Acute pancreatitis is one of the most common gastrointestinal conditions requiring hospitalization. Even though its presentation during pregnancy is uncommon, it is a medical challenge. Currently, no studies compare the clinical outcomes between pregnant patients with acute pancreatitis and nonpregnant patients with acute pancreatitis. Our aim was to compare the characteristics and clinical outcomes of pregnant and nonpregnant women with acute pancreatitis.
MethodsWe conducted a retrospective study that included all patients admitted to our hospital with acute pancreatitis over a 10-year period. Demographics, general characteristics, and clinical outcomes were evaluated and compared between pregnant and nonpregnant women with acute pancreatitis, at a ratio of 1:5.
ResultsOver 10 years, 27 pregnant patients with acute pancreatitis were treated. Etiology was biliary in 96% and hypertriglyceridemia was the cause in 3.4% (1 patient). The mean patient age was 26.2 years (range 15-36 years). The main cause of acute pancreatitis was biliary disease (96%). Patients in the study group were in their first, second, or third trimester of pregnancy, at 7.4%, 33.3%, and 59.3%, respectively. In the comparison of pregnant versus nonpregnant patients with acute pancreatitis, there were no differences in age, hospital stay (7.37 vs. 10.8, p = 0.814), severity (severe 3.7% vs. 16.7%, p = 0.79), local complications (0% vs. 1.9%, p = 0.476), or mortality (0% vs. 1.9%, p = 0.476).
ConclusionsThe clinical evolution of both groups with biliary acute pancreatitis was similar, with low morbidity and mortality.
La pancreatitis aguda es una de las condiciones gastrointestinales más comunes que requieren hospitalización. Aunque su aparición durante el embarazo es poco común, representa un reto médico. Actualmente no existen estudios que comparen los desenlaces clínicos entre mujeres embarazadas con pancreatitis aguda y pacientes no embarazadas con pancreatitis aguda. Nuestro objetivo fue comparar las características y desenlaces clínicos de las mujeres embarazadas y no embarazadas con pancreatitis aguda.
MétodosRealizamos un estudio retrospectivo que incluyó a todas las pacientes admitidas en nuestro hospital con pancreatitis aguda durante un periodo de 10 años. Se evaluaron y compararon los datos demográficos, las características generales y los desenlaces clínicos entre las mujeres embarazadas y las mujeres no embarazadas con pancreatitis aguda, con una razón de 1:5.
ResultadosSe trató a 27 pacientes embarazadas con pancreatitis aguda en un periodo de 10 años. La etiología fue biliar en 96% de los casos y en 3.4% de los casos la causa fue hipertrigliceridemia (1 paciente). La edad media de las pacientes fue de 26.2 años (rango de 15-36 años). La causa principal de la pancreatitis aguda fue la enfermedad biliar (96%). Las pacientes en el grupo de estudio cursaban su primer, segundo o tercer trimestre del embarazo, con una distribución del 7.4%, 33.3% y 59.3% respectivamente. En la comparación entre pacientes embarazadas y no embarazadas con pancreatitis aguda no existieron diferencias en edad, tiempo de hospitalización (7.37 vs. 10.8, p = 0.814), gravedad (grave, 3.7% vs. 16.7%, p = 0.79), complicaciones locales (0% vs. 1.9%, p = 0.476), o mortalidad (0% vs. 1.9%, p = 0.476).
ConclusionesLa evolución clínica de ambos grupos con pancreatitis biliar aguda fue similar, con baja morbilidad y mortalidad.
Acute pancreatitis (AP) is one of the most common digestive diseases requiring hospitalization in Western countries. In 2012, AP was the third most common gastrointestinal, hepatic, or pancreatic cause of hospitalization, accounting for more than 275,000 admissions with an aggregate cost exceeding $2.6 billion USD in the United States.1 Episodes are primarily mild in 75-85% of patients, with an in-hospital mortality rate of approximately 0.8%. However, 15-25% of patients may develop a severe course, with mortality exceeding 15-25%.2 From a clinical standpoint, there is evidence suggesting that patients at higher risk of developing severe AP (SAP) are obese, older adults, current smokers, alcohol consumers, and those with comorbidities.3 The clinical evolution of AP during pregnancy is not fully understood. Most Western studies report a good prognosis, but Asian studies have demonstrated a poor fetal and maternal outcome. That could be secondary to the etiology of the pancreatitis, given that hypertriglyceridemia is a leading cause of AP in pregnant women in Asia. Only small retrospective studies have addressed the issue, suggesting that pregnancy is not a risk factor for the development of AP.4,5 To the best of our knowledge, this is the first study that compares, with paired-characteristics, the clinical evolution between pregnant and nonpregnant patients presenting with a first episode of biliary AP.
Materials and methodsPatientsA retrospective study was conducted from a prospectively collected database. A search for pregnant patients with AP, encompassing a 10-year period (2004 to 2014), was carried out from the pancreatitis database of the Gastroenterology Department. The demographic data, clinical characteristics, therapeutic interventions, and in-hospital progression were collected from the patients’ clinical records. The relevant clinical history (comorbidities such as high blood pressure, diabetes mellitus, chronic kidney disease), previous episodes of AP, previous cholecystectomy, gestational age in weeks at admission, characteristics of the AP event (severity, local or systemic complications, mortality), hospital stay, laboratory tests (complete blood count, liver function tests, serum amylase and lipase, and blood chemistry [serum creatinine and blood urea nitrogen levels]), imaging studies (magnetic resonance cholangiopancreatography or endoscopic ultrasound) and therapeutic interventions (endoscopic retrograde cholangiopancreatography [ERCP] and/or laparoscopic cholecystectomy) were recorded for each patient.
At our institution, all patients with suspicion of AP are evaluated by a multidisciplinary team, which includes primary care physicians, gastroenterologists, radiologists, and surgeons. We treat an average of 100 cases of AP per year, most of them of biliary etiology, with an overall in-hospital mortality rate of 5%.6 All patients with AP receive standardized management with intravenous analgesia, intravenous hydration, enteral or parenteral nutrition, systemic antibiotics, and ERCP, as deemed necessary.
The present study included all pregnant patients admitted to our hospital that presented with AP. The AP diagnosis was made with 2 of the following criteria: characteristic abdominal pain, serum amylase and/or lipase greater than 3 times the upper limit of normal, and confirmatory findings of AP through imaging studies.7 The pregnant patients with biliary AP were compared with nonpregnant patients with biliary AP, with a 1:5 ratio. We excluded all patients that did not meet the above diagnostic criteria or those with incomplete data.
Statistical analysisThe information was descriptive, and all variables were expressed by means and percentages, as necessary. The Pearson chi-square test was used to compare the categorical variables of both groups. The statistical analysis was performed using the SPSS version 20 program.
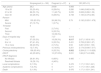
ResultsClinical characteristicsAn average of 4,515 pregnant patients are seen at our hospital yearly. Over a 10-year period, there were 27 pregnant patients diagnosed with AP and their mean age was 24.89 years (range:15 to 36 years). The majority of AP events were of biliary origin (96.6%). Only one patient had pancreatitis due to hypertriglyceridemia (3.4%). Most of the patients presented with AP in the third trimester of pregnancy (59.3%), followed by the second trimester (33.3%), and only 2 patients had AP in their first trimester (7.4%). Sixty-five percent of the patients had previous pregnancies. A total of 59.3% of the pregnant patients with AP had fewer than 7 days of hospitalization, compared with 35.2% of the nonpregnant patients with AP (OR 2.67, 95% CI: 1.165-6.161, p = 0.017) (Table 1).
Clinical characteristics and evolution in nonpregnant and pregnant patients with acute biliary pancreatitis.
| Nonpregnant (n = 162) | Pregnant (n = 27) | p | OR (95% CI) | |
|---|---|---|---|---|
| Age (years) | 26.2 | 24.89 | 0.868 | – |
| 15 to 20 | 33 (20.4%) | 8 (29.6%) | 0.280 | 1.646 (0.662-4.09) |
| 21 to 30 | 86 (53.1%) | 11 (40.7%) | 0.235 | 0.608 (0.266-1.39) |
| Over 30 | 43 (26.5%) | 8 (29.6%) | 0.738 | 1.165 (0.475-2.85) |
| Ranson | ||||
| Mild | 135 (83.3%) | 26 (96.3%) | 0.79 | 0.192 (0.025-1.478) |
| Severe | 27 (16.7%) | 1 (3.7%) | ||
| Trimester | 0 | |||
| First | 2 (7.4%) | – | – | |
| Second | 9 (33.3%) | |||
| Third | 16 (59.3%) | |||
| Days of hospital stay | 10.80 | 7.37 | 0.814 | |
| 1 to 7 | 57 (35.2%) | 16 (59.3%) | 0.017 | 2.67 (1.165-6.161) |
| 8 to 14 | 67 (41.4%) | 9 (33.3%) | 0.431 | 0.709 (0.300-1.67) |
| 15 or more | 38 (23.5%) | 2 (7.4%) | 0.59 | 0.261 (0.59-1.153) |
| Previous cholecystectomy | 12 (7.4%) | 4 (14.8%) | 0.201 | 2.174 (0.646-7.317) |
| Cholecystectomy | 106 (65.4%) | 9 (33.3%) | 0.002 | 0.264 (0.111-0.626) |
| ERCP | 42 (25.92%) | 10 (37.03%) | 0.231 | 1.68 (0.714-3.958) |
| ERCP diagnosis | ||||
| No lithiasis | 26 (61.9%) | 6 (60%) | 0.485 | – |
| Resolved lithiasis | 16 (38.1%) | 4 (40%) | ||
| Local complications | 3 (1.9%) | 0 | 0.476 | 1.17 (1.103-1.241) |
| Systemic complications | 7 (4.3%) | 0 | 0.271 | 1.17 (1.105-1.248) |
| Death | 3 (1.9%) | 0 | 0.476 | 1.17 (1.103-1.241) |
The rate of previous cholecystectomies in the pregnant and nonpregnant patients with AP was 14.8% vs. 7.4%, respectively (OR 2.174, 95% CI: 0.646-7.317, p = 0.201). After clinical resolution of the AP event, 65.5% of nonpregnant patients with AP and 33.3% of the pregnant patients with AP underwent cholecystectomy during the same admission (OR 0.264, 95% CI: 0.111-0.626, p = 0.002). ERCP was performed in 25.92% of the nonpregnant patients with AP, compared with 37.03% of the pregnant patients with AP (OR 1.68, 95% CI: 0.81-4.5 p = 0.231). Choledocholithiasis was diagnosed in 40% of the pregnant patients with AP, compared with 38.1% of the nonpregnant patients with AP. All those cases were successfully treated, with no severe complications.
OutcomesAccording to Ranson’s criteria at 48 h of admission, there was no difference in severity between the 2 groups of patients (OR 0.192, 95% CI: 0.025-1.478, p = 0.476). Mild AP occurred in 26 (96.3%) of the pregnant patients with AP and 153 (83.3%) of the nonpregnant patients with AP. Of the pregnant patients with AP, only one (3.7%) developed severe AP, compared with 27 (16.7%) of the nonpregnant patients with AP (p = 0.79).
The disease course was uneventful in the pregnant patients with AP, whereas 1.9% and 4.3% of the nonpregnant patients developed local and systemic complications, respectively. However, no significant differences were noted between the 2 groups. None of the patients suffered a preterm or cesarean delivery due to AP. Three deaths were documented in the nonpregnant patients with AP (1.9%) and none in the pregnant patients (OR 1.17, 95% CI: 1.03-1.241, p = 0.476).
DiscussionThe present study demonstrated that pregnancy may not predispose to an unfavorable outcome in AP of biliary etiology. To the best of our knowledge, this is the first study comparing the clinical evolution of pregnant and nonpregnant patients with biliary AP. Our study has several strengths. First, the exclusive assessment of biliary AP outcomes in pregnant women is relevant. Second, the matched-pair comparison between pregnant and nonpregnant patients with AP ensured equal distribution of the covariates analyzed. Third, obstetric and prenatal follow-up was carried out at our institution, guaranteeing multidisciplinary patient care.
There are certain discrepancies with results from other studies. For example, Tang et al. reported an overall poor maternal-fetal prognosis. However, their subgroup of patients with biliary etiology showed a favorable clinical evolution similar to the outcomes in our study, suggesting that poor outcomes could be explained by etiology.
On the other hand, our study validates the work by Xu et al., who reported a low overall incidence of AP in pregnancy with low morbidity.8 We have previously reported our experience managing AP, with an overall mortality rate of 5% at our institution.6
There are several limitations to our study. First, a small number of pregnant patients were included in the analysis, which could be a consequence of the low incidence of AP in that population. Second, the study was retrospective, and before 2012 the predictive tool utilized at our hospital to evaluate AP prognosis was Ranson’s criteria. After 2012, we began to use the modified Marshall score to predict severity, according to the revised Atlanta criteria.9 Since the development of Ranson’s criteria, many other multiple-parameter clinical scoring systems have been proposed, but the ideal score has yet to be identified, for multifactorial reasons. A recent study compared existing clinical scoring systems for predicting SAP and showed modest accuracy for all parameters.10
Third, a low number of patients in both groups underwent therapeutic interventions during their hospital stay. There is increasing evidence regarding the role of same-admission cholecystectomy, to prevent future biliary and pancreatic complications.11 Furthermore, there is recent evidence that conservative management of cholelithiasis and its complications during pregnancy is associated with recurrent biliary symptoms and frequent emergency department visits.12 In our population, cholecystectomy was performed twice as much in the nonpregnant patients with AP (65.4%), compared with the pregnant patients (33.3%), which could be secondary to the mild clinical course of the biliary AP. However, ERCP is considered safe during pregnancy and recent guidelines state that laparoscopic cholecystectomy is a safe procedure during any trimester.13
Fourth, no maternal-fetal deaths were documented, and newborns were discharged with no apparent complications. There was no long-term follow-up due to the main outcome of the study. A detailed follow-up could help to identify long-term complications or delayed procedure outcomes.
Finally, we must specify that the etiology of pancreatitis is extremely varied, depending on the population studied. In Western countries, biliary etiology accounts for up to 100% of cases of AP in some studies, whereas hypertriglyceridemia is the cause reported in a large number of Asian patients, which could explain the different clinical outcomes. More studies on pregnant and non-pregnant patients with hypertriglyceridemia-induced AP are needed.
In conclusion, our study showed that the clinical evolution of pregnant and non-pregnant patients with biliary AP was similar, with low morbidity and mortality. The nonpregnant patients had a longer hospital stay and a higher number of cholecystectomies.
Ethical disclosureProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality. The authors declare that no patient data appear in this article.
Finance disclosureNo financial support was received in relation to the present article.
Author contributionsJose A. González-González and Emmanuel I. González-Moreno designed the research, Tamahara González-Campos and Gilberto Herrera-Quiñones performed the research, Omar Borjas Almaguer and Roberto Monreal-Robles analyzed the data, Héctor J. Maldonado-Garza and Diego Garcia-Compeán critically reviewed the manuscript for important intellectual content.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: González-González JA, Herrera-Quiñones G, Borjas-Almaguer OD, Monreal-Robles R, González-Moreno EI, González-Campos T, et al. El impacto del embarazo en el desenlace de pancreatitis biliar aguda. Revista de Gastroenterología de México. 2020;85:416–420.