Colonoscopy is a very frequently used diagnostic technique that has a good safety profile, but it is not exempt from complications, the most well-known of which are bleeding and perforation. However, there are other less common complications, such as splenic rupture, that have elevated morbidity and mortality.
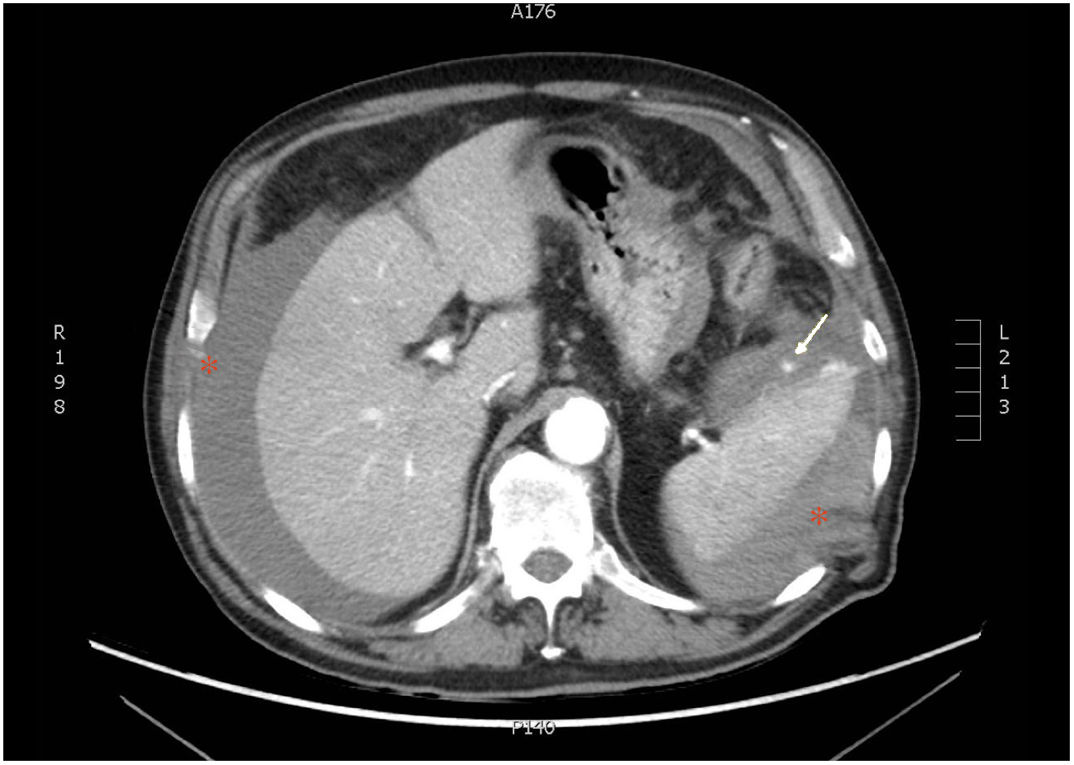
A 77-year-old man had a history of GOLD III chronic obstructive pulmonary disease, lung adenocarcinoma with no current evidence of recurrence, atrial flutter (anticoagulation with edoxaban), prostatectomy due to adenocarcinoma, cholecystectomy, and right inguinal hernioplasty. He sought medical attention for diarrhea, asthenia, and weight loss of several months of progression. Upon admission, oral anticoagulation was suspended and substituted with enoxaparin (60 mg/12 h). Diagnostic colonoscopy was performed, with the patient under deep sedation with propofol. There was no technical difficulty or immediate complications, and the only finding was diverticulosis. No pressure was applied on the left upper quadrant of the abdomen. Twelve hours after the procedure, the patient presented with low blood pressure, tachycardia, and generalized abdominal pain that was poorly controlled with opioids. The pain was described as progressively worsening over several hours. Emergency laboratory tests showed anemia of 8.4 g/dl (previously 12.9 g/dl) and an abdominal x-ray ruled out perforation. Emergency abdominal CT scan was carried out (Fig. 1) that identified splenic rupture with extravasation of the active contrast medium, a large peri-splenic hematoma, and moderate hemoperitoneum, corresponding to a grade V splenic injury, according to the American Association for the Surgery of Trauma (AAST). Despite intensive fluid therapy, the hemodynamic instability persisted, and so emergency splenectomy was performed.
Splenic rupture following colonoscopy is a rare, but potentially serious, complication, with 100 cases described and an estimated incidence of 1 out of every 100,000 procedures.1 Among the apparently associated risk factors are female sex, advanced age, a history of abdominal/pelvic surgery, and anticoagulant/antiplatelet treatment.2 Its etiology is not fully understood, but 3 possible mechanisms have been postulated: direct trauma to the spleen; traction on the splenocolic ligament; or traction on splenocolic adhesions secondary to inflammation or previous surgery.3,4 It usually manifests as abdominal pain in the left hypochondrium, with or without Kehr’s sign (pain radiating to the left shoulder), anemia, and hemodynamic instability.5 The role of deep sedation, which is increasingly used and could mask or delay the appearance of pain, is not clear. When splenic rupture is suspected, the study of choice is contrast-enhanced abdominal CT, albeit abdominal ultrasound can also be useful.
Treatment is dependent on the clinical situation of the patient and the grade of splenic injury. In hemodynamically stable patients, initial conservative management with fluid therapy, blood transfusion, and antibiotics can be attempted. In nonresponding patients and those that present with grade I-IV injuries on the AAST scale, with no previous splenic pathology, splenic artery embolization is an effective therapeutic option. Splenectomy is reserved for cases of active bleeding or persistent hemodynamic instability.6
Despite its low incidence, splenic rupture has elevated morbidity and mortality, making the early suspicion of the complication essential.
Ethical considerationsNo experiments on animals or humans were conducted in the present work and the protocols of our work center were followed in relation to the publication of patient data. Anonymity of patient data was preserved and given that no personal data that could identify the patient were published, informed consent was not necessary for the publication of the present case.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Rodríguez Prida J, Izquierdo Romero M, Álvarez Oltra G, López Caleya JF, Ramírez Baum CE. Rotura esplénica tras colonoscopia, una complicación poco conocida. Revista de Gastroenterología de México. 2021;86:322–323.