Milk is a liquid food that possesses an important quantity of highly bioavailable macronutrients. In addition, it is readily accessible, as well as relatively inexpensive. Given that the knowledge of physicians about nutrition and food composition is deficient, in general, many of the dietary interventions recommended in diverse clinical settings lack a scientific basis. The aim of the present review was to produce a technical opinion that serves as a frame of reference to best sustain recommendations for consuming milk and dairy products as daily nutrition in the adult and older adult. The effects of milk and dairy products during the pediatric stage are not addressed in the present work. The Asociación Mexicana de Gastroenterología and the Asociación Mexicana de Gerontología y Geriatría jointly discussed and analyzed topics dealing with the legal designation of milk, the classification and nutritional profile of cow's milk, its nutritional characteristics, its consumption in the adult, intolerance to cow's milk, and associations of milk consumption with digestive tract alterations and other conditions. Finally, certain aspects of milk consumption in the older adult and its relation to overall health are briefly discussed.
La leche es un alimento que tiene una importante cantidad de macronutrimentos de gran biodisponibilidad, accesible y de relativo bajo costo. El conocimiento de los médicos en general sobre nutrición y composición de los alimentos es deficiente por lo que muchas de las intervenciones dietéticas que tradicionalmente recomendamos en diversos escenarios clínicos carecen de sustento científico. El objetivo de esta revisión fue generar una opinión técnica que sirva como marco de referencia para sustentar de mejor forma la recomendación sobre el consumo de leche y productos lácteos en la nutrición diaria de adultos y adultos mayores. Los efectos de la leche y productos lácteos durante la etapa pediátrica salen del contexto del presente trabajo. La Asociación Mexicana de Gastroenterología y la Asociación Mexicana de Gerontología y Geriatría comentaron y analizaron de forma conjunta temas acerca de la denominación legal de la leche, clasificación y perfil nutrimental de la leche de vaca, sus características nutrimentales, su consumo en el adulto, intolerancia a la leche de vaca, asociaciones entre el consumo de leche y alteraciones del aparato digestivo y otras condiciones; finalmente, se mencionan de forma breve algunos aspectos sobre el consumo de leche en el adulto mayor y su relación con la salud.
The implementation of an appropriate diet is part of the integral treatment of digestive disorders. The majority of patients with gastrointestinal diseases associate their symptoms with dietary elements and they often seek nutritional advice as part of their medical consultation.1–3 Patients frequently restrict or add foods to their diet based on personal perceptions and preferences.4,5 In general, the knowledge physicians have about nutrition and food composition is deficient6 and many of the dietary interventions traditionally recommended in diverse clinical settings lack a scientific basis.7,8 One of the most frequent recommendations in daily clinical practice is to restrict the consumption of milk.9 Milk is a staple that contains an important quantity of highly bioavailable nutrients and is a readily accessible, relatively inexpensive food. Dairy products, especially milk, yogurt, and cheese, are the main sources of calcium and high biological value proteins in the diet of industrialized countries. A diet without dairy products complicates reaching the daily recommended intake of some of those elements. For example, inadequate calcium consumption has consistently been identified in large groups of the population, despite consensus recommendations to increase its ingestion.10 Furthermore, there have been important changes in recent years in the tendency to consume milk and dairy products, especially in certain population groups.11,12
In July 2018, the Asociación Mexicana de Gastroenterología and the Asociación Mexicana de Gerontología y Geriatría summoned a multidisciplinary group of 25 specialists to review and discuss the scientific evidence on milk and dairy product consumption in relation to digestive and overall health in the adult and older adult. They evaluated the evidence, formulated questions about the current state of the designated theme and discussed and answered them in mutual agreement.
The aim of the present review was to produce a technical opinion to serve as a frame of reference for supporting the recommendation of milk and milk product consumption in the daily nutrition of the adult and older adult. Milk and dairy products as food during the pediatric stage of development were not addressed.
MethodThree group coordinators were named (LU, IO, and RV) that performed a search of the PubMed database utilizing the keywords “milk”, “dairy consumption”, “dairy products”, “dairy intake”, “milk consumption”, “lactose”, “lactose intolerance”, “casomorphins”, “digestive system”, “digestive diseases”, “diet”, “nutrition”, “treatment”, “therapy”, “prevention”, “management”, “review”, “guidelines”, “consensus” and “metanalysis”, and their Spanish equivalents. The search included all articles in English and Spanish published within the time frame of July 1990 to July 2018. Preference was given to consensuses, guidelines, systematic reviews, and meta-analyses, but not exclusively. Complementary online and manual searches for all publications up to July 2018 that the coordinators considered relevant were also conducted. The bibliography of the selected citations was made available to the working group for consultation throughout the entire process.
Once the review was completed, twenty-five questions on different themes were formulated. They were discussed and answered at a face-to-face meeting that took place from July 19 to 21, 2018, in Santiago de Querétaro, Mexico. The final results of said review are described below.
The legal designation of milk and the classification and nutritional profile of cow's milkAccording to the NOM-243-SSA1-2010, the official Mexican standard, milk is designated as the natural secretion from the mammary glands of healthy cows or any other animal species, excluding colostrum.13 On average, the composition of bovine milk is water (87%), lactose (4-5%), fats (3-4%), proteins (3%; around 32g/L), minerals (0.8%), and vitamins (0.1%).14
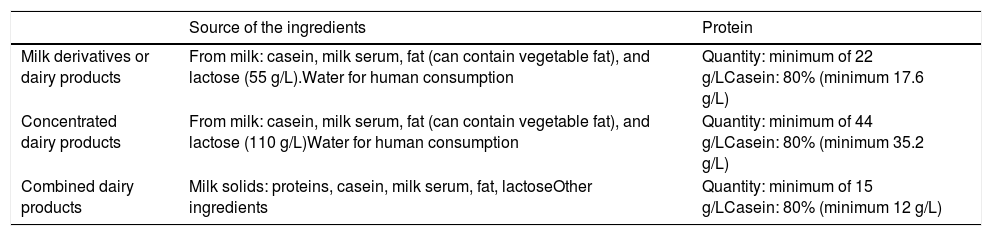
The following terms should be differentiated to avoid confusion: milk derivative or dairy product, combined dairy product, and milk formula. Table 1 shows the characteristics of milk derivatives or dairy products and those of combined dairy products, according to the designations established in the NOM-183-SCFI-2012.15 Milk formula refers to the formulas used in infancy, whether formulas for breastfeeding infants or substitutions for breast milk, follow-on formulas, and formulas for breastfeeding infants with special nutritional needs.16 Specialized documents state the characteristics of the different types of “formulas”, but their description and analysis are beyond the scope of the present document.
Characteristics of milk derivatives/dairy products, concentrated dairy products, and combined dairy products.
| Source of the ingredients | Protein | |
|---|---|---|
| Milk derivatives or dairy products | From milk: casein, milk serum, fat (can contain vegetable fat), and lactose (55 g/L).Water for human consumption | Quantity: minimum of 22 g/LCasein: 80% (minimum 17.6 g/L) |
| Concentrated dairy products | From milk: casein, milk serum, fat (can contain vegetable fat), and lactose (110 g/L)Water for human consumption | Quantity: minimum of 44 g/LCasein: 80% (minimum 35.2 g/L) |
| Combined dairy products | Milk solids: proteins, casein, milk serum, fat, lactoseOther ingredients | Quantity: minimum of 15 g/LCasein: 80% (minimum 12 g/L) |
The classification of milk for human consumption considers the following four features: a) the type of fat it contains (whole milk, semi-skimmed milk, skimmed milk); b) the primary process applied (rehydrated, reconstituted, delactosed); c) the secondary process applied (pasteurized, ultrapasteurized, ultrafiltered, evaporated, condensed, sweetened, dehydrated or powdered, concentrated; and d) modification of the original flavor (if flavoring is added or not). In relation to the first point, whole milk is that which has at least 30g/L of butyric fatty acid, semi-skimmed milk has at least 6g/L, but a maximum of 28g/L, and skimmed milk has a maximum of 5g/L.
Based on the above, the following different commercial designations are described in the NOM155-SCFI-2012:17
- •
Pasteurized milk: that which has undergone the process of pasteurization, whether standardized or not, to meet the NOM specifications, with respect to the content of lactose, fats, total solids, casein, and other ingredients.
- •
Ultrapasteurized milk: that which has undergone the process of ultrapasteurization, whether standardized or not, to meet the specifications described.
- •
Ultrafiltered milk: milk that is obtained from the skimming phase, separated, microfiltered, and pasteurized. Ultrapasteurized cream may then be added or not. The use of aseptic packaging and containers protects the product from the reoccurrence of infection and reduces any physicochemical or organoleptic modification to a minimum.
- •
Evaporated milk: milk that, through the partial elimination of its water content, results in a determined concentration of non-fat and non-butyric acid solids, whether standardized or not, to meet the specifications described.
- •
Sweetened condensed milk: milk that has been obtained through the evaporation of its water content by reduced pressure, to which sucrose and/or dextrose or some other natural sweetener has been added, until reaching a determined concentration of butyric acid and total solids, and then adjusted to the specifications described.
- •
Powdered milk or dehydrated milk: that which has undergone a dehydration process, whether standardized or not, to meet the specifications described.
- •
Concentrated milk: milk that is obtained through the partial removal of its water content, whether by ultrafiltration, inverse osmosis, or the addition of milk products until reaching the desired concentration, to meet the specifications described.
- •
Rehydrated milk: milk that has been obtained through the addition of water (fit for human use and consumption or purified) to the powdered milk and standardized with butyric acid in any of its forms, in the quantities necessary for meeting the specifications described.
- •
Reconstituted milk: made from powdered skimmed milk or from milk ingredients, such as casein, butyric acid, and milk serum, and from water fit for human use and consumption, with a minimum content of 30g per liter of milk protein and 80% casein in relation to total protein, in the quantities necessary for adjusting the product to meet the composition and flavor specifications of the milk described.
- •
Delactosed milk: that which has undergone a process of lactose degradation by lactase to meet the specifications described.
- •
Flavored milk: any of the milk designations included in the present Mexican official standard to which other ingredients have been added, such as natural or artificial flavoring, sweeteners, or coloring, and that contains at least 85% of milk that is fit for human consumption, to meet the specifications described.
The characteristics and specifications of those milks can be looked up in the NOM 155-SCFI-2012.17
Nutritional characteristics of cow's milkCow's milk (CM) is an excellent source of high biological value protein. In fact, it is often considered the best source of protein in relation to the essential amino acids and protein digestibility.15 The protein fraction is divided into serum proteins, which account for close to 20%, and caseins, which account for close to 80%. Both are considered to have high biological value. In addition to their nutritional role, milk proteins and several bioactive peptides resulting from enzyme hydrolysis have multiple biologic roles that can confer protective action on human health. The primary biologic actions include improving the absorption of other nutrients, as well as antibacterial, antithrombotic, opioid, and immunomodulating actions.15,18–20
The serum protein fraction includes alpha lactalbumin, beta lactoglobulin, albumin, immunoglobulins, lactoferrin, lactoperoxidase, protease-peptone, lysozyme, and transferrin.21 Beta lactoglobulin is an important retinol carrier and has fatty acid fixation action and antioxidant capacity, whereas lactoferrin is important for iron absorption, with an antioxidant and anticarcinogenic effect.20,22 Lactoferrin, together with beta lactoglobulin and alpha lactalbumin, have shown tumor development suppression.23 Caseins are calcium and phosphorus carriers.15 Additionally, bioactive peptides are beneficial for human health due to their antioxidant, immunomodulating, and cytomodulating effects, as well as their antithrombotic and antihypertensive action.24–27 Some peptides that resemble beta-casomorphins have actions similar to those of opioids, possessing analgesic and tranquilizing properties on the central nervous system.28,29
CM contains saturated (70%) and unsaturated (30%) fats.15 Conjugated linoleic acid, which corresponds to a group of isomers derived from linoleic acid that resulted from biohydrogenation by the rumen microbiota, has cardioprotective, immunomodulating, anticarcinogenic, and hypolipidemic effects.30,31
Milk is a good source of calcium, phosphorus, magnesium, zinc, and selenium, as well as of the liposoluble vitamins A, D, and E and the insoluble vitamin C and B complex (thiamin and especially riboflavin). Liposoluble vitamin concentration in CM depends on the fat concentration. Thus, their quantities can be lower in semi-skimmed milk and skimmed milk, which is why some countries add vitamins A and D to those milks. 15
Whether some type of milk should be consumed throughout the life cycle was not the aim of the present technical position, but the working group concluded that exclusive maternal breast milk is the best food for infants the first 6 months of extrauterine life and should be promoted at least during the first two years of life.32–34
Beyond the breastfeeding stage, the regulatory framework never addresses the question of whether there is any type of milk that should be consumed, and so a recommendation cannot be given. The requirements are individual, based on genetic expression, possible diseases, and special needs. Whole milk is currently recommended during childhood and adolescence, as long as no overweight is present, and it is one of a variety of foods in a well-balanced diet. For adults, the recommendation is semi-skimmed or skimmed milk.32
Cow milk consumption in the adultMilk is the only food designed by nature to specifically cover the nutritional requirements of infant mammals. The composition of CM, the most widely consumed in the Western world (with the exception of the Middle Eastern countries), is very different from human breast milk, which has a higher lactose content and a lower protein content. In particular, it has a higher proportion of caseins than lactalbumins and there is a great variation in the calcium:phosphorus ratio and the content of other inorganic nutrients and vitamins. Nevertheless, given its nutritional richness, CM, although perhaps not indispensable (because no one food is), offers many advantages. From a culinary perspective, it is an extremely versatile food that can be transformed into products with very different characteristics. They add variety to the diet (cheeses, yogurt, sour cream, sweet cream, butter) and are easier to conserve than milk itself. The average consumption of CM in Mexico (regardless of age group) is moderate. Figures from 2003 to the present range from 318.5 to 367.2mL per person per day. In 2017, consumption per capita was 349.3mL, in other words, a little under one and a half cups per day.35–37
There are no apparent nutritional consequences associated with the null or low consumption of CM, as long as there is a varied and balanced diet. Nevertheless, given the nutritional characteristics it possesses, including CM and dairy products within the daily diet is recommendable. The only two situations in which CM should not be consumed are in cases of cow's milk protein allergy38 and hypolactasia.39 Cow's milk protein allergy is not addressed in the present document and information on it can be found in specific documents.
Intolerance to cow's milkLactose is the principal disaccharide in milk. It is not absorbed in its natural state, but must be hydrolyzed through the effect of lactase, an enzyme produced by enterocytes and that is expressed in the brush border. Hypolactasia, the scientific term for lactase non-persistence, causes the incomplete digestion of lactose and its consequent intact arrival at the colon, where it is fermented by intestinal bacteria that produce hydrogen, methane, carbon dioxide, and short-chain fatty acids.40 Deficient Lactose maldigestion (LMd) symptoms are bloating, abdominal pain, borborygmi, and excessive gas production and they are frequently and erroneously attributed to irritable bowel syndrome (IBS),41 albeit the two entities can coexist.
The terms that should be used to classify persons that are intolerant to milk are of particular relevance.42
- a)
Intolerance is a subjective parameter corresponding to the presence of symptoms that an individual associates with the ingestion of dairy products, and for lack of a biomarker, is evaluated through structured questionnaires.42 It may or may not be due to deficient lactose absorption. Affected persons complain of bloating and abdominal discomfort, borborygmi, and flatulence after ingesting milk or its derivatives. Persons with very little lactase production present with diarrhea secondary to the osmotic effect of unmetabolized lactose.
- b)
Lactase non-persistence (hypolactasia) indicates a lower quantity of lactase in the brush border of the enterocytes. It is a genetic characteristic and should be objectively demonstrated by measuring the enzyme activity in biopsies of the small bowel mucosa.43
- c)
Maldigestion, mistakenly called malabsorption or deficient absorption, is the inability of the digestive tract to digest a certain quantity of lactose and tends to indirectly reflect lactase non-persistence. It can be primary, as in congenital lactase deficiency, which is an extremely rare condition affecting neonates, or secondary, as the consequence of different diseases that cause atrophy of the small bowel villi.44
The frequency of lactose intolerance (LIn) and of LMd in Mexico has been studied in different ways. Initial trials that utilized pharmacologic doses of lactose of 50g reported very high figures of LMd (around 80%) that were notably lower (30%-40%) when physiologic loads between 12-15g were administered.45 On the other hand, according to the Food and Agriculture Organization (FAO), Mexico is a country whose milk consumption is suboptimal.46 It is tempting to think that said discrepancy is due to limited dairy product consumption because of LIn, which is common in the Mexican population. However, that was not demonstrated in a population study that included 926 subjects born in three different regions of the country (the Northeast, the Center, and the South), which according to the researchers, represented different social and economic capacities and were areas that previously had shown distinct milk consumption.47 Unlike other studies, that analysis utilized whole milk or hydrolyzed milk to evaluate the capacity of lactose digestion, which was measured through the hydrogen breath test. Milk consumption was slightly lower in the sites with a greater prevalence of deficient lactose absorption (the Center and the South) and was lower overall in the rural population. LIn was similar in the urban and rural populations and only affected ingestion when classified as significant, in other words, at 7%, which would affect around 8 million Mexicans. Other authors have demonstrated an inverse relation between hypolactasia and lower dairy product ingestion.48
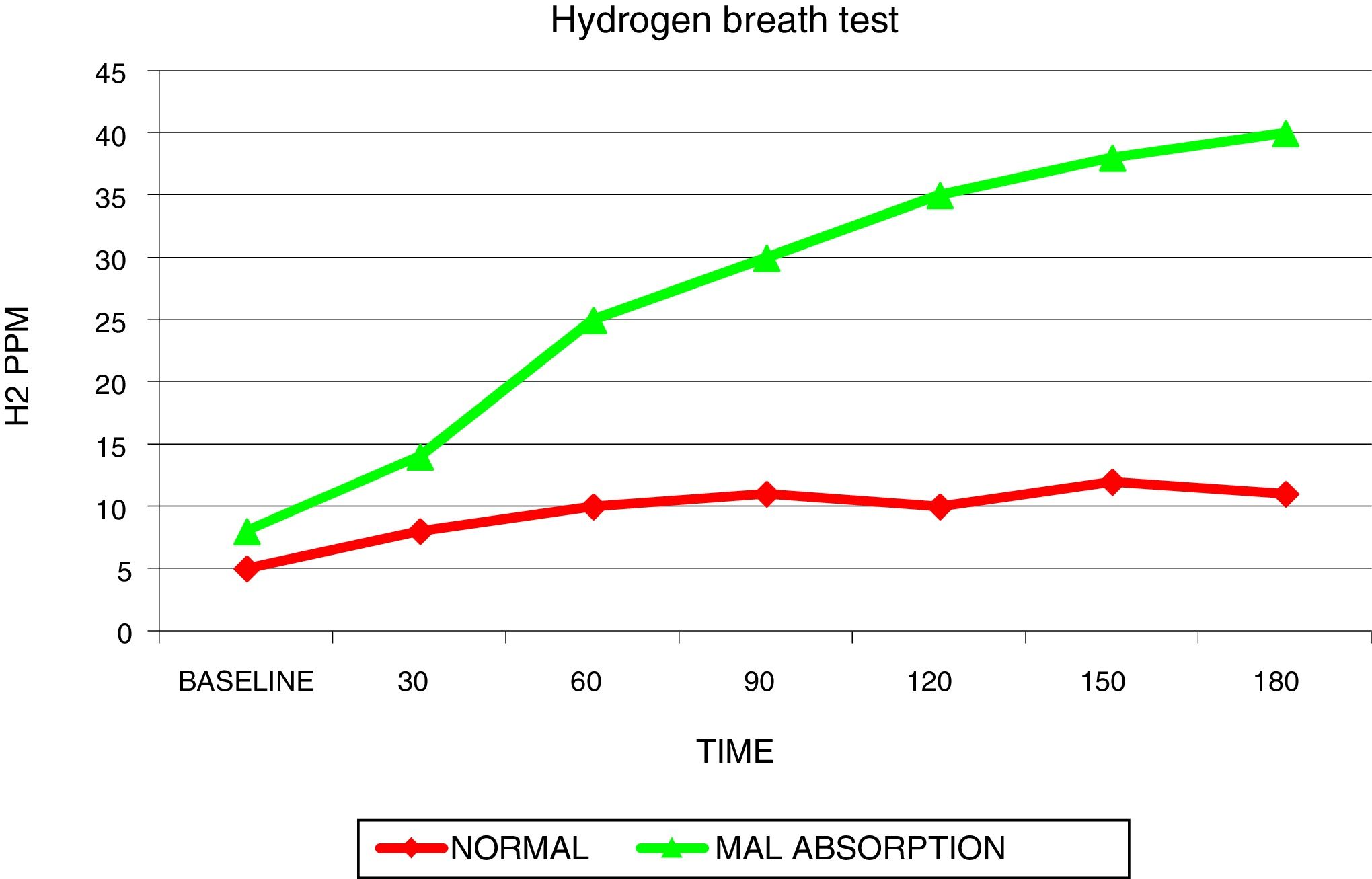
LIn is determined through tests that utilize challenges with lactose dissolved in 250mL of water or whole milk, measuring the products derived from lactase digestion, such as glycemia, galactose concentration in urine, or the parts per million of hydrogen in exhaled breath. The hydrogen breath test, which determines the amount of hydrogen after a load of 25g of lactose, is currently considered the ideal test for lactose maldigestion (fig. 1).49
The production of hydrogen in persons with lactose malabsorption is above 20ppm. The presence of simultaneous symptoms or in the hours following the lactose burden characterizes the patients with intolerance. When there are no symptoms, patients are classified as maldigesters, but tolerant. The majority of subjects with maldigestion can tolerate doses of up to 12g of lactose with no discomfort.
On occasion, there is no relation between intestinal discomfort and the capacity to digest lactose, suggesting that symptom origin could be due to other milk components. In that sense, current evidence points to the fact that some peptides derived from casein digestion are capable of binding to opioid receptors expressed in the digestive tract and could cause several of the symptoms in persons with intolerance to milk.50 Depending on the ancestry of the cows from which the milk is obtained, casein presents in two forms that are differentiated by the presence of proline (Pro) at position 67 in A2 casein or histidine (His) at the same position in casein A1. That characteristic is due to a point mutation (Pro67 to His67) that conditions the differentiating of the two types of casein by the oligopeptides derived from digestive enzyme action, given that Pro is resistant to proteolysis. In addition to that mutation, others in both types of casein in modern European dairy cows have been identified. The majority are of lesser importance, except for that in casein B, which belongs to the casein A1 family and also undergoes the same mutation at position 67, and similar to casein A1 hydrolysis, releases bioactive peptides.51 Casein proteolysis occurs at different sites and some of the peptides released are potentially bioactive, such as casomorphin-7 (CMF-7), an oligopeptide made up of 7 amino acids that is produced by the breaking of the protein chain of casein A1 at position 67 (His). It should be pointed out that casein proteolysis not only releases CMF-7 but also that close to 20 peptide chains of different sizes have been identified and some of them, such as CMF-4, CMF-5, and CMF-6, have an affinity for μ-opioid receptors.52 Research on other effects of casein and CMF on the digestive tract has increased significantly in recent years, especially experiments employing animals exposed to equivalent doses of casein, CMF, and whey protein. Those experiments have shown an important increase in mucus production and in inflammation mediators such as: greater myeloperoxidase activity in the intestinal mucosa, interleukin (IL-4) and immunoglobulin (IgE, IgG, IgG1, IgG2a) elevation, and Toll receptor (TLR-2, TLR-4) overexpression. The administration of casein A1 in rodents has strikingly been demonstrated to increase the production of the dipeptidyl-peptidase 4 (DPP4) enzyme that under normal conditions rapidly degrades the intestinal incretins (the group of hormones that regulate glucose and insulin metabolism) and to decrease antroduodenal motility. That effect is not inhibited with naloxone, indicating that there are other mechanisms of action.53
The clinical impact of milk, with and without casein A1, has been evaluated in three controlled, cross-over, randomized clinical trials. One was conducted on 41 Australian adults that received 750 cc of milk with casein A1 or A2 and the other two were conducted on Chinese adults that consumed 250 cc of milk with casein A1/A2 (40:60) or casein A2/A2. The study design was similar in both populations, with testing periods of 2 weeks separated by a two-week washout period. The three studies showed benefits in the milk without casein A1. Even though the sample size of the Australian study limited the interpretation of the results, they were interesting, in relation to the subgroups. For example, there was a correlation between abdominal pain and stool consistency, evaluated through the Bristol scale, with the consumption of casein A1 that was also present between bloating and abdominal pain and fecal calprotectin levels. The Chinese studies were conclusive upon separating poor lactose digestion (evaluated by testing galactose in urine) from milk intolerance, and showed that symptoms worsened with the consumption of milk with casein A1, in both hypolactasic and normolactasic subjects, bowel transit time was prolonged, and inflammatory markers were expressed.54–56 More studies are needed on humans as to the potentially negative effects that BCM7 could have on different populations and dietary environments before conclusions can be made.53
Associations between milk consumption and the digestive tractGastric emptyingGastric emptying is regulated in relation to the volume, caloric content, osmolarity, and temperature of what is ingested. That process is finely mediated by neuro-hormonal factors that make up a negative feedback mechanism established between the stomach and duodenum.57 For example, studies in murine models have found that gastric emptying is decreased by milk casein, compared with hydrolyzed soy, which increases it.58 In addition, it is very common for dairy products to be ingested together with other compounds, resulting in changes in the regulation of gastric emptying. For example, a study that compared the consumption of black tea with and without milk (50ml of whole milk) and evaluated the plasma concentrations of acetaminophen as an absorption subrogate, as well as areas of transversal sections of the gastric antrum by ultrasound, showed that milk consumption did not affect the absorption dynamic of acetaminophen or the gastric emptying evaluated by areas of transversal section59 and that gastric emptying evaluated after the consumption of 500mL of various liquids, including whole milk, was the same with orange juice as with whole milk (both with the same energy supply). The authors of that study concluded that gastric emptying of those liquids depended more on their energy supply than their nutritional composition.60 In another study, whether the consistency of skimmed milk affected gastric emptying was evaluated in individuals with lactose maldigestion and those without that condition. The milk was thickened with maltodextrin or rice flour, with a similar caloric content. Gastric emptying was measured through a breath test, marking the drinks with 13C. Gastric emptying did not differ according to the viscosity of the milk drink or to the presence of lactose maldigestion.61 Finally, one study evaluated the effect of osmolarity in the consumption of drinks with glucose at different concentrations (150, 300, and 600 mOsm), with lactose (150, 300, 290 mOsm), and with milk alone (283 mOsm) or with chocolate (614 mOsm) in persons with lactose maldigestion, evaluated through a lactose load test and capillary glycemia measurement. Percentages of gastric emptying were quantified 30min after the consumption of the liquids. Gastric emptying was not modified in relation to the presence of deficient or normal lactose digestion, but was affected according to the grade of osmolarity of the liquid consumed (glucose, lactose, or milk).62
With the current evidence, it can be inferred that gastric emptying is not substantially altered by the ingestion of milk per se. However, energy supply, osmolarity, and volume can potentially alter gastric emptying. The addition of sweeteners or other compounds can also modify the baseline parameters of the milk product and influence a change in gastric emptying.
Functional disordersFew studies were found that dealt with knowing the impact of milk consumption on functional gastrointestinal disorders. Clinical pictures are similar between milk intolerance, functional dyspepsia, irritable bowel, and tympanites. Symptoms attributed to the ingestion of milk or lactose in intolerant persons, such as bloating, flatulence, tympanites, colic, diarrhea, nausea, vomiting, heartburn, and regurgitation coincide with those produced by functional gastrointestinal disorders.63,64 There is little information on the relation between functional dyspepsia and milk ingestion. Intolerance to dairy products is not usually considered in the differential diagnosis of dyspepsia. One study on 197 patients diagnosed with functional dyspepsia (Rome III) found adult hypolactasia through a genetic study in 88 patients and they presented with more tympanites/bloating that the 109 patients with lactase persistence (p=0.014). The other symptoms of dyspepsia (proximal abdominal pain, nausea, vomiting, early satiety, and overall grading) were not different between the two groups.65 Given the above, good practice in a country such as Mexico with frequent LIn, would appear to include questioning the patient with possible functional dyspepsia about his or her ingestion of dairy products and its relation to symptoms.
In the case of IBS, there is more awareness among clinicians of the possibility that lactose intolerance can be at least a partial cause of symptoms. A European study recently reported on the search for lactose maldigestion in 51 patients with IBS, through the hydrogen breath test, allergy tests, and psychologic evaluation, and found that 41% of the patients considered themselves lactose intolerant, 47% had a positive hydrogen breath test, and one patient had signs of hypersensitivity to cow's milk measured through IgE. The patients that showed lactose maldigestion presented with more intense symptoms, more hydrogen production, and a higher degree of anxiety, depression, and fatigue. The authors concluded that the capacity to digest lactose and the intensity of IBS symptoms were the most important factors in the clinical picture, albeit mental status influenced symptom perception.66 A recent review on diet and IBS specified that there is solid evidence for decreasing the ingestion of fermentable short-chain carbohydrates, or FODMAPs, in general, but not milk or gluten.67 After abdominal pain, the most frequent symptoms in the Mexican patient are tympanites, bloating, and flatulence. The Mexican IBS Research Group published an epidemiologic study on 1687 patients from different areas of the country that reported bloating in 96% of the patients, tympanites in 86%, and flatulence in 81%.68 Those symptoms were also frequently mentioned by patients that described themselves as lactose intolerant. It has not been definitively clarified whether patients with lactose maldigestion produce more gas if they also present with IBS. But experts do coincide that it is necessary to study lactose digestion in all patients with tympanites or distension that ingest dairy products, whether or not they complain of being intolerant. Of course, suspending dairy products for a few days is a simple way to help arrive at a diagnosis, albeit the hydrogen breath test after the ingestion of 25g of lactose is recommended.69
Acid peptic disease and gastroesophageal reflux diseaseFor the first half of the twentieth century, milk was the cornerstone of treatment for peptic ulcer, even in cases that presented with bleeding, based on the neutralizing effect of milk on acid. However, it was later proven that due to its high content of calcium and proteins, and not its fat content, it significantly increased acid production. The consumption of a 250mL glass of milk was shown to increase acid production by 30%. In addition, unlike healthy persons, those with peptic ulcer are more sensitive to that effect on the parietal cells of the stomach.70 Later studies that compared two groups of patients with ulcers, one on a normal diet and the other on a milk-based diet, reported that the group that did not consume milk had better ulcer cicatrization results confirmed through endoscopic study.71 There is apparently no difference between the different types of milk.72 Based on the above information, patients with ulcers should not drink milk as disease treatment or for relief from the pain or burning sensation caused by ulcers. Nevertheless, as a food, it is an excellent source of calcium and high biological value proteins. Therefore, its consumption as a food is permitted in patients with ulcers, recommending moderation in the consumption of high-fat cheeses, such as Italian soft cheese, cream cheese, and Italian blue cheese, to name a few.73 Patients with acid peptic disease can consume milk in reasonable quantities and as part of a healthy diet. It is an excellent food, albeit not indispensable for adequate nutrition, but there is no problem with its consumption by persons that tolerate it and enjoy drinking it.74
In the case of gastroesophageal reflux disease, there is still not enough evidence to recommend not drinking milk. In some low-quality studies, milk was the food that caused the most reactions in persons with reflux, but a systematic evaluation with very strict requirements did not specifically include milk. Therefore, drinking milk for symptom relief is not recommended, but in patients with gastroesophageal reflux disease that tolerate milk, there is no problem in its consumption as a food. Nevertheless, if drinking milk causes symptoms related to reflux, its consumption should be avoided.75
MicrobiotaThe microbiota can be modulated through dietary changes, prebiotic, probiotic, and antibiotic consumption, and recently through fecal microbiota transplantation. The intestinal microbiota could be considered a biomarker for the consumption of healthy or nonhealthy foods.76 Some evidence is being found regarding milk and dairy product consumption and its effect on the intestinal microbiota, but it is not yet differentiated at the level of strains. Milk and dairy products contain polyunsaturated fatty acids, specifically conjugated linoleic (omega 6) acid, which modulates the production of arachidonic acid, prostacyclins, thromboxanes, cytokines, and acetylcholine, having a beneficial effect on inflammatory bowel diseases. Upon interacting with the microbiota, conjugated linoleic acid favors the growth and adhesion of certain Lactobacillus species and increases the production of short-chain fatty acids (acetic acid, butyric acid, and propionic acid). Those fatty acids are beneficial for the prevention of metabolic disorders and immune tolerance through the regulatory T cells, aiding in the synthesis and oxidation of fatty acids, lipolysis, and particularly, the production of butyrate. They have also been described to have anti-inflammatory properties and contribute to adequate intestinal motility.77–80
Inflammatory bowel diseaseThe role of milk and dairy products in inflammatory bowel disease (IBD) is controversial and has become confusing due to the phenotypic division of the status of hypolactasia in the adult. Milk and dairy products aggravate symptoms in some patients and their physicians recommend a reduced-lactose diet and sometimes with the probably unnecessary restriction of milk and its derivatives.81 In a study whose aim was to evaluate the influence of diet on the course of the disease, there were no significant associations between relapses and the ingestion of vegetables, cereals, milk and dairy products, or fish.82 Another retrospective study reported that persons with IBD consumed a larger amount of animal protein and carbohydrates and a lower quantity of unsaturated fat, dietary fiber, and alcohol, compared with the general population. The results indicated that dietary factors play a role in the disease course.83
Different studies stipulate that there is not enough evidence to eliminate or reduce the consumption of milk and dairy products in persons with IBD. To the contrary, it appears that their consumption can be a protective factor against IBD, specifically for Crohn's disease, but it is not certain if they play the same role in ulcerative colitis.81 The restriction of milk and its derivatives could have an adverse effect on the result and outcome of IBD.
Liver diseasesIn addition to the nutritional supply of milk, especially the milk serum that is derived from the making of cheeses, it has a high content of cysteine, which is one of the main components of the glutathione produced in the liver. Glutathione has a strong antioxidant effect, among its other numerous functions that are beneficial to health, such as detoxification (oxidative stress), defense, and protein synthesis. Milk, specifically the proteins in the serum, could have a certain clinical use, according to a study conducted in Switzerland that described reduced steatosis and stabilization of the lipid profile in a group of women with fatty liver that received milk serum.84
There are many myths in favor of and against the consumption of milk and its derivatives, and liver diseases are no exception. Unfortunately, much of the information is empiric and scientific evidence is scarce. Methodologically weak case reports and studies abound.
In general terms, there are few restrictions on the consumption of milk and dairy products in relation to liver diseases. In fact, daily consumption of milk, cheeses, and yogurt is recommended in nonalcoholic fatty liver disease as part of the so-called Mediterranean diet.85 Fructose, which is added to some dairy products or flavored milks has become associated with hepatic steatosis. However, its conclusive causality has not yet been established, making more studies necessary before making a pronouncement on its use.86,87
Regarding acute hepatitis, patients should have a complete and balanced diet. There are few food restrictions and no sustained evidence on modifications of milk and dairy product ingestion.
There are no restrictions on the consumption of dairy products in compensated cirrhosis of the liver. To the contrary, in cases of hepatic encephalopathy, the use of certain disaccharides, such as lactose, lactulose, and lactitol can be useful in reducing the production and intestinal absorption of ammonia. Type C encephalopathy (episodic, spontaneous, and recurrent) is the best therapeutic indication for the use of those sugars, as recommended in the hepatic encephalopathy clinical guidelines of the Asociación Mexicana de Gastroenterología.88 In acute hepatic encephalopathy, the oral route should be maintained to the extent possible and the pertinence of reducing liquids and sodium should be considered in accordance with the general conditions of each patient. Protein support, preferably of vegetable origin, is also recommended, due to its lower methionine load and higher fiber content that reduce the risk for encephalopathy. In chronic encephalopathy, total liquid and sodium support must also be considered, proteins should predominantly be of vegetable origin, albeit some products of animal origin, such as milk and fresh cheeses, are recommendable.89
In summary, information on the impact of dairy product consumption on liver diseases is scarce and methodologically weak. Nevertheless, milk and its derivatives are consumed with no problems in the majority of cases of acute and chronic hepatopathies.
Associations between milk consumption and other conditionsIn general, there is no evidence supporting the claim that the consumption of cow's milk increases mortality.90 A brief description of the evidence on milk and dairy product ingestion and their association with certain specific conditions follows below.
Cardiovascular diseaseWith respect to the association of milk and dairy product consumption with the risk for cardiovascular disease (CVD), the results of several systematic reviews with meta-analyses show that the consumption of different dairy products is associated with neutral, or even protective, clinical results for the development of CVD.91–93 Another systematic review reported an inverse association between low-fat dairy products and the development of high blood pressure.94 In a prospective study that incorporated three cohorts from the 1986-2010 and 1980-2012 Health Professionals Follow-up Study and Nurses’ Health Study and the 1991-2011 Nurses’ Health Study II, conducted in the United States, and that together include over 5 million persons, the consumption of dairy fat was associated with the risk for CVD. The authors concluded that replacing said fat for vegetable fat and polyunsaturated fatty acids could reduce the risk.95
The consumption of milk and its derivatives is recommended in patients with CVD, specifically in the older adult.96 The recommended dairy products should be skimmed or contain vegetable fat.91,95 The suggested amount for daily consumption takes the recommendation of the DASH diet97 and the Mediterranean diet98 into account. The former recommends between two and three equivalents of low-fat or non-fat dairy products, based on a standard daily dietary intake of 2000 Kcal. The latter recommends two to four equivalents of dairy products per day.
Bone mineral metabolismThe calcium in milk has high bioavailability, similar to that of calcium carbonate, which is easily absorbable.99 Persons with a high consumption of milk and its derivatives have a higher bone mineral content.100 The digestibility of calcium and phosphorous present in milk is high because they are bound to casein. Consequently, milk is an excellent source of calcium for maintaining good bone health in the adult and preventing the bone demineralization that is a cause of osteoporosis and fractures.101
Milk is the primary source of dietary vitamin D in the countries that add it to milk.102 In addition to providing calcium, milk and dairy products also contain proteins, vitamins, and other nutrients, such as phosphorus and potassium, which play and important role in the regulation of bone resorption. There is limited evidence in current studies on the positive effects of milk consumption in adulthood and the risk for fractures in the older adult.103 In a study published in 2014 and derived from two prospective cohorts (nurses and health professionals), the participants, at the beginning of the study, reported their milk consumption during adolescence and were followed for 22 years. The authors concluded that the high milk consumption in adolescence was not associated with a low risk for hip fracture in older adulthood. A marginal positive association was found in males, but disappeared when adjusted by height, which tends to be greater in men.104 Given the above, the evidence, albeit limited, suggests that the ingestion of milk and its derivatives has a positive effect on bone health during adulthood and on the risk for fractures in the older adult.103,105,106
Diabetes, obesity, metabolic syndrome or isolated components in adultsStudies showing that milk proteins have a positive effect on high blood pressure, dyslipidemia, and hyperglycemia and indirectly improve metabolic health, increase lean muscle mass, and reduce the incidence of obesity have increased in the last 20 years.107 Milk serum proteins have an insulinotropic effect, possibly due to the “incretin” effect.108 An increase in the daily ingestion of low-fat products, yogurt, and cheese can contribute to the prevention of type 2 diabetes.109 The daily ingestion of three equivalents of milk reduces the risk for DM and high blood pressure. In 7 studies, milk ingestion was reported to be inversely proportional to the development of CVD and DM.110
In a meta-analysis of prospective cohorts, milk ingestion was found to be associated with a reduced risk for presenting with CVD (RR: 0.90, 95% CI: 0.76-0.83), as well as cerebral vascular events (RR: 0.88, 95% CI: 0.82-0.95), and showed no relation to coronary disease.111
Another systematic review of prospective cohort studies showed an inverse relation between milk and dairy product consumption and the incidence and prevalence of metabolic syndrome (RR: 0.85, 95% CI: 0.73, 0.98).112 In a cross-sectional analysis, elevated milk consumption (mean intake of 77.9g/day) was associated with a low prevalence of metabolic syndrome and hypertriglyceridemia, as well as a decrease in LDL, in 130,420 Korean adults between 40 and 69 years of age.113 Given the above information, there appears to be an inverse association between the incidence of metabolic syndrome and milk and dairy product consumption, suggesting a protective effect of CM and dairy products for its development.
There is information derived from observational studies on a potential protective effect of CM and its derivatives on the development of high blood pressure. However, a study employing the Mendelian randomization method took data from 22 studies with 171,213 participants and 10 prospective studies, for a total of 32 studies and 197,332 participants. The authors found no modification in systolic pressure with the consumption of milk and dairy products. Therefore, at present, there is no evidence of a protective or hazardous effect of CM and its derivatives on high blood pressure.114
Mucus productionThe relation of milk and dairy product consumption to the production of mucus in the respiratory system in geriatric patients has no support, given that the few studies on the topic have low methodological quality and do not take into account respiratory tract comorbidities and smoking.115 In a study conducted on 169 persons with a mean age of 46 years, they were asked what they thought about mucus production and milk ingestion. The participants that thought there was a relation between the two consumed less milk. Of the 169 individuals, 130 agreed to participate in a double-blind, randomized, controlled clinical trial, in which they received milk or a placebo (a soy formula), and acute symptoms within the first 24hours after ingestion were evaluated. There was no difference in the frequency of symptoms between the two groups.116 In some studies, an association has been described between mucus production and CMF-7, which stimulates the production of the secretory glycoprotein, mucin-5AC (MUC5AC), that is expressed in the foveolar epithelium of the stomach and is also present in the respiratory system.117
CancerOne of the most controversial aspects of milk consumption is its relation or not to cancer. In a systematic review and meta-analysis that included 11 population cohort studies and a combined total of 778,929 individuals, the total ingestion of CM and dairy products was not associated with a risk for cancer death (RR: 0.99; 95% CI: 0.92-1.07, p=0.893). That lack of association was also shown in subgroups (separately considering the intake of CM, yogurt, cheese, and butter) in both men and women. There was only an increased risk for prostate cancer with the ingestion of whole milk (RR: 1.50; 95% CI: 1.03–2.17, p=0.032). A dose-response analysis showed that the increase in the ingestion of whole milk increased the risk for prostate cancer death, which could be more related to its fat content than to the milk itself.118
Milk consumption and health in the older adultThere is real evidence on the two main factors that, within the concept of active aging, increase life expectancy, and they are adequate nutrition and physical activity. The consumption of milk and its derivatives as part of the diet has different advantages in the population over 60 years of age. Those foods provide the diet with important diversity and contribute to adequate nutrition. Older adults consume milk and dairy products in a limited manner, in some they are restricted from their diet, and others have eliminated them from their diet, generally because of lactose intolerance. Cow's milk and its derivatives are an inexpensive source of several nutrients that favor the maintenance of an adequate nutritional status: high biological value proteins, vitamins (D, B12, and riboflavin), and minerals (calcium).119 Milk and dairy foods are low-cost, easily accessible, and can be ingested frequently throughout the day in their different presentations.
The nutrients in milk and dairy products contribute to a healthy aging process because they favor cardiovascular, gastrointestinal, immunologic, and metabolic health, as well as bone mineralization and muscle mass. Different studies have shown that people are aware of the health benefits that milk and dairy consumption provide, but a considerable part of the adult population continues to restrict its consumption in a personal attempt to lower lipid or cholesterol levels or because they have difficulty digesting some products, especially cheese.120 It has been shown that adults and the elderly have a lower score for the risk of death and can even have a better LDL-C profile by consuming more low-fat dairy products.121
Milk and its derivatives can play an important role in muscle health and evidence suggests they are also responsible for effects on body composition in the elderly, possibly due to their high content in bioactive compounds, such as the branched-chain amino acids contained in milk serum protein. Through questionnaires on the frequency of consumption of different foods, a cross-sectional study evaluated the association of dairy product ingestion with muscle mass in the past year through dual x-ray absorption study (DXA), muscle strength through manual pressure (dynamometry), and physical performance. The study was conducted on 1456 women from 70 to 85 years. The results showed that women that ingested more milk had a significantly higher mean muscle mass (34.4 ± 0.3 vs. 32.9 ± 0.3kg; p=0.001) and greater appendicular skeletal muscle mass (15.3 ± 0.2 vs. 14.5 ± 0.2kg; p=0.002). There were no important differences in manual pressure strength (20.9 ± 0.2 vs. 20.0± 0.2kg; p=0.02) or in the prevalence of falls within the 3 previous months.122
In another study that evaluated the association between milk and dairy product ingestion and peripheral bone structure and muscle mass in 564 elderly women from 80 to 92 years of age (mean age of 84.7 years), there was a positive association between milk and dairy consumption and appendicular bone mineralization and muscle mass. The ingestion of 2.8 portions/day vs. 0.9 portions/day significantly favored better bone structure in the appendicular skeleton.123
The association between milk and dairy consumption and the incidence of metabolic syndrome has also been studied in the elderly. One study prospectively analyzed 1868 men and women from 55 to 80 years of age that did not present with metabolic syndrome at the beginning of the study. They were followed for 3.2 years and the results showed an incidence of metabolic syndrome in 930 cases, with a hazard ratio (HR) of 0.72 (0.61, 0.86) for low-fat dairy products; 0.73 (0.62, 0.86) for low-fat yogurt; 0.78 (0.66, 0.92) for full fat yogurt; 0.80 (0.67, 0.95) for low-fat milk; and 1.31 (1.10, 1.56) for cheese.124
Another prospective study on 3454 non-diabetic older adults with an approximately 4-year follow-up showed that the total milk and dairy product consumption was associated with a lower risk for developing type 2 DM (HR: 0.68 [95% CI: 0.47-0.98]; p=0.040), mainly with low-fat milk and dairy products (HR: 0.65 [0.45-0.94]), low-fat milk (HR: 0.67 [0.46-0.95]), and yogurt (HR: 0.60 [0.42-0.86]) (p=.002).125
One study evaluated the association of milk and dairy consumption with the risk for fragility, according to the Fried criteria, in adults above 60 years of age that live in a community (n=1,871). The authors found that the subjects that consumed seven or more portions/week of low-fat milk and yogurt had a lower incidence of fragility (OR: 0.52; 95% CI: 0.29-0.90; p=0.03) than those that consumed under one portion/week. Particularly, the individuals that consumed seven or more portions/week of low-fat milk and yogurt had less risk for walking slowly (OR: 0.64, 95% CI: 0.44-0.92, p=0.01) and for losing weight (OR: 0.54, 95% CI: 0.33-0.87, p=0.02). The consumption of seven or more portions/week of whole milk or yogurt (OR: 1.53, 95% CI: 0.90-2.60, p=0.10) or cheese (OR: 0.91, 95% CI: 0.52-1.61; p=0.61) was not associated with the development of fragility.126
Obviously, more research is needed with respect to the increase in low-fat yogurt and milk consumption for the prevention of fragility in the older adult.
Appropriate nutritional information on their consumption is required so that the elderly can become aware of the important value of consuming milk and dairy products and the role they play in a healthy diet.
More conclusive evidence is needed regarding cognitive deterioration and delirium. However, a meta-analysis conducted in Japan found a protective association between milk consumption and dementia. Those authors concluded that more large-scale prospective studies are needed to describe potential dose-response milk ingestion patterns in populations with different characteristics.127
The recommendation of milk consumption in the older adult should be individualized, according to different health/disease conditions. The general recommendation is to consume low-fat, lactose-free milk that is preferably rich in proteins. Technologic advances have made it possible to modify milk and dairy products in lactose-free versions, signifying that lactose intolerance is no longer an impediment to benefitting from their consumption in the geriatric population.128,129
ConclusionsAt present, the scientific evidence supports the consumption of milk and dairy products as part of a balanced diet, which can be beneficial throughout adulthood, including the older adult stage, except in cases of specific medical conditions, such as lactose intolerance or cow's milk protein allergy. Consumed in adequate quantities, cow's milk and its derivatives provide the diet with macronutrients and micronutrients. There is some evidence that milk and dairy consumption could have potentially protective effects for the development of diabetes, overweight/obesity, and cardiovascular disease.
Financial disclosureThe Asociación Mexicana de Gastroenterología A.C. obtained non-conditioned funding for logistic purposes from the Instituto LALA and the Instituto de Bebidas de Coca-Cola de México. The scientific agenda, discussion, and conclusions stated in the present document were autonomous and independently written by the members of the working group.
Conflict of interestRVF: has received funds to attend congresses and has received speaking fees from Nestlé® and Sanofi® and has received speaking fees from Carnot®, BioGaia®, and Nutricare®.
RICS: is a member of the advisory board of Asofarma® and is a speaker for Mayoly-Spindler®, Asofarma®, and Chinoin®.
FMHI: is an advisor for Asofarma® laboratories and a speaker for Asofarma® and Takeda®.
MPMG: since 2004 has been on a committee of the Cámara Nacional de Industriales de la Leche (CANILEC).
Please cite this article as: Uscanga-Domínguez LF, Orozco-García IJ, Vázquez-Frias R, Aceves-Tavares GR, Albrecht-Junnghans RE, Amieva-Balmori M, et al. Posición técnica sobre la leche y derivados lácteos en la salud y en la enfermedad del adulto de la Asociación Mexicana de Gastroenterología y la Asociación Mexicana de Gerontología y Geriatría. Revista de Gastroenterología de México. 2019;84:357–371.