Irritable Bowel Syndrome (IBS) is a disorder characterized by abdominal pain or discomfort associated with changes in bowel habit. Currently there are no objective outcome measures for evaluating the effectiveness of treatments for this disorder.
AimsTo determine the usefulness of a method of analysis that employs polar vectors to evaluate the effectiveness of IBS treatments.
MethodsData from a Phase IV clinical study with 1677 active IBS-Rome III patients who received 100mg of pinaverium bromide+300mg of simethicone (PB+S) po bid for a period of four weeks were used for the analysis. Using the Bristol Stool Scale as a reference, the consistency and frequency of each type of bowel movement were recorded weekly in a Bristol Matrix (BM) and the data were expressed as polar vectors.
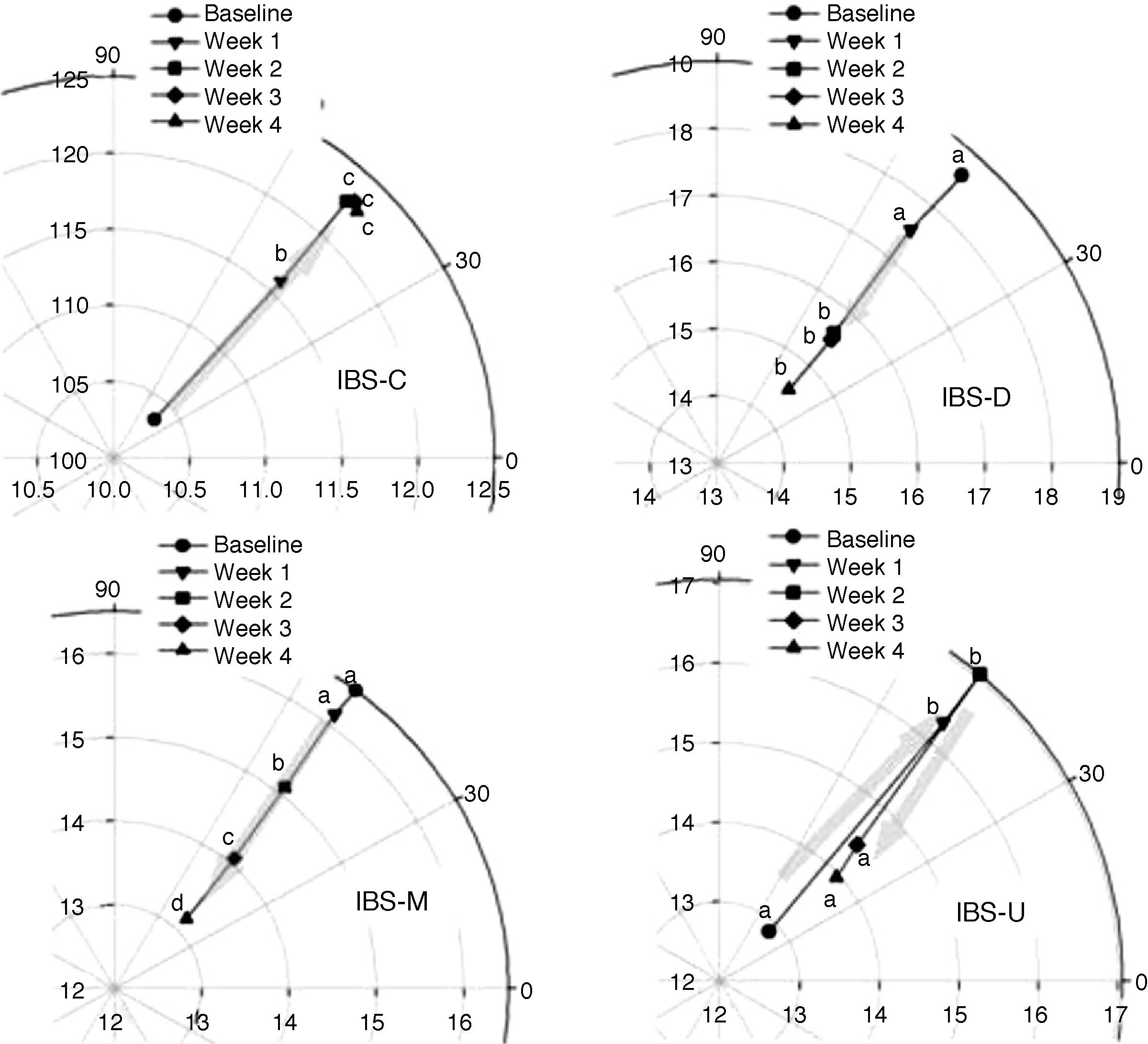
ResultsThe analysis showed a differential response to the PB+S treatment among the IBS subtypes: in reference to the IBS with constipation subtype, the magnitude of the vector increased from 10.2 to 12.5, reaching maximum improvement at two weeks of treatment (p<0.05, Scheffé). In the IBS with diarrhea and mixed IBS subtypes, the magnitude of the vector decreased from 19 to 14 (p<0.05) and from 16.5 to 13 (p<0.05), respectively, with continuous improvement for a period of four weeks. There was no definable vectorial pattern in the unsubtyped IBS group.
ConclusionsAnalysis with polar vectors enables treatment response to be measured in different IBS subtypes. All the groups showed improvement with PB+S, but each one had its own characteristic response in relation to vector magnitude and direction. The proposed method can be implemented in clinical studies to evaluate the efficacy of IBS treatments.
El Síndrome de Intestino Irritable (SII) es un trastorno caracterizado por dolor o malestar abdominal, asociado a cambios en el hábito intestinal. Actualmente no existe una variable objetiva para evaluar la eficacia de los tratamientos para este trastorno.
ObjetivoDeterminar la utilidad de un método de análisis con vectores polares para evaluar la eficacia de los tratamientos para el SII.
MétodosPara el análisis, se utilizaron los datos de un estudio clínico fase iv con 1,677 pacientes SII-Roma III, que recibieron bromuro de pinaverio 100mg+simeticona 300mg (BP+S) po bid por 4 semanas. Se registraron semanalmente la consistencia y la frecuencia de cada tipo de evacuación en una Matriz de Bristol (MB) y los datos se representaron como vectores polares.
ResultadosEl análisis mostró una respuesta diferencial de los subtipos de SII al BP+S: en SII-estreñimiento, la magnitud vectorial se incrementó de 10.2 a 12.5, alcanzando una mejoría máxima a las 2 semanas de tratamiento (p<0.05 prueba de Schefé). En SII-diarrea y SII-mixto, la magnitud del vector disminuyó de 19 a 14 (p<0.05) y de 16.5 a 13 (p<0.05), respectivamente, con mejoría continua durante las 4 semanas. En SII-no clasificable no existió un patrón vectorial definido.
ConclusionesEl análisis con vectores polares permite medir la respuesta a tratamiento en los diferentes subtipos del SII. Todos los subtipos mostraron mejoría con BP+S, pero cada uno respondió en forma característica en magnitud y dirección del vector. El método propuesto puede ser implementado en estudios clínicos para evaluar la eficacia de los tratamientos para el SII.
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by abdominal pain or discomfort associated with changes in bowel habit.1 Based on the predominant bowel habit, it is classified into subtypes that, in accordance with the most recent Rome III2 criteria, are IBS with diarrhea (IBS-D), constipation (IBS-C), mixed (IBS-M), and unsubtyped (IBS-U).2
In the absence of a biological marker in IBS, diagnosis is based on the Rome III1 clinical criteria that have been developed to classify functional gastrointestinal disorders (FGIDs)2; but there are no objective outcome measures for evaluating the efficacy of treatments for this disorder. Regulatory agencies have recently shown an interest in defining such objective outcome measures for the clinical trials that evaluate the medications presently being developed for IBS.3,4 The evaluation of pharmacologic efficacy must encompass several aspects, including the intensity of cardinal symptoms (abdominal pain and/or bloating) that can be evaluated with a visual analog scale (VAS), as well as changes in bowel habit (e.g. stool consistency that can be evaluated using the Bristol Stool Scale, or stool frequency that can be analyzed through symptom diaries).3
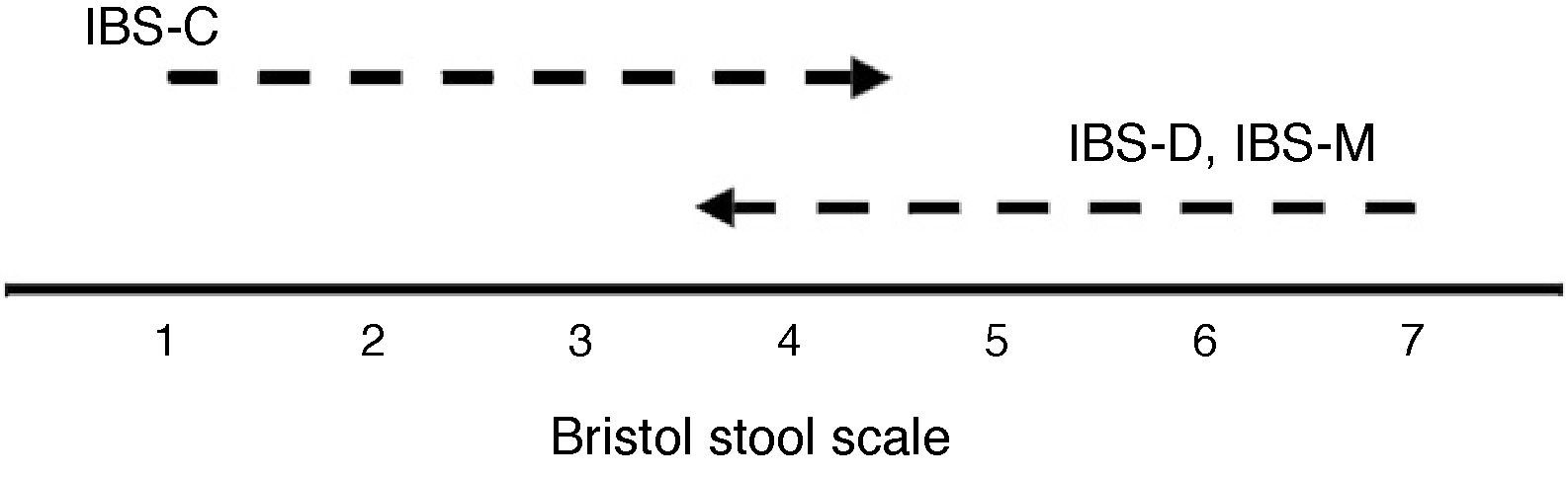
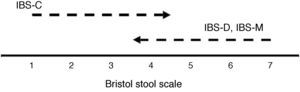
The Bristol Stool Scale has been recommended by the Rome III committee.1 It is a tool that enables bowel movements to be classified into seven categories, according to consistency: type 1, separate hard lumps, like nuts (hard to pass); type 2, sausage-shaped but lumpy; type 3, like a sausage but with cracks on the surface; type 4, like a sausage or snake, smooth and soft; type 5, soft blobs with clear-cut edges; type 6, fluffy pieces with ragged edges, a mushy stool; and type 7, watery, no solid pieces, entirely liquid.1 A matrixial table or Bristol Matrix (BM) can be constructed by simultaneously recording the changes in consistency using the Bristol Stool Scale and measuring evacuation frequency. This matrix integrates the two variables (omnibus variable) and can serve as an efficacy measure for evaluating pharmacologic treatments for IBS. Data from the BM can be graphed as a series of points or vectors in a two-dimensional space. In response to treatment effectiveness, improvement in stool frequency and consistency (type) recorded in the BM will be reflected as a movement of the vectors, and depending on the IBS subtype, this movement can be in the same or in opposite directions. For example, in patients with IBS-C, improvement means diminishing in evacuation consistency, going from a Bristol type 1 or 2 to a type 3 or higher, accompanied by increased evacuation frequency (moving from left to right, Fig. 1). In contrast, in patients with IBS-D, clinical improvement implies bowel movements of a greater consistency, going from types 6 and 7 to type 5 or lower, with a reduction in evacuation frequency. Once the magnitude and direction of the vectorial movement is known (the degree of improvement), vectors can be transfered to a plane of polar coordinates that enables the treatment response in all the IBS subtypes to be observed at the same time. This method of analysis is based on the assumption that things are more easily understood if they can be visualized.
The aim of this study was to determine the usefulness of the method of analysis employing polar vectors for evaluating IBS pharmacologic treatment efficacy. The data used were obtained in an open Phase IV study conducted on patients with active IBS who received 100mg of pinaverium bromide+300mg of simethicone (PB+S) po bid over a four-week period. The hypothesis stated that this method is adequate for evaluating the efficacy of any IBS treatment, by determining stool consistency and frequency improvement through a BM that allows for the treatment response in the various IBS subtypes (IBS-D, IBS-C, IBS-M, IBS-U) to be differentiated.
MethodsPopulationThe data used in this analysis were obtained from a Phase IV clinical study that included 1677 patients with active IBS in accordance with Rome III criteria. Patients were recruited by 1303 physicians with different specialties throughout the Mexican Republic. Selection criteria were:
- (a)
For inclusion – Patients of both sexes who were ≥18 and ≤50 years of age and who had a body mass index (BMI) <50. Clinical diagnosis of IBS according to the Rome III criteria: presenting with recurring abdominal pain or discomfort for at least three days a month in the last three months that was associated with 2 or more of the following characteristics: (1) improvement with defecation, (2) onset associated with a change in stool frequency, and (3) onset associated with a change in stool form (appearance). In addition, based on the Rome III classification, patients were categorized according to bowel habit as IBS-D, IBS-C, IBS-M, and IBS-U. IBS-D was identified by loose or liquid stools in at least 25% and hard or lumpy in less than 25% of bowel movements; IBS-C: hard or lumpy stools in at least 25% and loose or liquid in less than 25% of bowel movements; IBS-M: hard or lumpy stools in at least 25% and loose or watery stools in at least 25% of bowel movements; and IBS-U: modifications in stool consistency but insufficient to be classified as IBS-D, IBS-C, or IBS-M. Active IBS was defined as the presence of abdominal pain and/or discomfort at least twice a week during the previous seven days.
- (b)
For exclusion – The presence of alarm symptoms over the past 6 months, e.g.: involuntary weight loss, anorexia, inexplicable anemia, palpable lymph nodes or masses, fever, digestive tract bleeding, the suspicion or confirmed presence of malignant disease in any system or organ; women who were suspected of being pregnant, women who were pregnant, or who were breastfeeding; the suspicion or confirmed presence of rectoanal stricture; esophageal varices; a history of chronic nonspecific ulcerative colitis, Crohn's disease, or rectoanal ulcer; major upper or lower abdominal surgery; digestive tract malformation; or bowel obstruction.
An open, prospective, descriptive, and multicenter study was conducted. Treatment was PB+S for a period of four weeks. Stool consistency and frequency and improvement in cardinal symptom intensity (abdominal pain and bloating) were evaluated on a weekly basis.
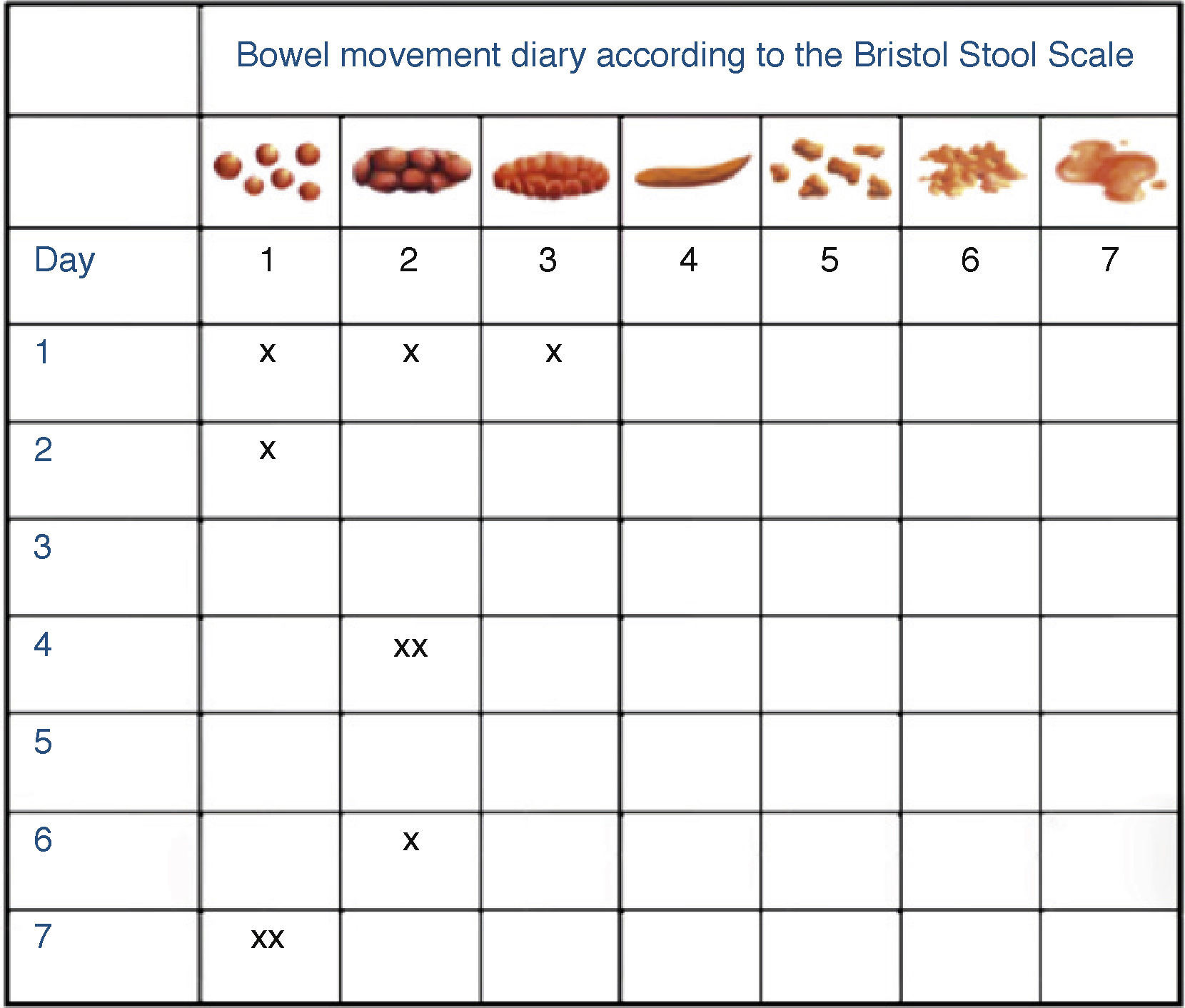
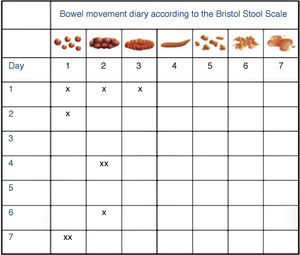
Data collection instrumentThe intensity of abdominal pain and bloating were evaluated by the patients through a 10-cm-long VAS for each symptom. Stool consistency (type) was recorded according to the Bristol Stool Scale on a 7-day format that also took into consideration the frequency of all types of bowel movements (Fig. 2). This format, or BM, was used during the four weeks of treatment. With the BM data, a vectorial calculation was made (see the statistical analysis) to evaluate the changes obtained with PB+S treatment.
Bowel movement frequency diary according to the Bristol Stool Scale types (BM). An example of the diary filled out by the patients is shown. Drawings of the different stool types according to the Bristol Stool Scale are at the top of the diary. The patients were instructed to identify the type of defecation and to mark the frequency of each type daily.
An omnibus variable was created that included two variables: consistency (type) and frequency of evacuations obtained from the BM. Given that the aim was to demonstrate the treatment changes through graphs, a two-dimensional configuration using polar vectors was decided upon. Polar vectors are dimensionless and can be evaluated based on their magnitude, and direction. A vector is a point in space (it can be multidimensional), that has a distance from its point of origin and can move in any direction. Its coordinates are simply the distance from the origin and the angle in relation to a horizontal plane.
The vector calculation was made in the conventional manner:
where r is the magnitude of the vector and y is the equivalent of the hypotenuse of a right triangle and therefore is equal to the square root of the sum of the weekly stool frequency (x), plus the total sum of the Bristol Stool Scale types the patient would have had (y), each one squared. The vectorial angle (which is equal to the direction of the vector) was calculated with the equation: θ=tan−1(y/x), in which tan−1 is the arc tangent of the coefficient of the numerator y (total sum of the Bristol types) and the denominator x (total weekly stool frequency). Thus, each patient had an r and θ value that could be lineally combined with the other subjects in order to obtain a mean (the expected value) vector magnitude according to each IBS-Rome III subtype. The vector was obtained in such a way that it represented the sum of the variables. In short, the higher the value of the Bristol type and the frequency of the bowel movements were, the greater was the magnitude of the vector. The maximum value of x was the result of: ∑i=1n=7xi=28, in a patient who would have shown all the Bristol types during the week. In contrast, the frequency of bowel movements during one week determined the maximum value of y. The weekly stool frequency in IBS patients was in the first percentile (P1) of 2 defecations, the P10 of 3 defecations, the median (P50) of 8 defecations, the P90 of 15, the P95 of 19, and the P99 of 28 defecations. In this manner, certain mathematical equivalences are produced that, even though they are not exact, can be useful for clinical interpretation.Data were expressed as mean and standard deviation (mean±SD), and standard error (SE) was specified when used. The differences in the means of magnitude and angles were calculated with ANOVA for repeated measures and post hoc comparisons were run with the Scheffé test, obtaining homogeneous groups.
Ethical aspectsThe Phase IV clinical study protocol that produced the data of this analysis was approved by the Ethics Committee of the Universidad de Guanajuato and the General Hospital of Naucalpan Dr. Maximiliano Ruiz Castañeda. The study was conducted in accordance with the Declaration of Helsinki,5 the Good Clinical Practice,6 and the local regulations concerning clinical research. All participating patients signed informed consents.
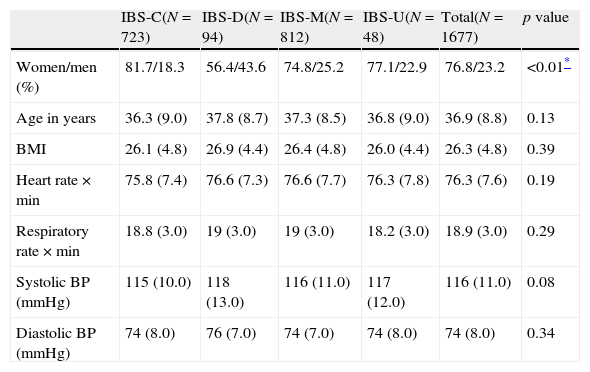
ResultsDemographic characteristics of the populationThe 1677 patients with active IBS included in the clinical study were classified according to IBS subtype as: IBS-C, 42.9%; IBS-D, 5.6%; IBS-M, 48.6%; and IBS-U, 2.9%. The total sample mean age was 36.9±8.8 years, BMI was 26.3±4.8, and 76.8% were women. The percentage of patients who stated that their IBS progression was longer than one year was 36.4%. Of the patient total, 1369 (81%) completed the four weeks of treatment with PB+S and attended their final visit. Table 1 shows the demographic and clinical characteristics of this subset, according to the IBS subtypes.
Patient clinical characteristics according to IBS subtype.
| IBS-C(N=723) | IBS-D(N=94) | IBS-M(N=812) | IBS-U(N=48) | Total(N=1677) | p value | |
| Women/men (%) | 81.7/18.3 | 56.4/43.6 | 74.8/25.2 | 77.1/22.9 | 76.8/23.2 | <0.01* |
| Age in years | 36.3 (9.0) | 37.8 (8.7) | 37.3 (8.5) | 36.8 (9.0) | 36.9 (8.8) | 0.13 |
| BMI | 26.1 (4.8) | 26.9 (4.4) | 26.4 (4.8) | 26.0 (4.4) | 26.3 (4.8) | 0.39 |
| Heart rate×min | 75.8 (7.4) | 76.6 (7.3) | 76.6 (7.7) | 76.3 (7.8) | 76.3 (7.6) | 0.19 |
| Respiratory rate×min | 18.8 (3.0) | 19 (3.0) | 19 (3.0) | 18.2 (3.0) | 18.9 (3.0) | 0.29 |
| Systolic BP (mmHg) | 115 (10.0) | 118 (13.0) | 116 (11.0) | 117 (12.0) | 116 (11.0) | 0.08 |
| Diastolic BP (mmHg) | 74 (8.0) | 76 (7.0) | 74 (7.0) | 74 (8.0) | 74 (8.0) | 0.34 |
BMI: body mass index; min: minutes; BP: blood pressure. Data expressed as mean (standard deviation).
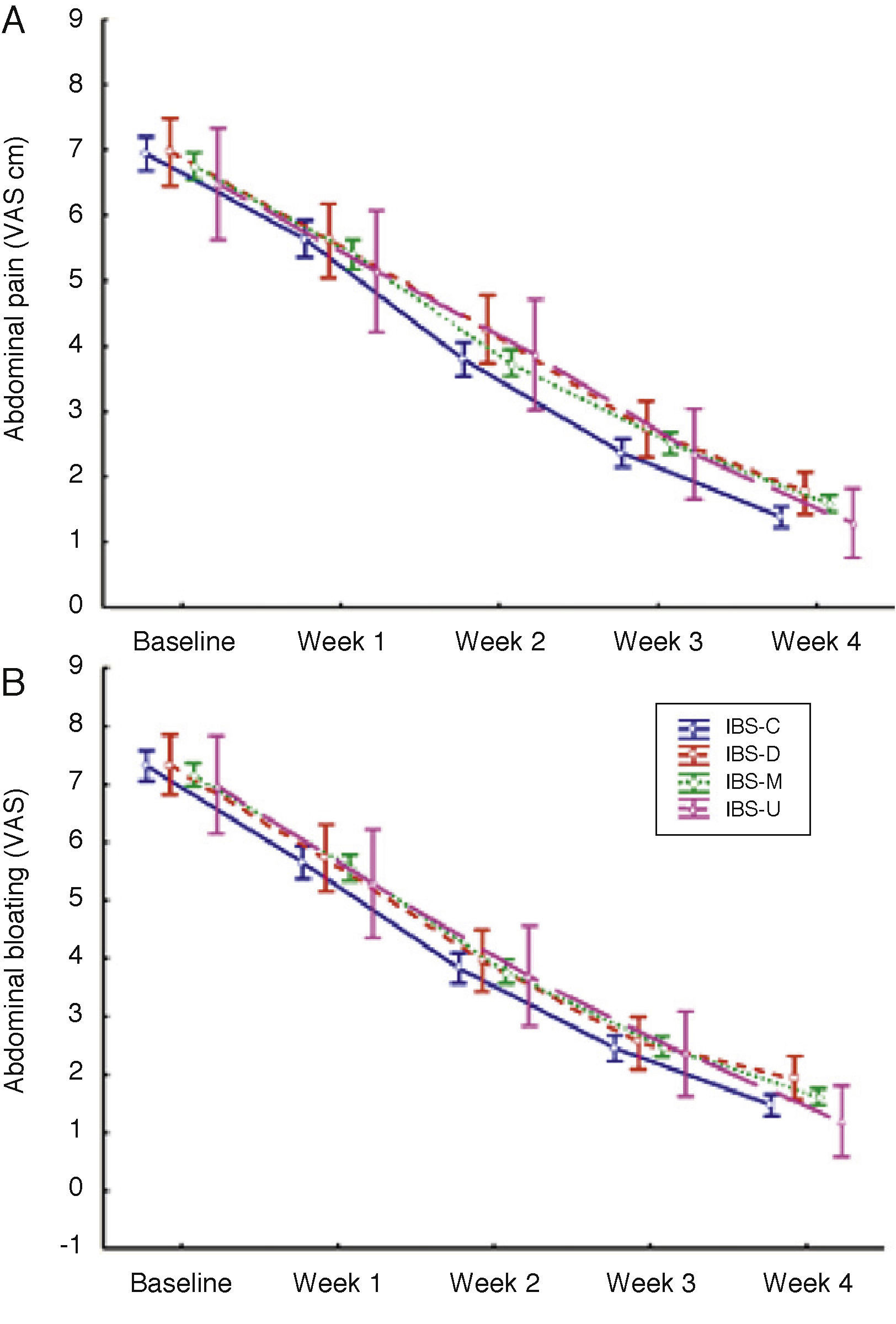
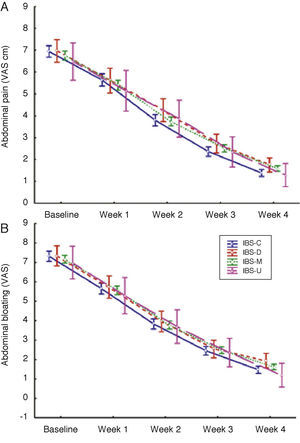
There was a notable reduction in the intensity of abdominal pain and bloating with the PB+S treatment, regardless of the IBS subtype. A plateau was not reached at four weeks, but there was maximum improvement in that time period (Fig. 3).
Changes in the intensity of abdominal pain and bloating. The intensity of abdominal pain and bloating was evaluated by the patients through a 10cm VAS. The changes in time were significant (p<0.001, repeated measures MANOVA) for pain (A) and bloating (B). The contrast between subtypes showed no significant difference. Blue: IBS-C, red: IBS-D, green: IBS-M, and pink: IBS-U. The figure shows means±SE.
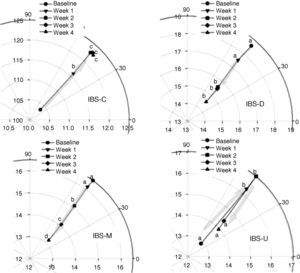
Polar vector analysis made it possible to show that there was considerable improvement in the IBS-C patients within the first two weeks of treatment and that it remained steady during the final two weeks. In this group there was an increase in vector magnitude from 10.2 to 12.5, reaching maximum improvement at two weeks of treatment (p<0.05, Scheffé). A vector magnitude of 12.5 is apparently equal to type 4 on the Bristol Stool Scale.
The magnitude of the vector was reduced in the patients with IBS-D and IBS-M. In the IBS-D patients the vector began at a magnitude of 19.0 and it went toward a magnitude of 14.0 (p<0.05), whereas the IBS-M group shared the same direction as the IBS-D group, starting at a magnitude of 16.5 and gradually moving toward a magnitude of 13.0 (p<0.05). There was important improvement in these two IBS subtypes during the second treatment week, and unlike the IBS-C group, it continued during weeks 3 and 4. The IBS-U group showed erratic behavior with no definite pattern in relation to vector magnitude and direction (Fig. 4).
Polar vectors showing the changes in magnitude (r) and direction, during four weeks of treatment with PB+S, according to each IBS subtype. Notice that the vectorial magnitude axes were adjusted according to the space covered during the four weeks and therefore, at its maximum improvement (r<12.5), IBS-C did not reach the lower end of IBS-M (r>13); in addition, considering the magnitude of the vector, there is overlapping in the IBS-D, IBS-M, and the IBS-U spaces. The letters correspond to homogeneous Scheffé groups in the post hoc analysis. See the statistical analysis section for details.
This study demonstrates that the transformation into polar vectors of the combination of the type of stool consistency according to Bristol Stool Scale, and the frequency of each of those stool types evaluated in a BM, is a useful method for evaluating IBS pharmacologic treatments, as it was the case with PB+S. This approach to evaluate efficacy does not include the changes in IBS cardinal symptoms, such as abdominal pain and bloating, because they can be evaluated through VAS.
Polar vector analysis clearly displayed the difference in treatment response in the various IBS subtypes, according to the predominant bowel habit. Even though all the subtypes responded positively to PB+S treatment, the response was different for each one. IBS-C showed a rapid symptom response within the first two weeks and then remained stationary, while improvement was progressive in IBS-D and IBS-M and continued to advance up to four weeks. According to the angle followed by the vectors on the polar coordinate plane (near 45°), bowel movement improvement was proportional in both consistency and frequency, without favoring either of the two variables. Upon graphing the polar vectors it became obvious that, despite the direction of the improvement of each IBS subtype, they all appeared to advance toward a common zone located between points 12.5 and 14, in relation to stool consistency and frequency; this zone could represent “normalcy” and such a finding needs to be verified in future studies.
A current limitation in the development of new IBS therapeutic options is the lack of validated outcome measures that objectively record their efficacy in clinical studies7; the fact that there are no biological markers for the diagnosis of IBS also has to be taken into account.8 In the last few years, the most widely used primary outcome measures in IBS clinical studies have been global variables of binary response: adequate improvement of abdominal pain and discomfort or satisfactory relief of IBS symptoms, that followed the Rome recommendations.9 Nevertheless, certain psychometric aspects of these variables have not been adequately validated and therefore are not presently accepted by the regulatory agencies.3 This has led to continuous meetings between the representatives of those agencies, experts on the subject matter, and representatives of the pharmaceutical industry,2 in an effort to define the reported outcome measures for the patients, the so-called PRO or Patient Reported Outcomes.2 This can be difficult when it entails evaluating the results in patients with FGIDs that do not have an organic or structural lesion and whose evaluation is made through symptom-based criteria.10,11
The method of analysis used in this study has taken the current tendencies and recommendations into account, such as including diagnosed patients through the Rome III criteria1 and evaluating the changes in stool consistency and frequency. In addition, it was based on the collection of symptoms through diaries and the weekly evaluation of treatment response. It also contemplated the variables in a multidimensional context and evaluated the individual response in the different IBS subtypes.3
A first limitation of the suggested method is the fact that the physician must graph the weekly vector results himself however, it is possible to develop computerized programs that can facilitate the follow-up of changes that occur in the patients and that can show the results of different treatments. A second limitation is that this method is applicable exclusively to medications that have an effect on stool consistency and frequency, and as a result, a third limitation is the fact that polar vectors do not evaluate the effect of treatment on abdominal pain or discomfort (abdominal bloating) that are key symptoms in IBS. However, it is worth noting that a recent review of the literature on questionnaires used in IBS to create a framework by which PRO can be developed for this disorder, established that abdominal pain and discomfort are two different symptoms. Therefore questions about discomfort response should be avoided, because it is very nonspecific.12 In the future, evaluations will have to be made on whether improvement in stool consistency and frequency not only reduces abdominal pain, but also other symptoms such as associated anxiety,13 and also whether the effect on pain and anxiety can be analyzed through vectors. A fourth limitation of this study is that the clinical significance of the change in vector magnitude and direction has not been determined. Regulatory agencies have emphasized the importance of identifying objective endpoints that would allow clinically significant improvement to be established, and thus report the percentage of patients that manage to go beyond that endpoint.2 Finally, the vectorial method was studied in patients who were seen in private medical practices in Mexico and it is necessary not only to validate the results in studies on open populations, but also on subjects from other cultures and in other languages.
In conclusion, polar vectors can be useful in clinical trials for the integral evaluation of the changes in stool consistency and frequency in response to an IBS treatment. Vectorial analysis shows that the combined therapy of PB+S, administered for at least four weeks, differentially modifies the frequency and consistency of bowel movements in all IBS subtypes, but with differences in the magnitude and velocity of the change between them. It should be pointed out that, even though the polar vectors analyzed in this study did not evaluate the response to pain and/or subjective abdominal bloating, the improvement of these symptoms analyzed through VAS was also significant for all the IBS subtypes. It is necessary to apply this method of analysis in placebo-controlled studies in order to confirm the results observed in this study.
Financial disclosureThis study was financed by Takeda México S.A. de C. V.
Conflict of interestsDr. Juan Carlos López-Alvarenga is currently a Biometric Scientist for Clinical Trials of Takeda México SA de CV. Has received research grants by Silanes, Roche, Servier. Has been a speaker for Takeda, Roemmers, Bayer, Roche and Novartis.
Dr. Sergio Sobrino-Cossío has been a speaker for Takeda México SA de CV, Astra, Ferrer, Olympus, Boston Scientific, Trasmédica, Wilson Cook.
Dr. José-María Remes-Troche is a member of the Advisory Borrad of Takeda Pharmaceuticals, Alfa-Wasserman and Janssen. Has been a speaker for Nycomed-Takeda, Advance Medical, Astra-Zeneca and Bristol-Myers-Squibb. Has received a research grant from Sanofi-Pasteur.
Dr. Jazmín Chiu-Ugalde and Dr. José Antonio Vargas-Romero, are employees of the Medical Direction of Takeda México SA de CV.
Dr. Max Schmulson has served as a consultant for Procter and Gamble, Novartis, Schering-Plough, Alfa-Wasserman, Janssen, Nestle Ltd and Almirall. Has been a speaker for Takeda México SA de CV, Schering-Plough, Mayoli-Spindler, Alfa-Wasserman, Janssen and Novartis. Has received research grants from Takeda México SA de CV and Nestle Ltd.