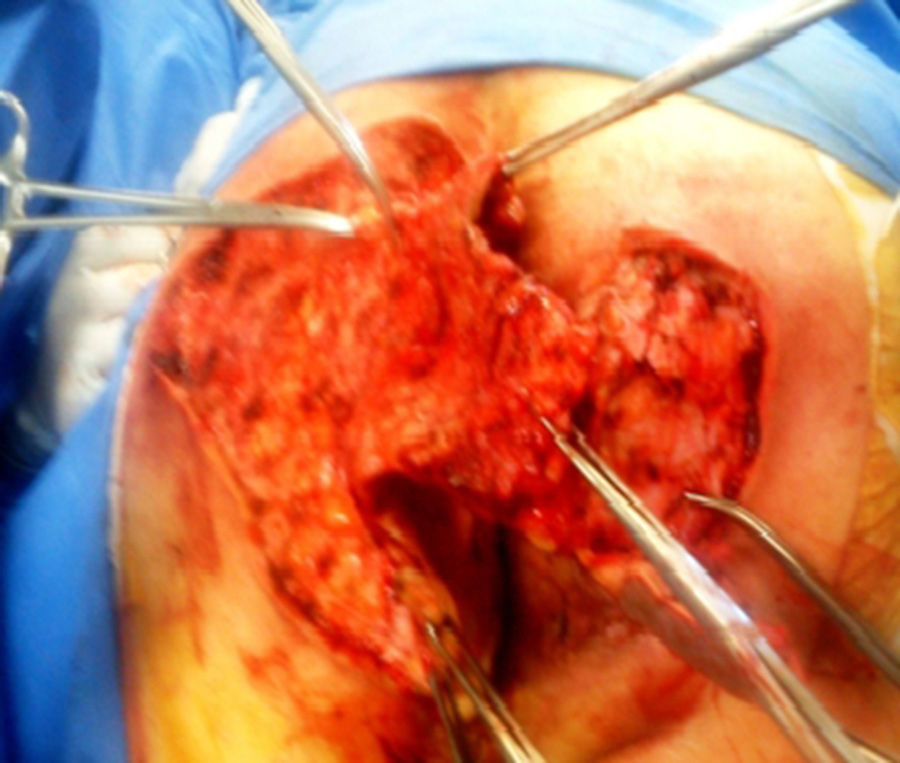
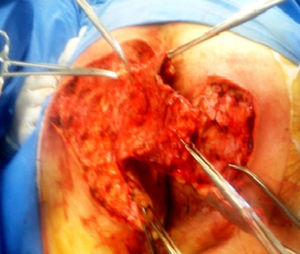
A 64-year-old man had a past history of poorly controlled type 2 diabetes mellitus of 18-year progression, alcoholism, and severe smoking. He presented with an abscess in the left perianal region 10 years prior, with pain, edema, erythema, and spontaneous drainage 8 days later; at present, according to the patient, symptoms are imperceptible but there is a constant scant purulent to serous discharge. Physical examination revealed irregular widespread involvement of the bilateral gluteal, perianal, and scrotal areas, with the presence of subcutaneous nodules, amorphous and irregular scars, dermal abscesses with secondary fibrosis, sinuses and/or ulcers, contracture, and induration of the skin (Fig. 1). No anal duct involvement was identified in the proctologic revision. Laboratory work-up was normal and culture of the purulent matter reported Escherichia coli. Intra-anal ultrasound revealed “fistulous” tracts with no communication with the anal duct. Surgical treatment was radical resection of the complete thickness of all the affected skin with a 2cm margin that extended to the subcutaneous fat, leaving only healthy tissue (Fig. 2). The postoperative period was satisfactory and the patient was released 72h after surgery, with only sitz baths carried out for the secondary wound, and follow-up at 10 months until the definitive cure and release (Figs. 3 and 4) with no recurrence, no infection, and with epithelialization. The histopathologic study reported “hidradenitis suppurativa”.
Verneuil's disease is a rare pathology of unknown etiology. The first case was described in 1839 by Velpeau, but it was not until 1854 that it was clinically identified by Verneuil.1 It is characterized by nodular inflammation and chronic infection of the apocrine glands, “fistulas”, abscesses, and fibrosis located on the scalp, neck, axilla, breast, and the periumbilical, inguinal, perianal, and gluteal regions.2
Its incidence is 1 in every 600 individuals and it is more frequent in men and in adults. It is associated with diabetes mellitus, overweight, smoking, anemia, poor hygiene, hormone disorders, and Cushing's disease.3,4 Symptoms are: a minimum of pain, continuous scant purulent discharge, and edema and erythema in the affected zone; there is no systemic inflammatory data, but the pathology has a negative psychologic and social effect.5 The most frequently isolated microorganisms are: Proteus mirabilis, Staphylococcus aureus, and Escherichia coli.6 Diagnosis is difficult if there is no experience with the disease, and therefore it tends to become chronic and extend from the involved area.7
The concept of hidradenitis suppurativa is not new, but its etiology is unknown,8 and so the following was concluded upon analyzing the present case:
The origin of this pathology comes from a poorly drained abscess2,9 that remains in the subcutaneous zone and extends toward the epithelium, where it converges with the apocrine glands, becoming chronic in a poorly vascularized zone.
Morphologically, the fistulas are paradoxical, superficial, multiple, and they are communicated with each other and irregular, with no common origin or epithelium; they do not reach the status of a classic fistula (defining fistula as an opening or passage that exists from one epithelium to another).
It is a chronic disease with no clinical systemic manifestation, it is not incapacitating, and in some cases is painless,10 due to a high degree of adaptability or of becoming accustomed to it; the loss of anatomy and its consequent physiology results in destroyed or very damaged nociceptors. Another contributing factor is diabetic neuropathy.
Treatment with oral and topical antibiotics (clindamycin, tetracyclines, metronidazole, cephalosporins, rifampicin, etc.) and the purely topical ones (resorcinol, fusidic acid, azelaic acid) is described, all with high recurrences. Systemic corticoids (cyclosporine, azathioprine, methotrexate, alpha TNF inhibitors, including infliximab) provide discreet improvement and transitory results. Antiandrogens (cyproterone acetate, finasteride, ethinyl estradiol) have very limited results. Patients worsen with zinc salts. Oral retinoids (isotretinoin, acitretin) provide minimum improvement. Radiotherapy, cryotherapy, photodynamic therapy, botulinum toxin, and radiofrequency have all shown very poor results.2,8,9
Pharmacologic treatment is not an option, due to the diminished vascularity of the area and the continuous chronic inflammation process. Therefore, the only choice left is surgery and the technique is: radical resection with disease-free borders and closure by secondary intention.
The gluteal and perianal area, in particular, has late cicatrization. Nevertheless, secondary wound closure is an excellent alternative even in immunosuppressed patients. Deformation is acceptable and there is no limitation in the function of the anatomic region in question. Sitz baths as a therapeutic measure make it possible to avoid a second surgical procedure, such as flap rotation or graft application, given that it is an extensive bloody or denuded area that is very painful, with a high risk for infection or recurrence and prolonged cicatrization.
Sitz baths provide adequate pain and inflammation control, reducing analgesic consumption, and cicatrization is improved with granulated tissue, preventing infection and recurrence. And it is a low-cost outpatient procedure.
In conclusion, the presentation of this case (there is no protocol treatment to date) is a “watershed” for the basis of new studies that define the disease pathophysiology, treatment, and its cure.
Verneuil's disease is of great interest to the medical community and merits interdisciplinary, comprehensive, and long-term management.
Financial disclosureNo financial support was received in relation to this work.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: García-Sánchez MA, Santillan-Arellano EG. Enfermedad de Verneuil. Presentación de un caso y revisión de la literatura. Revista de Gastroenterología de México. 2015;80:225–227.