For the last 15 years, infection from Helicobacter pylori (H. pylori) has been recognized in gastritis pathogenesis, and is known to trigger an important inflammatory response in these patients.
AimTo determine the association between follicular gastritis and H. pylori infection in children seen at a public hospital in Peru.
MethodologyAn analytic, cross-sectional study was conducted on all the children treated at the Hospital Nacional Docente Madre “Niño San Bartolomé” in Lima, Peru, within the time frame of 2011-2012. All the personal data from the patients’ medical histories and endoscopic procedures were collected. The crude prevalence ratios (PR) were obtained and adjusted (aPR) with their 95% confidence intervals (95%CI), using generalized linear models with the binomial family and log link function.
ResultsA total of 123 children met the study criteria. Forty-eight (39%) of the study sample were girls and the mean age of the children was 12 years. H. pylori was present in 44% of the sample and 9% presented with more than 100 bacteria per field (classified as +++). Thirty-five percent of the children had esophagitis due to concomitant reflux. The presence of H. pylori was associated with follicular gastritis (P<0.01; aPR: 2.3; 95% CI:1.49-3.49), adjusted by the children's age.
ConclusionsBased on the data analyzed, it was concluded that the children with follicular gastritis had a greater likelihood of having H. pylori than those that did not present with gastritis. These results can be extrapolated to other similar populations and should be evaluated in each setting so that this does not become a public health problem within the next few years.
Durante los últimos 15 años la infección por Helicobacter pylori (Hp) ha sido reconocida en la patogénesis de la gastritis, desencadenando una importante respuesta inflamatoria.
ObjetivoDeterminar la asociación entre gastritis folicular y la infección de Hp en niños atendidos en un hospital público peruano.
MetodologíaEstudio transversal analítico desarrollado entre los años 2011 y 2012, con la totalidad de los niños atendidos en Hospital Nacional Docente Madre «Niño San Bartolomé», de Lima, Perú. Se recolectaron los datos personales de su historia clínica, datos del procedimiento endoscópico y sus hallazgos. Se obtuvieron las razones de prevalencia crudas y ajustadas (RPa) con sus intervalos de confianza del 95% (IC del 95%), usando los modelos lineales generalizados, con la familia binomial y la función de enlace log.
ResultadosParticiparon 123 niños que cumplían con los criterios del estudio, 48 (39%) fueron niñas y la mediana de edad fue 12 años. Presentó Hp el 44% de ellos y el 9% presentó más de 100 bacterias por campo (clasificados como 3 cruces). El 35% tuvo esofagitis por reflujo concomitante. La presencia de Hp estuvo asociada a la gastritis folicular (p<0.01; RPa: 2.3; IC del 95%, 1.49-3.49), ajustando por la edad de los niños.
ConclusionesSobre la base de los datos analizados se concluye que los niños con gastritis folicular tienen más probabilidad de tener Hp con respecto a los que no presentan gastritis. Los resultados pueden ser extrapolados a otras poblaciones similares, debiendo ser evaluado cada escenario para que esto no se convierta en un problema de salud pública en unos años.
Helicobacter pylori (H. pylori) is a spiral Gram-negative microorganism that has been reported worldwide. Approximately one out of every 2 persons of the world population is infected with H. pylori.1–4 For the last 15 years, H. pylori infection has been recognized in the pathogenesis of gastritis and peptic ulcer disease by triggering an important inflammatory response.5,6 The infection is acquired mainly in childhood and is associated with different gastrointestinal symptomatology, including recurrent abdominal pain, chronic hemorrhagic gastritis, and follicular gastritis, and it is sometimes asymptomatic.7–9Recent studies suggest that chronic follicular gastritis in childhood can increase the risk for developing gastric neoplasia in adult life.10 In our environment, different studies have been conducted on the histopathologic characteristics of gastritis from H. pylori,11 but whether there is a relation between that infection and its main characteristics, or if that relation exists in the pediatric population, has not been precisely determined.
Therefore, the aim of our work was to determine whether there was an association between follicular gastritis and H. pylori in children seen at a public hospital in the metropolitan area of Lima, Peru.
MethodsStudy design and populationEvaluating the anatomopathologic registers of the Hospital Nacional Docente Madre Niño San Bartolomé of all the children that underwent esophagogastroduodenoscopy requiring gastric biopsy or biopsy of some section of the gastrointestinal tract between the years 2011 and 2012, an analytic cross-sectional study was conducted on those patients that had the possibility of being affected by H. pylori. The patients seen at a different hospital, those that did not have a gastric biopsy, or those whose medical records were incomplete, were excluded from the study (23 patients). Non-probabilistic convenience sampling was carried out, calculating a minimum sample size of 97 patients utilizing a 10% expected error and 95% confidence interval.
Instruments and variablesA worksheet was designed that included the personal data from the medical history (age, sex) and data from the endoscopic procedure and it findings: year of evaluation, film number, sample location (esophagus, stomach and/or duodenum), and the anatomopathologic characteristics.
Chronic nonhemorrhagic gastritis was defined when there was gastritis with the presence of lymphoplasmacytic inflammatory infiltrate (also known as round cell infiltrate) in the gastric mucosa. Chronic hemorrhagic gastritis was defined with the appearance of multiple erythematous and/or predominantly superficial ulcers at the corpus and antrum, and even reaching the duodenum. Follicular gastritis was defined as such when there were lymphocytes forming complete nodules and follicles. Reflux esophagitis was defined according to the consensus of the American Gastroenterology Association, using the pathologic criterion of abundant eosinophils (≥ 15) predominantly in the superficial layer of the epithelium, as well as the possibility of basal cell hyperplasia and elongated papillas.12,13 The dependent variable was the presence of H. pylori. In order to be observed and to evaluate its damage to the mucosa, it was classified as absent if no bacteria were found in the observation field, it was described with a plus sign (+) if 1-20 bacteria per field were observed, two plus signs (++) if 21-100 bacteria per field were observed, and three plus signs (+++) if more than 100 bacteria per field were observed. This classification has been used by national and international authors for diagnosing H. pylori in different types of samples.14,15 This process of H. pylori identification was aided by the use of hematoxylin and eosin staining and then Giemsa and Warthin Starry stains for confirming the presence of H. pylori. The histochemical staining was processed at the hospital in which the study was conducted, following the technical recommendations, and they were used as markers for evaluating the presence of H. pylori.
ProceduresPermission was requested from the baseline coordinators to collect the data coinciding with the study period. After permission was granted, coordination meetings were held to define the variables and aims. The missing information of the patients included in the final baseline was searched for in the hospital's database. And finally, the baseline was created, carrying out data quality control and analyzing the spreadsheet. The baseline was generated using the Windows Excel 2010 program and the data were processed using the Stata version 11.1 statistics software (StataCorp LP, College Station, TX, USA).
Data analysisIn the descriptive analyses, the numerical variables were evaluated with the normality suppositions and then described through medians and interquartile ranges. The categorical variables were analyzed through percentages and frequencies. For the bivariate statistics, the Fisher's exact test was used for the cross-tabulation of the categorical variables and the rank sum test for the cross-tabulation of the categorical variables vs the quantitative ones, after the evaluation of the normality suppositions in each case. For the inferential statistics, generalized linear models were used, employing the binomial family and the log link function, obtaining the crude prevalence ratios and 95% confidence intervals (95% CI). The multivariate analysis was conducted in the same manner, obtaining the adjusted prevalence ratios (aPR). Statistical significance was set at a p < 0.05.
Ethical aspectsData confidentiality was maintained and the ethical recommendations of the international organizations were followed. The study protocol was approved by the ethics committee of the Hospital Nacional Docente Madre Niño San Bartolomé.
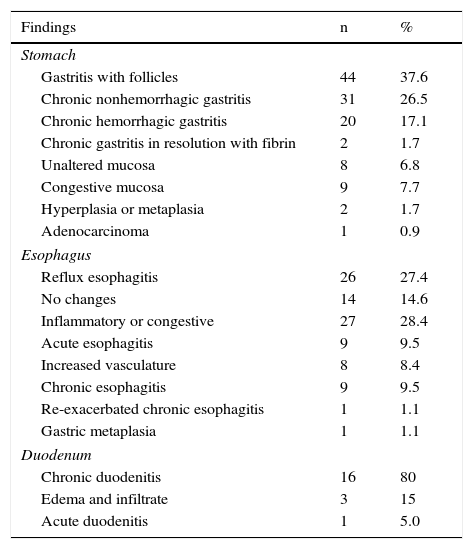
ResultsOne hundred twenty-three patients that fit the study criteria were included. Of that total, 48 (39.0%) were girls. The median age was 12 years and the interquartile range was 7-14 years. Likewise, 73 (59.4%) biopsies were performed in the stomach and esophagus, 24 (19.5%) only in the stomach, 15 (12.2%) in the stomach, esophagus, and duodenum, 6 (4.9%) only in the esophagus, and 5 (4.1%) in the stomach and duodenum, according to the criteria of the specialist. The histopathologic characteristics in relation to the finding site are shown in Table 1.
Histopathologic characteristics according to the finding site in children infected with Helicobacter pylori at a public hospital in Peru.
| Findings | n | % |
|---|---|---|
| Stomach | ||
| Gastritis with follicles | 44 | 37.6 |
| Chronic nonhemorrhagic gastritis | 31 | 26.5 |
| Chronic hemorrhagic gastritis | 20 | 17.1 |
| Chronic gastritis in resolution with fibrin | 2 | 1.7 |
| Unaltered mucosa | 8 | 6.8 |
| Congestive mucosa | 9 | 7.7 |
| Hyperplasia or metaplasia | 2 | 1.7 |
| Adenocarcinoma | 1 | 0.9 |
| Esophagus | ||
| Reflux esophagitis | 26 | 27.4 |
| No changes | 14 | 14.6 |
| Inflammatory or congestive | 27 | 28.4 |
| Acute esophagitis | 9 | 9.5 |
| Increased vasculature | 8 | 8.4 |
| Chronic esophagitis | 9 | 9.5 |
| Re-exacerbated chronic esophagitis | 1 | 1.1 |
| Gastric metaplasia | 1 | 1.1 |
| Duodenum | ||
| Chronic duodenitis | 16 | 80 |
| Edema and infiltrate | 3 | 15 |
| Acute duodenitis | 1 | 5.0 |
Of the patient total 43.9% (n=54) were diagnosed with H. pylori, and of those patients, infection in 50% (n=27) of them was catalogued as+(1-20 bacteria per field), in 41% (n=22) as++(21-100 bacteria per field), and in 9% (n=5) as+++ (> 100 bacteria per field).
The number of plus signs varied according to whether the patient had follicular gastritis or not. A total of 55.6% (n=15) of those patients that had one plus sign, did not present with follicular gastritis. In contrast, 81.8% (n=18) of those that had 2 plus signs presented with follicular gastritis. And finally, 40.0% (n=2) of the patients that had 3 plus signs presented with follicular gastritis, and the differences were statistically significant (p=0.02).
The mean age varied depending on the type of pathology. The median age of those that presented with follicular gastritis was 13 years (interquartile range: 9-16 years) vs a median of 11 years (interquartile range: 4-14 years) of those with no follicular gastritis diagnosis (p=0.01). Likewise, the median age of those patients with H. pylori infection was 13 years (interquartile range: 10-15 years) vs a median of 9 years (interquartile range: 4-14 years) of those with no H. pylori diagnosis (p < 0.01).
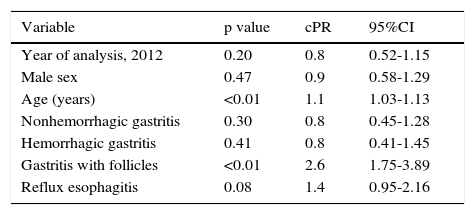
The bivariate analysis showed a statistically significant relation between age (p < 0.01) and follicular gastritis (p<0.01) with the presence of H. pylori in the children evaluated. The remaining results are shown in Table 2.
Bivariate analysis of the presence of Helicobacter pylori according to characteristics of children seen at a public hospital in Peru.
| Variable | p value | cPR | 95%CI |
|---|---|---|---|
| Year of analysis, 2012 | 0.20 | 0.8 | 0.52-1.15 |
| Male sex | 0.47 | 0.9 | 0.58-1.29 |
| Age (years) | <0.01 | 1.1 | 1.03-1.13 |
| Nonhemorrhagic gastritis | 0.30 | 0.8 | 0.45-1.28 |
| Hemorrhagic gastritis | 0.41 | 0.8 | 0.41-1.45 |
| Gastritis with follicles | <0.01 | 2.6 | 1.75-3.89 |
| Reflux esophagitis | 0.08 | 1.4 | 0.95-2.16 |
cPR: crude prevalence ratio obtained through generalized linear models (GLM), using the binomial family and the log link function.
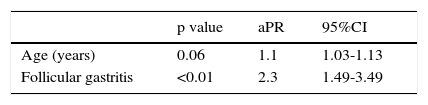
The multivariate analysis produced a statistically significant relation between follicular gastritis (p<0.01) and the presence of H. pylori - adjusted by the children's age. Table 3 shows the rest of the results.
Multivariate analysis of the presence of Helicobacter pylori according to characteristics of the children seen at a public hospital in Peru.
| p value | aPR | 95%CI | |
|---|---|---|---|
| Age (years) | 0.06 | 1.1 | 1.03-1.13 |
| Follicular gastritis | <0.01 | 2.3 | 1.49-3.49 |
aPR: adjusted prevalence ratio obtained through generalized linear models (GLM) using the binomial family and the log link function.
H. pylori infection has been studied from many perspectives, even though there is still much to discuss about this topic. However, there are clear concepts as to the anatomopathologic damage it can cause, but this has been studied very little in relation to childhood. It is known that a longer exposure time increases the risk for diseases caused by this pathology, and one of the factors to keep in mind - and the most important in our work - is its relation to gastritis.16,17 Patients with follicular gastritis were found to have a 2.3-fold greater frequency of H. pylori infection, compared with those that did not have follicular gastritis. These results coincide with those of a similar study carried out in 2012 reporting that chronic gastritis, active gastritis, and follicular gastritis are significantly higher in children infected with H. pylori.18 Another similar study conducted in Colombia showed that the patients with this type of gastritis had more intense and persistent dyspeptic symptoms. In addition, it stated that there was substantial improvement of those symptoms and the histologic findings in the gastric mucosa upon H. pylori erradication.19 This is due to the fact that H. pylori induces the production of proinflammatory substances by mononuclear cells. In this manner, substances such as interleukin 12 create a greater stimulus for a greater presence of Th1 lymphocytes, forming lymphoid follicles, but they are incapable of eliminating the bacterium.
Even though age was not statistically significant in our study, this could have been due to the small sample size, given that the p value was very close to 0.05. Some studies have shown that there is an association between older age and H. pylori infection. A study carried out in Portugal stated that older children can contract H. pylori infection at a rate similar to that of small children.20,21 Another study conducted in Colombia demonstrated that H. pylori infection progressively increased with patient age and was more notable after 6 years of age.22 In Peruvian studies, the mean age for acquiring the infection has changed from 12-18 months in 1990 to 2.4 years in 2002.23 This variable should be studied in future analyses, confirming whether it is an influential variable of the disease in our environment.
More than one fourth of the patients that presented with H. pylori also presented with reflux esophagitis. In a case-control study carried out in Brazil, it was found that reflux esophagitis was more frequent in children that did not have H. pylori, a result that differs from ours.24 This could be due to the fact that their study population was one made up exclusively of esophageal biopsies, whereas our study also included gastric and duodenal biopsies. Further investigation is needed to determine whether there are differences in relation to the anatomic area evaluated.
The large majority of patients presented with chronic duodenitis, a result concurring with those of studies conducted in Brazil and Uganda. They reported that H. pylori infection was a risk factor for presenting with duodenal infections, especially if it was associated with Giardia lamblia.25–27 One out of every 10 patients presented with H. pylori infection described with 3 plus signs, meaning that those children had more than 100 bacteria per field. Similar studies in Vietnam concurred that large numbers of H. pylori infection are associated with childhood.28 Nevertheless, the quantity found in our study is alarming. This is due to the fact that we are a so-called Third World country, in which the prevalence of H. pylori infection is greater in the low economic population. H. pylori is also strongly associated with inadequate sanitary conditions in the developing countries.
And finally, a recent study stated that the diagnostic tests for defining treatment should be invasive (histology, antibiogram), leaving the noninvasive tests, as well as test/treatment, for epidemiologic or treatment confirmation studies, thus preventing unnecessary treatments and reducing strain resistance. Those children presenting with association with peptic ulcer disease should receive treatment adapted in accordance with sensitivity tests and lasting a recommended 10-14 days. Treatment costs, adherence, and possible adverse effects should be taken into account. A confirmation test, such as the breath test, is also recommended 4-8 weeks after treatment has ended.29
A limitation of our study was selection bias, produced by not having an adequate sample, but even so, the data can be considered as an approximate reality value, given that they come from a referral hospital that treats a large number of children from the Peruvian capital. Moreover, there are no other studies in our environment that analytically assess the association between follicular gastritis and H. pylori, making ours an important starting point for future research on this topic. We recommend that further studies be conducted at more healthcare centers to evaluate aspects that were not analyzed in our study, as well as to determine whether age really is an influential factor in H. pylori infection.
Based on the data analyzed we conclude that pediatric patients with H. pylori infection have a higher frequency of follicular gastritis compared with those with non-H. pylori gastritis.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureSelf-financed.
Conflict of interestThe authors declare that there is no conflict of interest.
This article was prepared as part of the activities of the second Research Group of the SOCEM, offered in conjunction with the Medical Association of Research and Health Services. This manuscript was prepared by Claudia Vera, fulfilling the participation requirements of the second GIS, Lima, Peru.
Please cite this article as: Mejia CR, Vera CA, Huiza-Espinoza L. Asociación entre gastritis folicular y Helicobacter pylori en niños atendidos en un hospital público peruano. Revista de Gastroenterología de México. 2016;82:80–85.