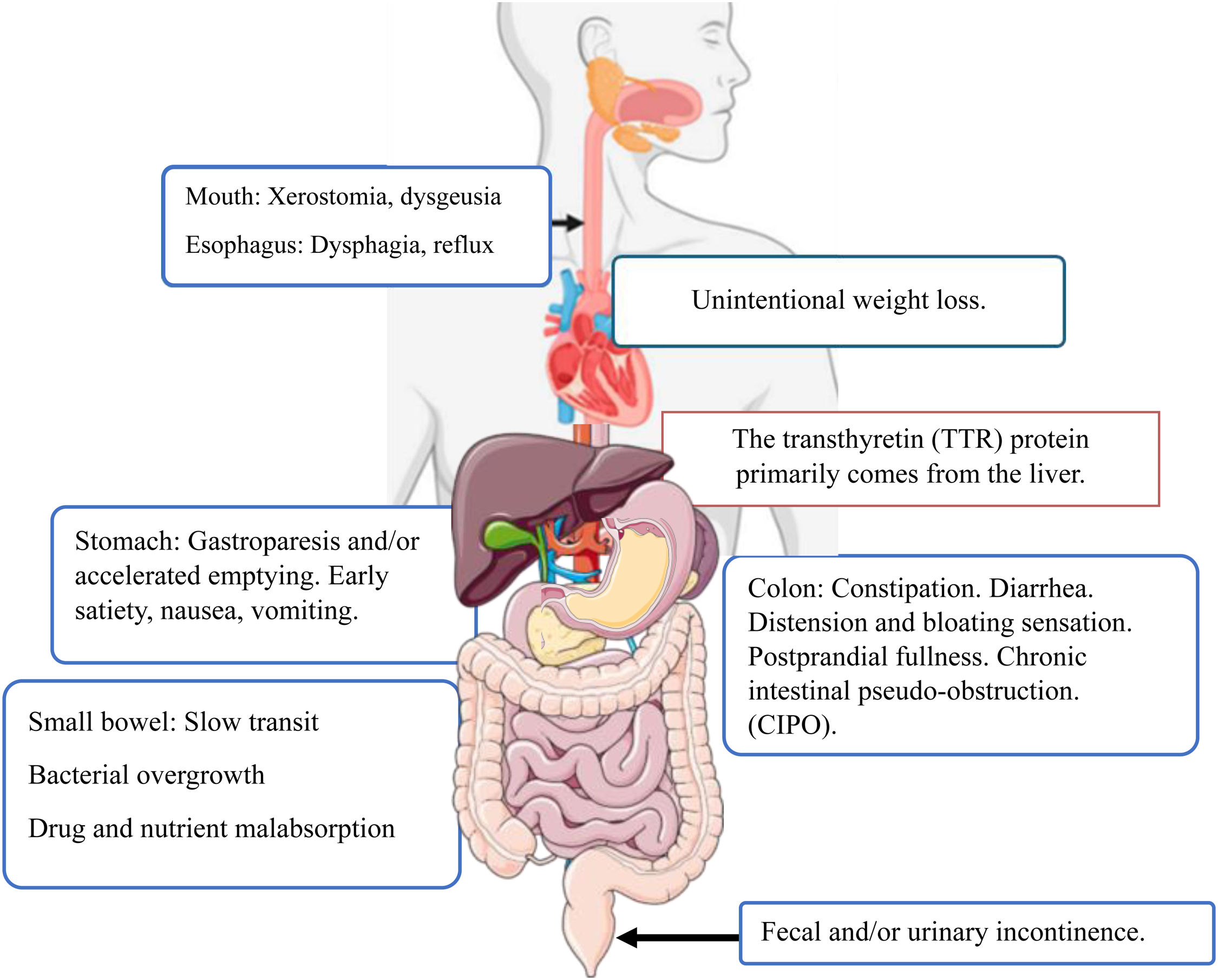
Dysphagia, early satiety, postprandial fullness, nausea, vomiting, and unintentional weight loss are symptoms that may correspond to those of hereditary transthyretin amyloidosis (hATTR). Regardless of causal genotype, 56 to 69% of persons with hATTR report gastrointestinal manifestations.1 hATTR is a systemic disease, with progressive deterioration, caused by the deposit of amyloid fibers in different organs and tissues.2 It can simulate bowel occlusion or present as autonomic diarrhea (constipation that alternates with diarrhea) due to amyloidosis of the autonomic nervous system and the intestine.3 Presentation age varies from 30 to 40 years. In Mexico, 10% of the reported cases present with gastrointestinal manifestations.4 hATTR may present as polyneuropathy or cardiomyopathy, but other organs, such as the eye or gastrointestinal system, are involved.5 Gastrointestinal symptoms can be nonspecific, overlooked, or dismissed as functional. There is increasing recognition of cases of hATTR worldwide (10,000 annually since 2018), with a prevalence of 1 in every 450,000 inhabitants.1 There are endemic zones in Mexico (Guerrero, Morelos, Guanajuato), with a mean presentation age of 37 years and a prevalence of 0.89 cases in every 100,000 inhabitants.4 Gastrointestinal manifestations generate an important burden on quality of life, due to autonomic neuropathy and infiltration of the enteral plexus,6 and are the second reason for care in patients with hATTR in Mexico.4 Gastrointestinal manifestations can present insidiously and nonspecifically, resulting in multiple visits to specialists before the definitive diagnosis is made (Fig. 1).
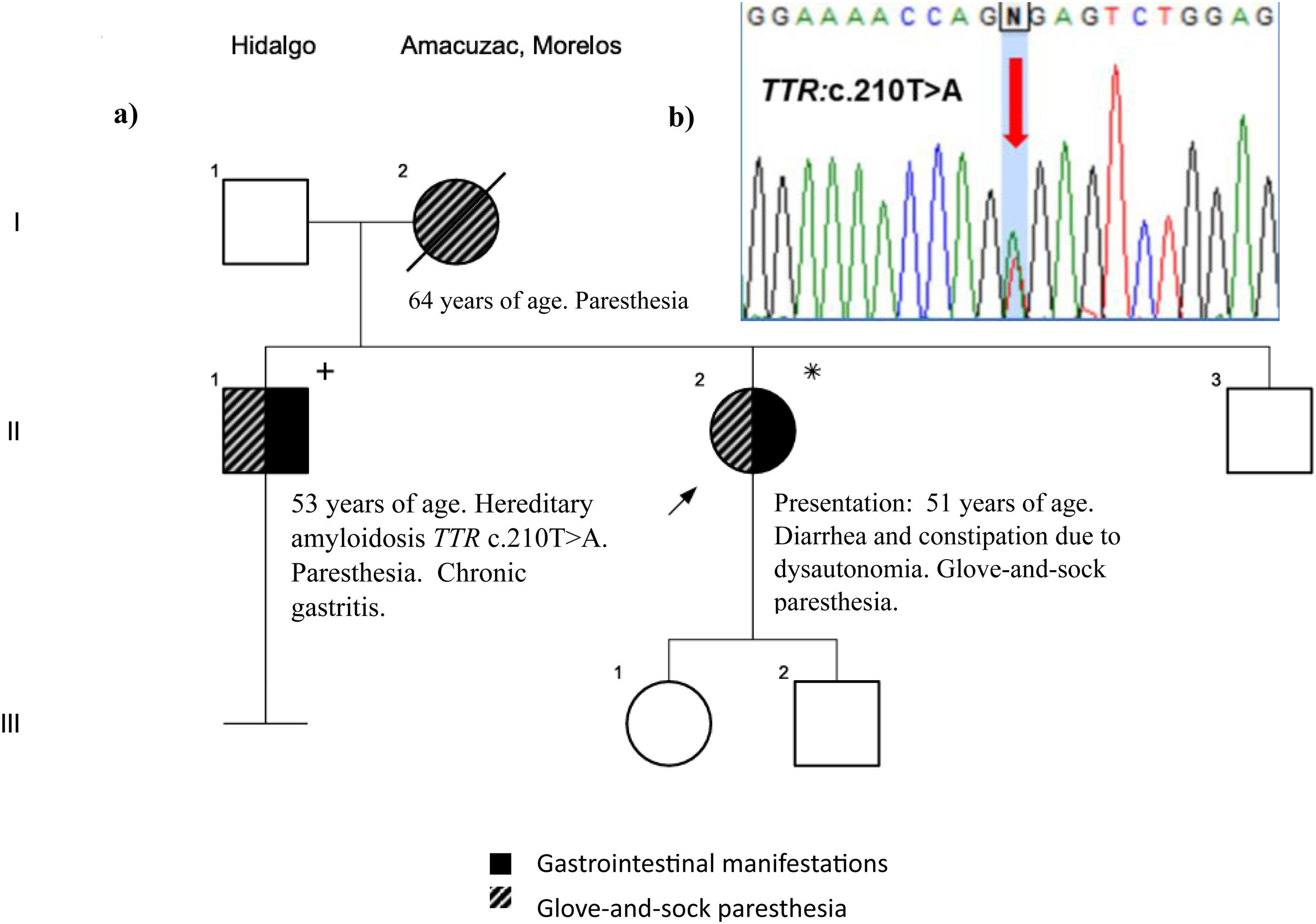
A 51-year-old woman presented with constipation and diarrhea, weight loss, epigastric pain, early satiety, and postprandial fullness of 6-month progression. She went to the emergency room on 8 occasions due to diarrhea and vomiting, receiving numerous treatments for gastroenteritis, with no improvement. The epigastric pain worsened over the past 2 months, was colicky and nonradiating, and accompanied with nausea and vomiting. Her family history showed that her mother had died from multiple sclerosis at 59 years of age and her surgical history revealed a left corneal transplant at 35 years of age, graft loss at 5 months, and two retransplants. She has had high blood pressure for 8 years (treatment: losartan/hydrochlorothiazide). The patient was hospitalized for uncontrollable vomiting, dehydration, and ileus (HR: 70 bpm; RR: 18x’; temperature: 36.7 °C; BP: 130/90 mmHg; height 1.68 m; weight 76 kg; BMI 27.6 kg/m2). A nasogastric tube was placed (fecaloid output 120 ml in 24 h). We calculated an unintentional weight loss of 35 kg (previous weight: 111 kg, weight at admission: 76 kg). Laboratory tests: mild hypokalemia: 3.10 mmol/l, uric acid 8.10 mg/dl, alanine aminotransferase 57 U/l, amylase 126 U/l, lipase 439 U/l, PT 21.10 s, triglycerides 87 mg/dl, and total bilirubin 1.10 mg/dl. No biochemical cause of ileus was found nor were there signs of mechanical obstruction on the abdominal X-ray, ultrasound, or tomography studies. Esophagogastroduodenoscopy was carried out later, only identifying Los Angeles grade A esophagitis and erosive gastropathy. The endoscopic findings did not completely explain the gastrointestinal symptoms, and we consulted the Genetics Department, upon discovering that the patient’s brother presented with the same insidious symptoms, leading to the diagnosis of hATTR. In the family genealogy there was an autosomal dominant pattern (Fig. 2a): mother (I.2) died presenting with polyneuropathy and emaciation, with hATTR a consideration in the differential diagnosis of multiple sclerosis; brother (II.1), 53 years of age, presented with abdominal pain, constipation, inguinal pain after hernia repair, chronic gastritis, and distal glove-and-sock paresthesia. The maternal family was from an endemic region for hATTR in Mexico (Amacuzac, Cuernavaca).4 Upon having the genetic diagnosis, the episodes of ileus were considered secondary to chronic intestinal pseudo-obstruction (CIPO) due to dysautonomia. Other manifestations of dysautonomia were found (dry eyes, xerostomia, urinary incontinence), sensory neuropathy (glove-and-sock paresthesia, hypoesthesia, altered thermoregulation), motor neuropathy (distal muscular hypotrophy), and carpel-tunnel syndrome. The diagnosis was confirmed through sequencing of the TTR gene (Fig. 2b).
a) Genealogy with dominant autosomal pattern for hATTR. b) Electropherogram of the TTR gene (GENOS MÉDICA laboratory). Red arrow: pathogenic variant in the heterozygous state, a change from thymine to adenine (TTR c.210T>A) that affects the amino acid sequence (p.Ser70Arg) in the transthyretin protein.
The patient’s prior corneal implant loss was attributed to keratoconjunctivitis sicca and neurotrophic keratopathy, seen in hATTR. Other target organs were evaluated, reporting euthyroid hyperthyroxinemia and stage IV chronic kidney disease. The patient was referred to tertiary care for treatment (inotersen). An electromyography/nerve conduction study confirmed the presence of axonal sensorimotor polyneuropathy in the limbs, but there is limited access to demonstrating enteric involvement of the autonomic nervous system through biopsy or scintigraphy in our environment.
hATTR is an autosomal dominant condition caused by mutations in the TTR gene and has a prevalence of 1-9/1,000,000.7 Gastroparesis, constipation, and POIC are frequent complications of this disease.3,6 In a cross-sectional study, manifestations included unintentional weight loss (31.5%), early satiety (26.4%), alternating constipation and diarrhea (24.3%), nausea and vomiting (10 to 20%), and fecal incontinence (6.2%).6 Unintentional weight loss was an alarm symptom.7 hATTR can produce gastrointestinal manifestations several years before neuropathy and myocardiopathy, making the timely diagnosis indispensable.8–10 The present article is the first to highlight gastrointestinal manifestations in a case of hATTR in Mexico, as well as the first case diagnosed in the State of Hidalgo.
Financial disclosureThe present work has received no external financial support for its development and publication. The diagnostic test of the TTR gene was carried out as part of a no-cost protocol, sponsored by PTC Therapeutics, currently in force for patients and families with hATTR. Authorization was obtained from the GENOS MÉDICA laboratory for the use of the electropherogram as a key image. No financial support was necessary.
Ethical considerationsThe patients signed statements of informed consent and a privacy notice for the genetic study. Written and signed informed consent was requested of the patients for the data collection and participation in this review and its publication. Routine written and duly signed consent was obtained from the patients for the endoscopic procedure. Prior to obtaining the DNA for analysis, the advantages and disadvantages of the genetic study were explained to the patients. The counseling was completed, and written statements of consent were signed for sending the samples and processing the 10 ml of venous blood in EDTA tubes. This article corresponds to a retrospective analysis of a single case, following the current bioethical research norms. Given that it is a retrospective case record review, authorization by the Ethics in Research Committee was not required for the diagnosis or molecular confirmation of the case. The Ethics in Research Committee of the Hospital General de Tulancingo was informed. The authors declare that this article contains no personal information that could identify patients, and we have the authorization of the patients for this publication.
The authors declare that there is no conflict of interest.