Introduction
Wilson's disease (WD) is an autosomal recessive disorder of copper metabolism resulting in abnormal accumulation of copper in many organs due to mutations in the gene coding for the ATP7B copper transporter.1 The liver and brain are the most affected, and clinical manifestations can occur in many ways, but the development of liver failure with its complications and/or incapacitating neurological manifestations is almost universal.1,2
The gene defect is located in the long arm of the chromosome 13, and to date, molecular genetic analyses have revealed approximately 300 different mutations.3 Treatment of this disabling disease has traditionally being based on the use of copper-chelating agents, striving for restoration of normal copper metabolism, and thus achieving normal levels of free serum copper and urine excretion.1 Liver transplantation (LT) has been recognized as the ultimate therapeutic approach, mainly in patients with end-stage liver disease, and less often as an adjunct for the treatment of unremitting neurological disease (with controlled hepatic disease or in its absence).4 In the present study, our aim is to describe the clinical outcome of a Mexican cohort of patients with WD, not within any research scenario, but under standard conditions of a daily basis clinical practice, in a third level attention institution. Special attention was placed upon patients in whom LT was performed as a result of deteriorating neurological manifestations.
Material and methods
Patients with WD were identified from a database containing all diagnoses on discharge at the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, by using the code E83.0 (which stands for disorders of copper metabolism) of the International Classification of Diseases (ICD-10). This is a nation-wide tertiary referral hospital in care of adult patients, most of whom have mestizo origin, and a low- to medium-class socioeconomic status. All cases diagnosed between 1980 and 2002 were reviewed by members of the Department of Gastroenterology (S.Z.G., J.G.L., J.R.T., and A.T.) to confirm the diagnosis using the Leipzig diagnostic criteria (score ≥ 4).5 Eventually, all patients with confirmed WD were referred to consultation to the Liver Transplantation Clinic (M.O.M) for further follow-up and study of family members. The latter was performed on first-degree relatives of the proband, and it comprised a complete clinical examination, liver function tests, and measurement of ceruloplasmin and urinary copper excretion. Therefore, the design of our study had both a retrospective and a prospective component, although gathering of information was retrolective (retrospective study / retrolective cohort). Data pertaining to diagnosis, copper metabolism, laboratory and imaging profiles, treatment, clinical outcome and genetic analysis (direct DNA sequencing of the ATP7B gene) were obtained from medical charts. To assess changes on liver functional status, the original MELD score (or PELD when indicated) was calculated, and development or progression of complications related to hepatic failure and portal hypertension (ascites, variceal bleeding, spontaneous bacterial peritonitis, hepatorenal syndrome, hepatic encephalopathy) was evaluated. Magnetic resonance imaging (MRI) of the brain was performed in all patients with neuropsychiatric manifestations, before orthotopic LT and 6 months after this procedure. Follow-up and outcome were noticed. All studied patients were Mexicans, defined as individuals born in Mexico, whose parents and grandparents identified themselves as Mexican mestizos. The study was approved by the local Institutional Board for Human Research and designed according to international guidelines.
Results
We were able to confirm the diagnosis of WD in 11 patients (8 males and 3 females), out of a total of 24 potential patients identified. All of the nonconfirmed patients did not fulfill the diagnostic work-up for WD and were lost to follow-up.
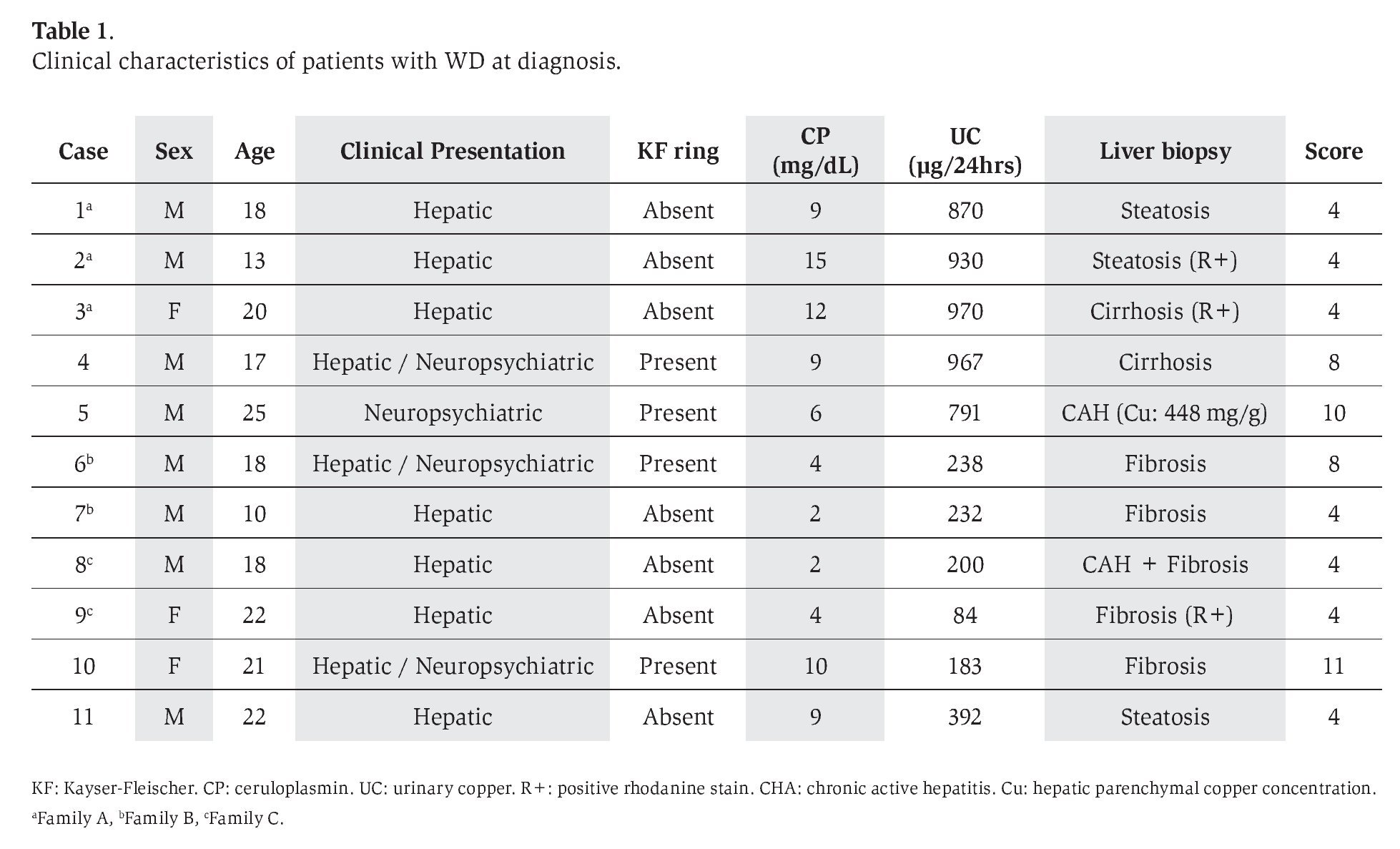
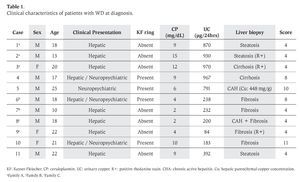
Clinical criteria of WD are shown on Table 1. All patients had a Leipzig score 3 4 points, consistent with a highly likely diagnosis.5 Median age at diagnosis for all patients was 18 years (range 10-25). Patients 3, 6 and 8 were probands for family screening, disclosing 4 affected members; therefore, the disease was familial in 7 patients (family A=3, family B=2, family C=2) and sporadic in 4. Hepatic manifestations were present in 10 patients and had started at a median age of 17 years (range 10-22). These included steatosis or abnormal liver echogenicity on ultrasound and/ or elevated aminotransferases in 6, jaundice, ascites and splenomegaly in 3, and hepatomegaly in 2. On the other hand, neuropsychiatric phenomena were observed in 4 patients (in 3 cases these were associated with hepatic manifestations), and started at a median age of 18.5 years (range 16-24). These were characterized by tremor, dysarthria, gait disturbances, choreic movements and emotional lability. All the latter patients had Kayser-Fleischer rings on slit-lamp examination, and one of them also suffered from sunflower cataracts. A median diagnostic delay of 1 year (maximum 3 years) was noticed for both patients with hepatic or neuropsychiatric manifestations. Only 2 patients developed generalized symptoms such as fatigue and malaise. There were no cases with hemolysis or fulminant presentation.
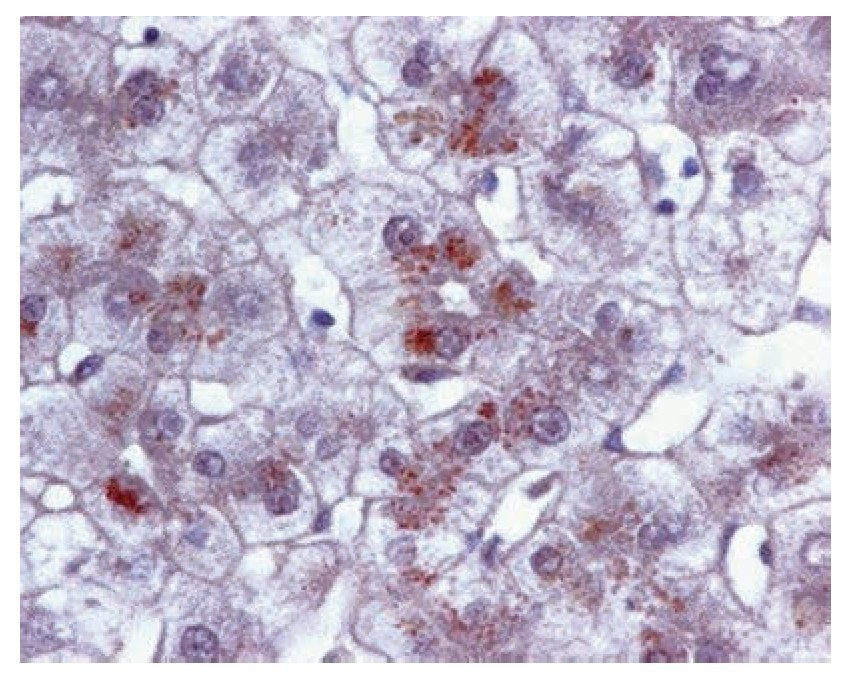
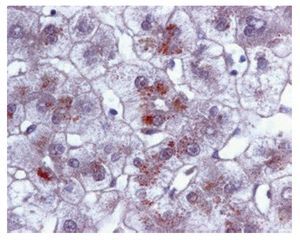
Liver biopsy with histochemical copper staining (rhodanine) was performed in all cases, although positive granules in hepatocytes were evidenced in 3. Quantification of hepatic copper content was carried out only in one patient with the sporadic form (case 5, Table 1, Figure 1); as was also the case for genetic analysis, disclosing homozygocity for the haplotype H1069Q (Case 10). The reason to perform hepatic copper quantification and genetic analysis, each in only one patient, is because these are expensive techniques with very scarce availability in our center.
Figure 1. Liver biopsy of case 5 showing quantification of hepatic copper content
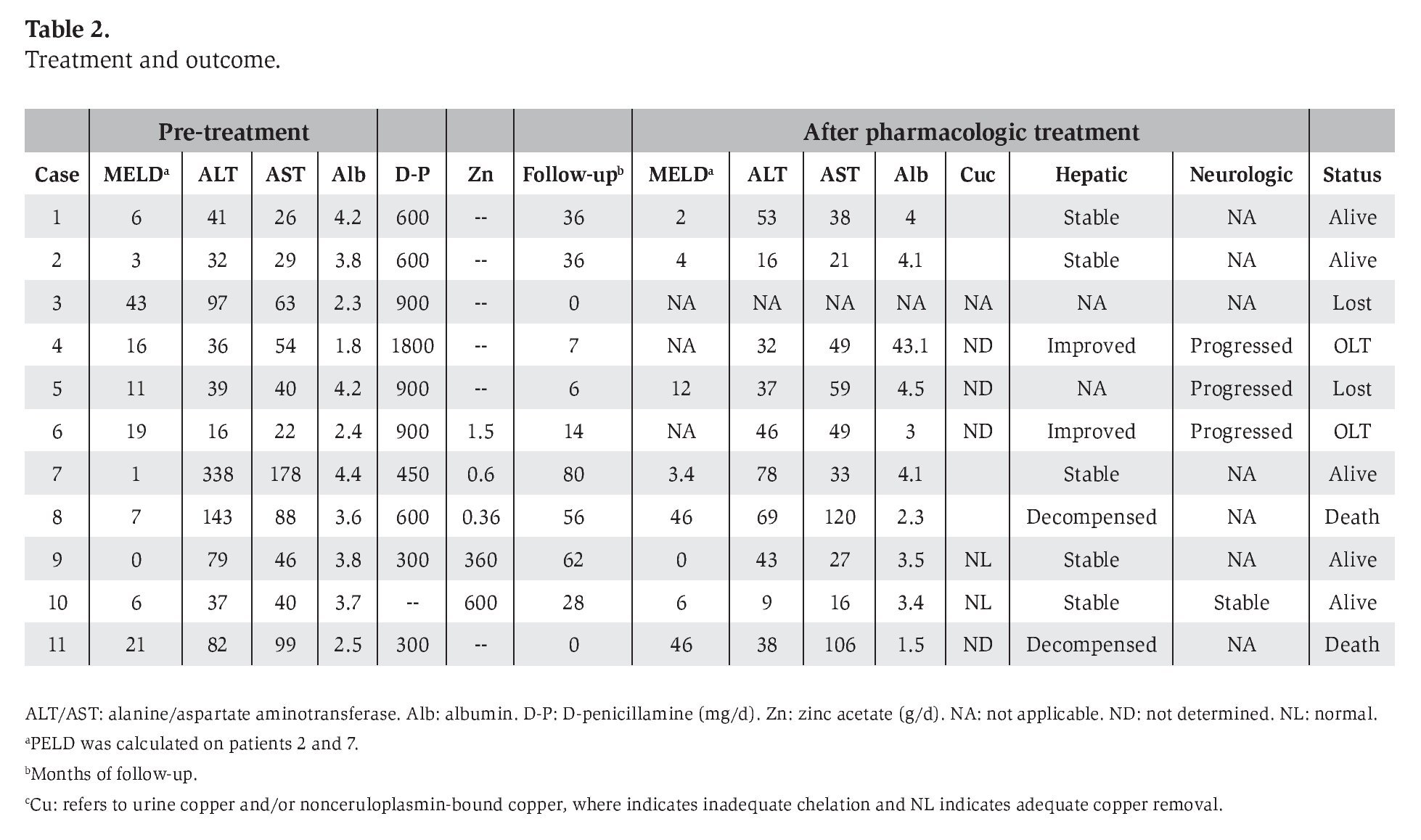
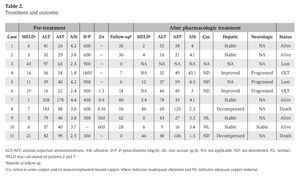
Median follow-up on this series was 28 months (range: 0 to 80 months). Pharmacologic treatment included D-penicillamine in ten patients and oral zinc in five (four had combination therapy) (Table 2). Of the seven patients who had only hepatic manifestations (cases 1-3, 7-9 and 11), normalization of copper metabolism was achieved only in one (case 9), and there were follow-up inconsistencies in four (cases 1-3 and 7) that impeded adequate chelating treatment (patient 3 was lost to follow-up on the day D-penicillamine was started). There were two deaths: patient 8 declined LT because of religious beliefs, and he had a rapid deterioration of hepatic disease during a period of repeatedly starting and discontinuing D-penicillamine, and finally died after an episode of variceal bleeding followed by hepatorenal syndrome; while patient 11 developed spontaneous bacterial peritonitis three days after the beginning of pharmacologic treatment, and died because of sepsis and multiple organ failure.
When considering patients with both hepatic and neuropsychiatric manifestations, two patients (cases 4 and 6) had marked improvement in hepatic disease, but frank deterioration of neurological status, with worsening of gait disturbances, and development of tremor and choreic movements. In the first, initial neurological deterioration seemed to be related to administration of D-penicillamine, but for both cases neurological disease progressed in spite of adequation of treatment. Consequently, LT was indicated after which, neurological remission of all manifestations occurred. Both patients are alive and performing normal activities after 4 and 6 years of definite treatment. The last patient (case 10) has remained stable for both hepatic and neurological disease, only with zinc-based therapy, achieving adequate copper metabolism goals. These three patients have had disappearance of the Kayser-Fleischer ring. Patient 5, who had only neuropsychiatric phenomena, was unfortunately lost after only 6 months of follow-up. This patient had also been considered for LT, given that his neurological signs worsened after D-penicillamine was started.
Brain MRI was performed on the four patients with neuropsychiatric manifestations. The main findings were: generalized atrophy, dilatation of ventricles, high signal intensity on T2 weighted images in the putamen and decreased signal intensity in basal ganglia. In the 2 patients treated with LT, a follow-up MRI after 6 months of the procedure showed total resolution of brain lesions in one, and marked improvement in the other.
Discussion
In the majority of patients with suspected WD, the diagnosis was not confirmed because of inadequate follow-up, a condition that may respond to the fact that most patients were referred from underdeveloped areas in the country, and thus continuing consultation was difficult. Clinical presentation was not different to what has been reported in the literature, with establishment of diagnosis during the second and third decades of life.1,6 However, it is noticeable that no cases of fulminant liver failure, or patients with hemolytic anemia, were identified. This can be due to referral bias (since most patients are stable and referred from other institutions) or to a lack of clinical suspicion.
Regarding genetic analysis, identification of the H1069Q homozygous haplotype on the ATP7B gene, was rather an expected result, given the European ancestry of the Mexican mestizo population. This mutation predominates among different European countries,3 including a series of WD patients from Spain (our main European genetic ancestry).7 To our knowledge, there are no published series of genetic testing among mestizo patients in Latin America (except for Brazil), although it is predictable that it may not differ substantially from European series. Brazil and possibly some other Caribbean populations might represent an exception given their highly multiracial mixture, as already shown in a Brazilian series.8 This issue merits further studies among Mexican mestizo lineage, since other mutations may be prevalent among possible subpopulations. Finally, this patient had neurologic disease, an already described association.9
Irregular availability of D-penicillamine, scarcity of zinc preparations, and lack of alternative treatment with trientine, all affected pharmacologic treatment in the current series of WD, obtaining a low rate of successful de-coppering therapy (only 2, out of 9 patients on chelating treatment). However, 3 more patients have remained stable during a follow-up of 36-80 months. Exacerbation of neurological symptoms with D-penicillamine was evidenced in 2 out of 4 patients, a figure above the frequency of 20-30% reported in the literature.1,10
LT is not widely available in our country, aside from referral centers, owing to varied reasons, including religious concerns. Successful transplantation was accomplished in 2 of our patients. They had experienced progression of neurological manifestations while on adequate chelating treatment. It was very noticeable that these patients achieved neurological remission after orthotopic LT, including disappearance or frank improvement of previously documented abnormalities on MRI within a period of 6 months.
According to the AASLD guidelines, LT is considered in patients with WD when decompensated liver disease unresponsive to medical therapy occurs, or in cases with fulminant hepatic failure; whereas the indication for neurological progression is controversial, based on previous reports that did not demonstrate a beneficial neurological outcome.4 Currently, most authors adhere to these indications for LT,2,6,11 although for some, progression of neurological manifestation while on pharmacologic treatment also implies performance of LT irrespective of liver function status.1,12-14 This indication has derived from numerous case reports on successful improvement of neurological manifestations after LT, although a publication bias cannot be ruled out. Stracciari et al reported a well-documented case of global neurological improvement after LT on a patient with WD, and made an analysis of existing literature, estimating that 78% of patients improve their neurological status after the procedure.15 Since then, several other patients with neurological disease have benefited from orthotopic or living-related LT, overcoming the number of patients with neurological deterioration or transplantation-related death (including the current series, 44 vs 4 cases, respectively).12-14,16-23 The cause of a flawed outcome has been mostly related to complications inherent to LT, although frank neurological deterioration has also been documented.18 Additionally, healing of brain lesions has been demonstrated according to serial MRI or CT scan in the post-operative stage.15,22-24 The neurological improvement (on clinical grounds and imaging studies) after orthotopic LT observed in our patients adds evidence on the issue of considering progressing neurological manifestations as an indication for LT in patients with WD.
Establishing LT as an indication for the treatment of neurological manifestations on patients with WD (progressing neurological disease in spite of medical treatment) seems logical given the exposed evidence, and due to the fact that transplanted patients have a quality of life similar to that of matched controls from the general population.25 Although a randomized clinical trial could efficiently resolve this issue, it does not seem to be possible, according to ethical principles. Therefore, it should be strongly considered, especially in patients with stable hepatic function and before incapacitating or irreversible central nervous system damage occurs. Also, it could represent an adequate alternative for a majority of patients in whom neurological manifestations fail to respond to D-penicillamine,26 especially in countries with a restricted pharmacologic armamentarium, but with centers having a consolidated team on LT.
Abbreviations: Wilson's disease (WD), Liver transplantation (LT), International Classification of Diseases (ICD-10), Magnetic resonance imaging (MRI).
Grants and fi nancial support:Dr. Duarte reports receiving fellowship support from the Fundación Mexicana para la Salud Hepática (estímulo Ángeles Espinosa Yglesias).
Correspondence author: Aldo Torre. Department of Gastroenterology.
Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán". Vasco de Quiroga #15, Tlalpan, C.P. 14000. México City, México Phone: +52 55 5573 3418. Fax: +52 55 5655 0942.
E-mail: detoal@yahoo.com
Received: January 13th, 2009 Accepted on: May 26th, 2009