¿ Abstract
Recognizing nonerosive reflux disease (NERD) is a distinct presentation of gastroesophageal reflux disease (GERD) was one of the most important developments in the field of GERD in the last decade. Whilst the definition of NERD has not changed significantly over the years, the disorder accounts for the majority of the GERD patients and those who failed proton pump inhibitors (PPI) treatment. Recent developments in NERD have focused primarily on understanding its pathophysiology and natural history. The introduction of the esophageal impedance/pH monitoring has led to the assessment of other forms of gastroesophageal reflux in causing NERD. Therapeutic modalities still focus on acid suppression, but there is growing recognition that other therapeutic strategies should be considered in NERD.
¿ Introduction
It has been demonstrated that 44% of the US population report GERD-related symptoms at least once a month and 20% do so once a week.1,2 Furthermore, due to the close relationship between GERD and body mass index (BMI), it is highly likely that the prevalence of GERD will closely follow the increase in BMI that is expected in the future.
Most patients with GERD fall into one of two categories: NERD or erosive esophagitis. The two main phenotypes of GERD appear to have different pathophysiological and clinical characteristics. Furthermore, NERD and erosive esophagitis clearly diverge regarding response to antire-flux treatment. NERD patients have a significantly lower response rate to PPI therapy, and consequently they constitute the majority of the refractory heartburn group.3,4
¿ Definition
NERD has been commonly defined as the presence of classic GERD symptoms in the absence of esophageal mucosal injury during upper endos-copy. The Genval Workshop suggested that the definition of NERD should be reserved for individuals who fulfill the definition of GERD, but who do not have either Barrett's esophagus or definite endoscopic esophageal mucosal breaks (erosion or ulceration).5 We proposed that NERD should be defined as the presence of typical symptoms of GERD caused by intraesophageal reflux (acidic or weakly acidic), in the absence of visible esophageal mucosal injury at endoscopy.1
Recently, the Montreal International Consensus defined GERD as a condition that develops when the reflux of stomach contents causes troublesome reflux-associated symptoms, and NERD was defined by the presence of these symptoms in the absence of esophageal mucosal breaks.6
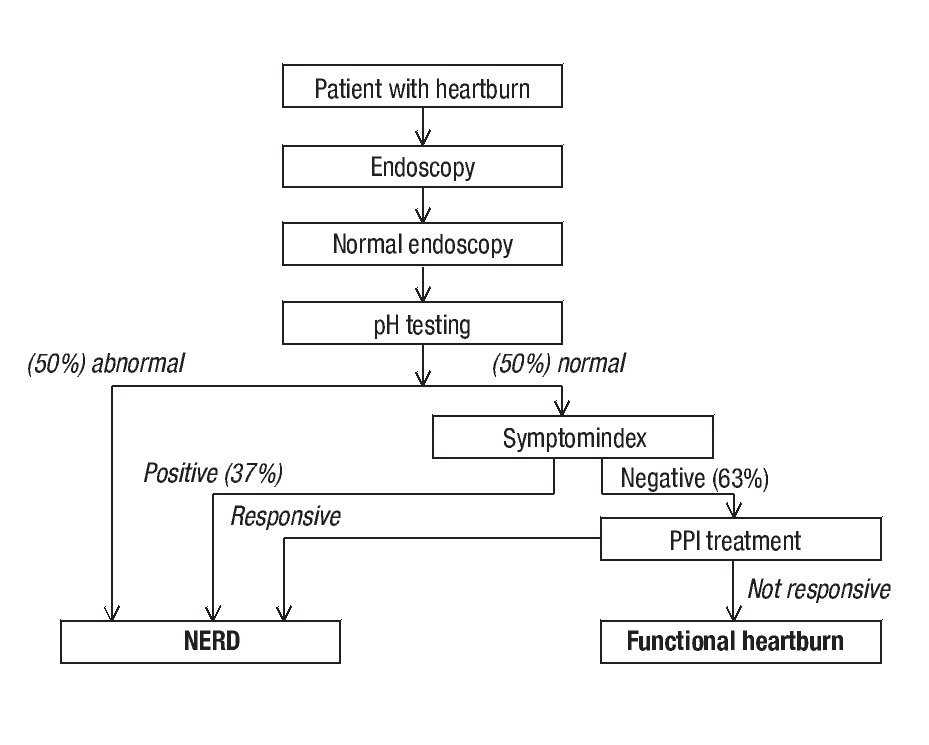
Studies have shown that about 30%-50% of NERD patients demonstrate esophageal acid exposure within the physiological range.7 The Rome II Committee for Functional Esophageal Disorders considered these patients as having functional heartburn, defined as "episodic retrosternal burning in the absence of pathological gastroesophageal reflux, pathology-based motility disorders, or structural explanations.8 This subgroup was further divided into 2 subgroups. The first one included patients who demonstrated a close temporal relationship between their heartburn symptoms and acid reflux events, in spite of having a physiological range of esophageal acid exposure. This "hypersensitive esophagus" subgroup accounts for up to 40% of the patients with functional heart-burn.7 Patients with hypersensitive esophagus demonstrate partial response to PPI treatment. 9 In contrast, the other subgroup (accounting for up to 60% of the patients) demonstrates no correlation between heartburn episodes and acid reflux events. The Rome III Committee for Functional Esophageal Disorders redefined the functional heart-burn group, and consequently NERD, by primarily incorporating the hypersensitive esophagus group and patients with negative symptom association who are responsive to PPI treatment back into the NERD group (Figure 1).10
¿ Figure 1. A diagnostic algorithm for NERD and functional heartburn based on Rome III criteria.53
¿ Treatment
PPIs are currently considered the most effective and safe therapeutic modality for GERD. In clinical trials, these agents have consistently been demonstrated to be more effective than any other acid-suppressant agent in healing erosive esophagitis and relieving GERD-related symptoms. The superior efficacy of PPIs is also observed in NERD patients. In a recent meta-analysis, van Pinxteren et al. demonstrated that the relative risk (RR) for heartburn remission in NERD patients from placebo-controlled trials was 0.68 (95% CI: 0.59-0.78) for PPIs vs. placebo and 0.84 (95% CI: 0.74-0.95) for histamine-2 receptor antagonistss (H2RAs) vs. placebo.11 The RR for PPIs vs. H2RAs was 0.74 (95% CI: 0.53-1.03).
A number of studies have evaluated the efficacy of PPIs in NERD patients. In a multicenter, randomized, double-blind study involving 209 patients, omeprazole 20 mg once daily was compared with placebo in controlling NERD symptoms.12 After 4 weeks of therapy, 57% of patients in the omeprazole group were free of heartburn, 75% were free of acid regurgitation, and 43% were completely asymptomatic. In another study, NERD patients were randomized to omeprazole 20 mg/ day, omeprazole 10 mg/day or placebo.13 Researchers found that at 4 weeks, 46% of patients treated with omeprazole 20 mg/day, 31% treated with omeprazole 10 mg/day, and 13% of those on placebo reported complete relief of heartburn. Miner et al. enrolled 203 patients with NERD who were randomized to either rabeprazole 20 mg once daily or placebo. After 4 weeks, 56.7% of the patients receiving rabeprazole reported satisfactory symptom relief vs. 32.2% of those receiving placebo (P < 0.008).14 A recent study that utilized the wireless pH capsule demonstrated that PPIs can normalize esophageal acid exposure in patients with NERD within 48 hours of initial administration.15
In general, the proportion of NERD patients responding to a standard dose of PPI is approximately 20%-30% lower than what has been documented in patients with erosive esophagitis. In a systematic review of the literature, PPI symptomatic response pooled rate was 36.7% (95% CI: 34.1-39.3) in NERD patients and 55.5% (95% CI: 51.5-59.5) in those with erosive esophagitis.16 Therapeutic gain was 27.5% in NERD as compared with 48.9% in erosive esophagitis. Moreover, patients with NERD demonstrate a close relationship between response to PPI therapy and the degree of esophageal acid exposure. The greater the distal esophageal acid exposure, the higher the proportion of NERD patients reporting symptom resolution.13 This is opposite to what has been observed in patients with erosive esophagitis, in whom increased esophageal inflammation has been associated with a lower response rate to PPI once daily. NERD patients also demonstrate longer lag time to sustained symptom response (2 to 3-fold) when compared to patients with erosive esophagitis. Furthermore, NERD patients demonstrate similar symptomatic response to half and full standard dose of PPI17, unlike patients with erosive esophagitis who demonstrate an incremental increase in healing and symptom resolution. In one study, the time to both first and sustained relief of reflux symptoms during PPI treatment in NERD patients was assessed by the ReQuestTM questionnaire. Both pantoprazole (20 mg/day) and esomeprazole (20 mg/day) were shown to provide a similar median time to first symptom relief (2 days) and to sustained symptom relief (10-13 days).18 The reason for the differences in therapeutic response parameters between NERD and erosive esophagitis is primarily due to the common inclusion of functional heartburn subjects in the NERD group. However, because most NERD patients demonstrate only modest abnormal esophageal acid exposure, even after excluding functional heartburn patients, the symptomatic response rate of NERD patients to PPI remains lower than that seen in erosive esophagitis patients.
Because GERD is mostly a non-progressive disorder, treatment for many of these patients could be symptom-driven. Thus, on-demand or intermittent therapy with a PPI is an attractive therapeutic strategy for NERD patients in clinical practice.19, 20 These therapeutic approaches are convenient, allow patients to remain in control, are cost effective, and decrease the likelihood of rebound of acid secretion. Studies have demonstrated that intermittent or on-demand PPI therapy in NERD is effective and associated with improved quality of life as well as reduced cost.21,22
Dexlansoprazole MR, a novel modified-release formulation of dexlansoprazole, which incorporates dual delayed-release technology designed to prolong the serum concentration-time profile thus provididing extended acid-suppression, has been recently assessed in NERD patients. Dexlansoprazole 30 mg daily for 4 weeks was shown to be superior to placebo in providing 24-hour heart-burn-free days and nights (54.9% vs. 17.5% and
80.8% vs. 51.7%, respectively).23
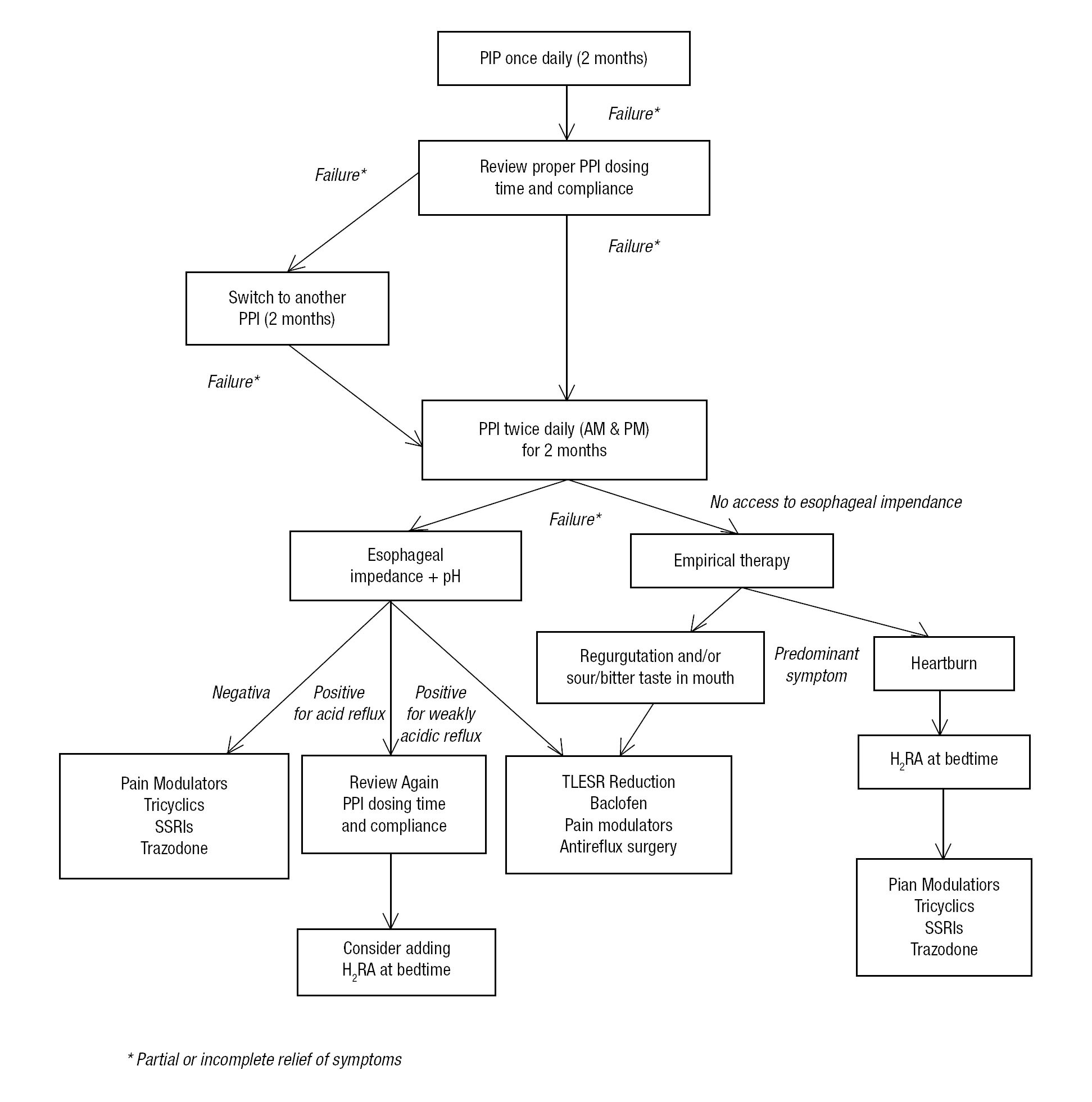
Novel therapeutic modalities are currently being considered for GERD patients and specifically those with NERD. The main areas of interest include improving acid suppression, reducing the transient lower esophageal sphincter relaxation rate, decreasing esophageal sensitivity, and enhancing esophageal motility (Figure 2).
¿ Figure 2.Algorithm for treating refractory NERD patients.54
Response to antireflux surgery has been shown to be different between patients with NERD and those with erosive esophagitis. Fenton et al. compared the clinical outcome of antireflux surgery in patients with erosive esophagitis and NERD patients, demonstrating that 91% vs. 56% reported heartburn resolution, 24% vs. 50% reported dysphagia following surgery, and 94% vs. 79% were satisfied with surgery, respectively.24
¿ Treatment for Refractory NERD
Transient Lower Esophageal Sphincter Relaxation (TLESR) Reducers
A wide range of receptors have been shown to be involved in triggering TLESR providing us with the opportunity to develop novel reflux inhibitors.25 Most promising among these appear to be gamma-aminobutyric acid B (GABAB) receptor agonists and metabotropic glutamate receptor 5 (mGluR5) antagonists, which can achieve high levels of TLESR's inhibition.25,26
Baclofen, a GABAB agonist, was introduced into the clinical arena as a potential add-on treatment for patients in whom PPI treatment (once or twice daily) has failed.27,28 Baclofen reduced TLESR rate by 40%-60% and reflux episodes by 43%; in addition, it increased lower esophageal sphincter basal pressure and accelerated gastric emptying.27-29 Baclofen has been shown to significantly reduce duodeno-gastrooesophageal reflux (DGER) and weakly acidic reflux as well as DGER-related symptoms.30,31 In subjects with persistent heartburn despite PPI treatment, doses of up to 20 mg 3 times daily have been used.30 Because the drug crosses the blood-brain barrier, a variety of central nervous system (CNS)-related side effects have been reported, primarily including somnolence, confusion, dizziness, lightheadedness, drowsiness, weakness, and trembling. Side effects are likely an important limiting factor in the routine use of baclofen in clinical practice.
Arbaclofen placarbil (also known as XP19986) is a novel transported prodrug of the baclofen's pharmacologically active R-isomer. It is currently in clinical development for the treatment of refractory GERD. Arbaclofen placarbil was designed to be efficiently absorbed in the gastrointestinal tract and rapidly metabolized to release R-baclofen after absorption. Unlike baclofen, arbaclofen placarbil is well absorbed from the colon, allowing the drug to be delivered in a sustained release formulation that may allow less frequent dosing and thus reduced fluctuations in plasma exposure. This in turn may lead to potentially improved efficacy through a combination of greater duration of action, subject's convenience, and a better safety profile than baclofen.32,33
The effect of ADX10059 on esophageal acid exposure and symptoms has been recently evaluated in GERD patients. Given at a dose of 250 mg 3 times daily, this potent, selective, negative allosteric modulator (NAM) of mGluR5 significantly reduced the percentage of time below pH 4 and the duration of symptomatic reflux episodes. In the study, ADX10059 was generally well tolerated. Based on these preliminary data, the mGluR5 NAM ADX10059 appeared to have a potential role in the clinical management of GERD.34 However, on December 14, 2009, Addex Pharmaceuticals Ltd. ended the development of ADX10059 because of a possible association with severe hepatic side effects. The adverse events occurred regardless of the dose and appeared to be related to the duration of drug administration.
¿ Visceral Pain Modulators
Thus far, no studies have specifically assessed the value of visceral pain modulators in refractory GERD patients. However, given the fact that most patients who fail PPI treatment belong to the NERD group and more than 50% of the (twice daily PPI) failure subjects demonstrate lack of either weakly or acidic reflux, the usage of these agents is highly attractive.35,36 Additionally, it could be argued that visceral pain modulators could be helpful even for weakly acidic reflux that has not been shown to be associated with esophageal mucosal damage. Pain modulators such as tricyclic antidepressants, trazodone (a tetracyclic antidepressant), and selective serotonin reuptake inhibitors (SSRIs) have all been shown to improve esophageal pain in patients with noncardiac chest pain.35,37,38 It is believed that the visceral analgesic effect from these agents results from their action on the central nervous system and/or peripheral action at the sensory afferent level.
Pain modulators are used in non-mood-altering doses, and they presently provide a therapeutic alternative until more novel esophageal-specific compounds become available. Side effects are relatively common and may limit their usage in certain patient populations such as the elderly and those with multiple comorbidities.
¿ Botulinum Toxin Injection
In a recent study, botulinum toxin was administered by pyloric injection to 11 patients with refractory GERD and associated gastroparesis.39 Marked improvement in GERD-related symptoms, which correlated with improvement in gastroparesis-related symptoms and gastric-emptying scintigraphy was demonstrated. The mean duration of response is approximately 5 months.40
¿ Antireflux Surgery
A recent surgical study reported that refractory GERD was the most common indication for antire-flux surgery, accounting for such in 88% of the cases.41 Interestingly, the most common preoperative symptom reported under failure of medical antire-flux treatment was regurgitation (54%). Overall, 82% of the patients reported that the preoperative reflux symptom completely resolved, and 94% were satisfied with the results of the surgery. In another study involving only 30 subjects with refractory GERD who were followed for a 12-month period, main preoperative symptoms were regurgitation (93%) and heartburn (60%). At the end of a 1-year follow-up post-surgery, all patients reported complete heartburn relief, and 86% reported resolution of regurgitation. Patients' satisfaction rate with surgery was 87%.
Three recent studies suggested that a positive SI during impedance-pH monitoring in patients on PPI can predict a favorable response to medical or surgical therapy. The first study by Mainie et al. followed 19 patients who were refractory to a double-dose PPI and underwent successful laparoscopic Nissen fundoplication.42 Prior to surgery, 18 of the 19 patients were found to have a positive SI on combined multichannel intraluminal impedance (MII)-pH monitoring (14 with non-acid and 4 with acid reflux). After a mean follow-up of 14 months, 16 patients with a positive SI were asymptomatic. The second study by Becker et al. assessed 56 patients with persistent symptoms on a single dose of PPI and an abnormal MII- pH monitoring.43 Most of these patients later demonstrated a significantly higher response rate to doubling the PPI dose as compared to subjects with normal MII-pH monitoring. In a third study, a group of Italian investigators prospectively assessed the outcomes of laparoscopic Nissen fundoplication in 62 patients who were PPI nonresponsive or noncompliant.44 All surgically treated patients had a positive MII-pH monitoring. The overall patient satisfaction rate was 98.3%, and no differences were found in clinical outcomes based on their preoperative MII-pH or manometry results. It was concluded that MII-pH provides useful information for a better selection of patients for antireflux surgery and that laparoscopic Nissen fundoplication results in excellent outcomes primarily in patients with positive MII-pH monitoring or SI. Unfortunately, all the aforementioned studies were uncontrolled and did not clearly describe whether symptoms were due to residual reflux.
¿ Alternative Medicine
The value of acupuncture has been recently evaluated in GERD patients who failed PPI once daily.45 When compared to doubling the PPI dose (standard of care), adding acupuncture was significantly better in controlling regurgitation and both daytime and nighttime heartburn. This is the first study to suggest that alternative approaches for treating visceral pain may have a role in GERD patients with persistent heartburn despite PPI therapy.
¿ Psychological Treatment
Patients with poor correlation of symptoms with acid-reflux events display a high level of anxiety and hysteria as compared with patients who demonstrate a close correlation between symptoms and acid-reflux events.46 Anxiety and depression have been shown to increase GERD-related symptoms reporting in population-based studies. Nojkov et al. provided the first evidence that response to PPI treatment may be dependent on the level of psychological distress.47 Thus, it has been proposed that a subset of patients who do not respond to PPI therapy are more likely to have a psychosocial comorbidity than those who are successfully treated with a PPI. In these patients, treatment directed toward underlying psychosocial abnormality may improve response to PPI therapy.
¿ Future Therapy
Several directions in drug development have been pursued in patients who failed PPI treatment. These include an earlier, more profound acid suppression, reduction of the rate of TLESR, improved esophageal and/or gastric motility, attenuation of esophageal pain, and mucosal coating of the esophagus.
Vecam, a combination of a PPI and succinic acid (an acid pump activator, VB101), demonstrated a meal-independent antisecretory effect. Oral administration of succinic acid in humans displays the same acid-stimulating activity as pentagastrin. This resulted in augmented PPI effects in rats.48
AGN 201904-Z is a slowly absorbed, acid-stable pro-PPI that rapidly converts to omeprazole in the systemic circulation. A single oral dose provides continued metered absorption (CMA) that prolongs plasma residence time. Consequently, the activated proton pumps are exposed to the drug over longer periods of time. In a 5-day phase I study, AGN 201904-Z resulted in a significantly greater acid suppression than esomeprazole 40 mg per day. Nocturnal acid suppression was significantly greater with AGN 201904-Z than with esomeprazole 40 mg per day. AGN 201904-Z also reduced the proportion of patients with episodes of nocturnal acid breakthrough (NAB) (25% vs. 100%).49
Tenatoprazole is an imidazopyridine-based PPI with a prolonged plasma half-life. Tenatoprazole 40 mg daily provides better nighttime acid control than esomeprazole 40 mg once daily. In a single-center, double-blind, double-dummy, randomized, 4-way, cross-over study that was conducted in 32 healthy male subjects, S-tenatoprazole-sodium produced significantly greater and more prolonged dose-dependent 24-h and nocturnal acid suppression than esomeprazole 40 mg.50
Several new compounds that combine a PPI with an H2RA have been recently evaluated. They are all still in early stages of development. The fast-dissolving OX 17 is a fixed-dose combination of omeprazole and famotidine. This drug has undergone several phase II/III clinical trials.51 In addition, a combination of an H2RA with tenatoprazole has also been recently patented.52 Further studies are needed to determine the value of these compounds in refractory GERD patients.
As previously mentioned, the main focus for drug development in refractory GERD patients is TLESR reduction and a more potent, early, and consistent acid suppression. However, due to the diverse causes of PPI failure, a single therapeutic strategy may not be the solution for all patients. It is likely that individually tailored therapy would be the most proper management approach.
Abbreviations used:
GERD = gastroesophageal reflux disease
NERD = nonerosive reflux disease
EE = erosive esophagitis
Correspondence: Professor Ronnie Fass, MD, FACP, FACG.
Chief of Gastroenterology. Southern Arizona VA Health Care System. 3601 S. 6th Avenue
(1-111-GI). Tucson, AZ 85723-0001 USA.
Phone: 520 792 1450, ext. 5139. Fax: 520 629 4737.
Email: Ronnie.Fass@va.gov