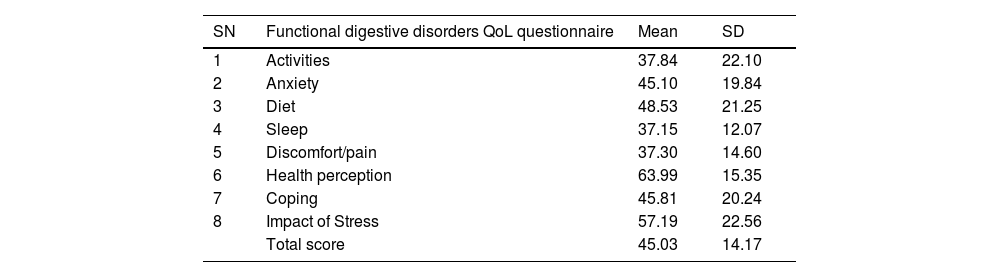
Table 3 shows the distribution of QoL scores, as measured by the FDDQL scale. The mean global QoL score was 45.03 (SD 14.17). A higher QoL was observed in the domains of health perception, followed by the impact of stress and the impact of diet. The poorest scores were seen in the domains of sleep, followed by discomfort/pain, and daily activities, in that order.
Distribution of QoL scores of the sample.
| SN | Functional digestive disorders QoL questionnaire | Mean | SD |
|---|---|---|---|
| 1 | Activities | 37.84 | 22.10 |
| 2 | Anxiety | 45.10 | 19.84 |
| 3 | Diet | 48.53 | 21.25 |
| 4 | Sleep | 37.15 | 12.07 |
| 5 | Discomfort/pain | 37.30 | 14.60 |
| 6 | Health perception | 63.99 | 15.35 |
| 7 | Coping | 45.81 | 20.24 |
| 8 | Impact of Stress | 57.19 | 22.56 |
| Total score | 45.03 | 14.17 |
There were no significant differences in total QoL scores between the various categorical sociodemographic variables (Student’s t-test and ANOVA test p values >0.05). Similarly, age (r = –0.143, p value 0.31) and duration of illness (r = –0.223, p value 0.11) were not significantly correlated with global QoL scores.
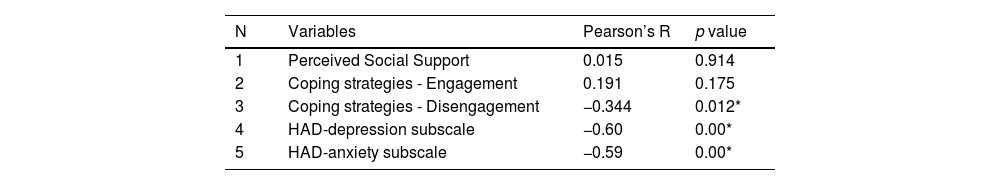
Table 4 shows the correlation between psychosocial variables and global QoL scores. There was a significant negative correlation between global QoL and the disengagement coping style (r = –0.344, p value 0.01), depression (r = –0.60, p value 0.00), and anxiety (r = –0.59, p value 0.00).
Correlation between the total QoL scores and psychosocial variables.
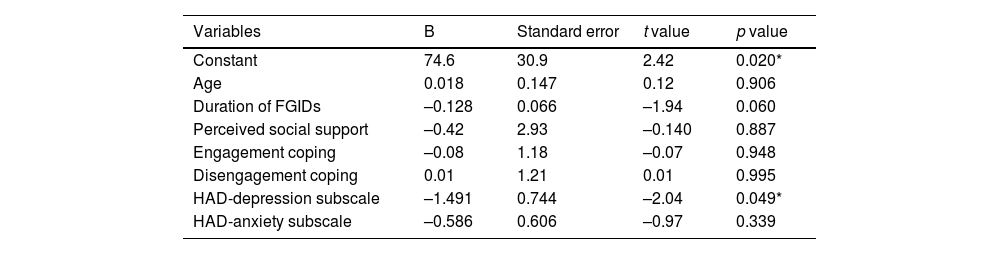
Table 5 shows the results of the multiple regression analysis carried out using a fit regression model. Using the FDDQL global score as the response variable, and using age, FGID duration, perceived social support, coping strategies, depression, and the HAD anxiety subscale scores as the predictor variables, we simultaneously quantified the relative contribution of those variables to the QoL in patients with FGIDs.
Multiple regression analysis of the total FDDQoL versus the sociodemographic, clinical, and psychosocial variables.
| Variables | B | Standard error | t value | p value |
|---|---|---|---|---|
| Constant | 74.6 | 30.9 | 2.42 | 0.020* |
| Age | 0.018 | 0.147 | 0.12 | 0.906 |
| Duration of FGIDs | –0.128 | 0.066 | –1.94 | 0.060 |
| Perceived social support | –0.42 | 2.93 | –0.140 | 0.887 |
| Engagement coping | –0.08 | 1.18 | –0.07 | 0.948 |
| Disengagement coping | 0.01 | 1.21 | 0.01 | 0.995 |
| HAD-depression subscale | –1.491 | 0.744 | –2.04 | 0.049* |
| HAD-anxiety subscale | –0.586 | 0.606 | –0.97 | 0.339 |
Regression model summary: S=11.735, R-sq=44.38%, R-sq (adj)=35.53%.
Regression Equation: FDDQL global score=74.6+0.018 Age – 0.1280 Duration of FGID – 0.42 Social support – 0.08 Engagement coping + 0.01 Disengagement coping – 1.491 HAD depression subscale – 0.586 HAD anxiety subscale.
Results of the analysis demonstrated that those variables predicted 44.38% (R-squared [adjusted]=35.53%) variance in QoL. Of those variables, only depression (T = –2.04, p value 0.049) significantly predicted QoL in patients with FGIDs.
DiscussionThe present study assessed FGIDs across the spectrum of the ROME diagnostic categories, including functional dyspepsia (n=27), functional nausea/vomiting (n=7), IBS (n=21), functional constipation (n=6), functional diarrhea (n=4), and functional bloating (n=3). We used the R4DQ algorithm for the standardized diagnosis of FGIDs. Though most previous researchers have employed the ROME criteria for the diagnosis of FGIDs, the exclusion of organic etiologies was left to the judgment of the clinician. While this may be well-accepted in clinical practice, medical research has to be more specific. The R4DQ is an algorithm based on the ROME IV criteria, which specifies the investigation to be performed, according to patient complaints, to arrive at a specific FGID diagnosis. The use of the R4DQ leaves very little room for speculation on the diagnostic reliability of the ROME criteria across varied clinical settings17.
The central aim of our study was to estimate the QoL of patients with FGIDs. The instrument chosen for that purpose was the functional digestive disorders quality-of-life questionnaire (FDDQL). Though most researchers in this area have used generic measures to assess QoL, such as the SF-36 and the WHOQoL-BREF, we chose a disease-specific measure to assess QoL in FGIDs. Disease-specific QOL measures tend to determine specific elements of the illness and have been shown to be more sensitive to subtle changes than the generic instruments that measure QoL26. Said responsiveness is critical in clinical situations for assessing treatment impact.
None of the baseline social and demographic variables, such as sex, educational level, marital status, sociodemographic status, occupation, family type, and dietary pattern, were significantly associated with QoL scores in the sample. Only a handful of studies have investigated differences between sexes in QoL in FGIDs27, reaching inconclusive results due to variations in methodology and the scales employed. For example, in a study on 251 females and 92 males with IBS, Simren et al. reported that women with IBS reported a lower health-related quality of life (HRQoL) score, compared with men28. However, the measures used as a proxy for QoL were symptom severity, the impact of fatigue, anxiety, depression, and psychological well-being. On the other hand, Lee et al. reported no sex-related differences in IBS29. There are no research data on the contribution of other demographic variables on QoL in FGIDs.
Of the psychosocial variables, we found a nonsignificant positive correlation between perceived social support and QoL scores. There is a dearth of studies, especially in the Asian context, on the moderating effects of social support on FGIDs. Patients with functional disorders perceive their social support to be less helpful than they actually are30. This is due to the stigma and shame associated with the term “functional” as the diagnostic label. The health anxiety and neuroticism usually found in those patients skew their perception and they interpret symptoms as life-threatening. In such a scenario, the existing social support and reassurance from caregivers play an important role in mitigating those fears and allaying anxiety.30 Recent clinical guidelines thus emphasize the support of caregivers in providing optimal reassurance, minimizing stigma, avoiding labelling, reducing isolation, and engaging positively with patients31.
An engagement style of coping showed a nonsignificant positive correlation with QoL scores, whereas a disengagement coping style showed a significant negative correlation. That was not surprising, given the knowledge of the benefits of coping with illness and stressful life events32. However, not all coping strategies are equally beneficial. Coping, though intended to master, tolerate, and/or minimize stress, depends upon the activities or strategies employed in addressing that goal. Said distinction is important because strategies focused on confronting or addressing the situation (engagement-focused coping) are more beneficial or adaptive in the long term. In contrast, strategies that are aimed to avoid or divert attention from the problem, reducing the immediate impact of the situation or emotion, have been shown to be unhelpful or deleterious. Thus, by categorizing coping styles into engagement versus disengagement, the present study was able to distinguish which coping style impacted QoL in patients with FGIDs.
Levels of both depression and anxiety displayed a highly significant negative correlation with QoL in FGIDs. Comorbid emotional disorders have been commonly reported in FGIDs. Affective symptoms can be both a perpetuating or predisposing risk factor for FGIDs and can influence treatment outcomes by negatively impacting the doctor-patient relationship, treatment adherence, healthcare seeking, and poor satisfaction with overall care33. Those problems are magnified due to the large overlap between depression and anxiety with FGIDs, as demonstrated by Zamani et al., in their 2019 meta-analysis34. Given the prevalence and impact of depression and anxiety on various aspects of FGIDs, it is not surprising that they affect QoL. In a review of clinical predictors of QoL in FGIDs, Chang et al. reported that depression and anxiety were one of the strongest QoL predictors in FGIDs3.
Using regression analysis (multivariate), we wanted to simultaneously quantify the relative contribution of the biopsychosocial variables to the QoL of patients with FGIDs. The results showed that those variables (age, duration of illness, perceived social support, coping strategies, depression, and anxiety) predicted a 44.38% variance in the QoL scores. In other words, in any given patient with a FGID, those variables can explain approximately 45% of the variance in QoL. Of the study variables, only depression significantly predicted the QoL in the sample. Similar observations were made by Tung et al., who found that only depression (and not sociodemographic and other clinical factors) was correlated with QoL in IBS patients35.
Thus, our argument that psychosocial factors, especially depression, should be routinely assessed in all patients presenting with functional symptoms of the gastrointestinal tract, was further strengthened. A holistic biopsychosocial approach that includes contributions from the psychiatric and social services will go a long way in improving the disability of patients suffering from FGIDs.
The strengths of our study were that a) we used the latest version of the ROME IV criteria to assess FGIDs, b) we used the algorithm-based R4DQ, along with the clinical evaluation and investigations to diagnose FGIDs, as opposed to a solely questionnaire-based study, c) we assessed a range of FGIDs, instead of limiting the diagnosis to IBS or functional dyspepsia, and d) we used a disease-specific QoL-rating instrument (FDDQL) to improve responsiveness and validity, as opposed to a generic scale (WHOQOL-BREF, SF-36).
Our study is not without limitations. A sample size of 52 patients is small, in comparison to other studies. The study setting (gastroenterology department) could have led to bias, by excluding certain FGID diagnoses, such as globus, which is primarily seen at the ENT department. The assessment of psychopathology was limited to depression and anxiety. Other forms of psychopathology, such as substance abuse, psychosis, bipolar disorders, and anxiety spectrum disorders, could have been assessed. The temptation to perform statistical sub-analyses of QoL scores of individual FGIDs was resisted because data mining to yield further interesting results would only have reduced the quality of the findings, given the sample size of our analysis.
The present study is a modest attempt to explore QoL and its determinants in FGIDs in Indian patients. It is a still unexplored area that has the potential to advance our knowledge in determining the factors that directly impact the QoL of patients with FGIDs. Such studies need to be first conducted in clinical settings to accurately capture FGIDs, without being limited by small sample sizes. More research is needed on FGIDs other than IBS and functional dyspepsia. The personality factors involved in and predispositions to neuroticism and health anxiety need to be investigated as potential moderators of QoL in FGIDs, and the role of those psychosocial factors in community samples needs to be assessed. Lastly, effective interventions to target those psychosocial determinants need to be conducted and replicated in Indian settings, immensely benefiting the patients that suffer from disabling FGIDs.
Financial disclosureThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
Please cite this article as: Sundas A, Sampath H, Lamtha SC, Soohinda G, Dutt S. Correlatos psicosociales de calidad de vida en trastornos gastrointestinales funcionales. Rev Gastroenterol Méx. 2022. https://doi.org/10.1016/j.rgmx.2022.04.006