Radiotherapy forms part of the treatment for neoplasia,1 and an estimated 50% of cancer patients will receive this therapy during their treatment.2 The harmful effect of ionizing radiation can be experienced long after the primary disease for which it was indicated has been resolved. In the gastrointestinal tract, it can damage the small bowel, resulting in what is known as «radiation enteritis», which can cause bowel obstruction. When it affects the colon it is called «radiation colitis» and «radiation proctitis» when it involves the rectum.3
We present herein the case of a patient with bowel obstruction secondary to radiation enteritis that developed years after her treatment for cervical cancer; our aim is to increase awareness of the fact that this disease should be suspected in patients that have undergone radiation.
A 48-year-old woman had an 8-month history of chronic, colicky abdominal pain. In the mornings her abdomen was soft and pain free, but as the day progressed she felt bloated and had abdominal pain. She did not complain of vomiting and her bowel movements were normal. The patient stated that she had presented with cervical cancer 4 years earlier and received radiotherapy. She later underwent a total hysterectomy that resulted in disease remission. The physical examination revealed a soft, nondistended abdomen. No masses or organomegaly were palpated, peristalsis was present, and there were no signs of peritoneal irritation. A colonoscopy was done to rule out rectosigmoid pathology, finding images consistent with radiation proctopathy and no evidence of stricture. The patient was released after the study and only given topical treatment with mesalazine in suppositories. Twenty-four hours after the colonoscopy, she went to the emergency department due to intense colicky pain and abdominal distension. Plain abdominal and chest x-rays were ordered because there was a suspicion of a possible perforation during the colonoscopy.
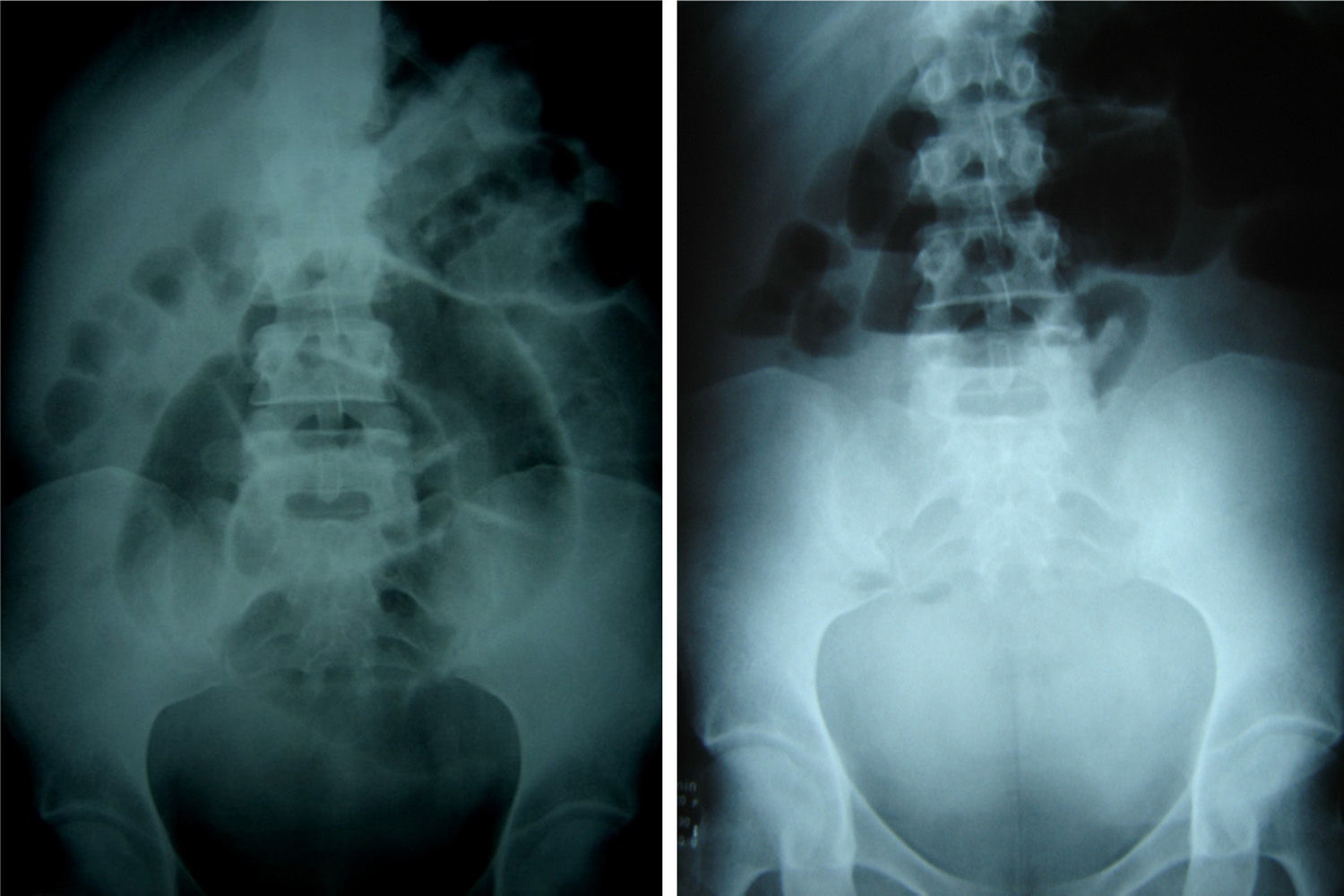
The chest x-ray showed no evidence of free subdiaphragmatic air and the abdominal film displayed the presence of very dilated, centralized small bowel segments and air-fluid levels (fig. 1). Conservative management with nasogastric decompression was begun, after which a water-soluble contrast study was carried out; a narrowing at the region of the ileum was identified, along with persistent segment distension. The laboratory work-up reported: Hb 16.0g/dl, leukocytes 8,600 x mm3, segmented neutrophils 68%, bands 2%, platelets 405,000, glucose 80mg/dl, urea 27mg/dl, and creatinine 0.7mg/dl.
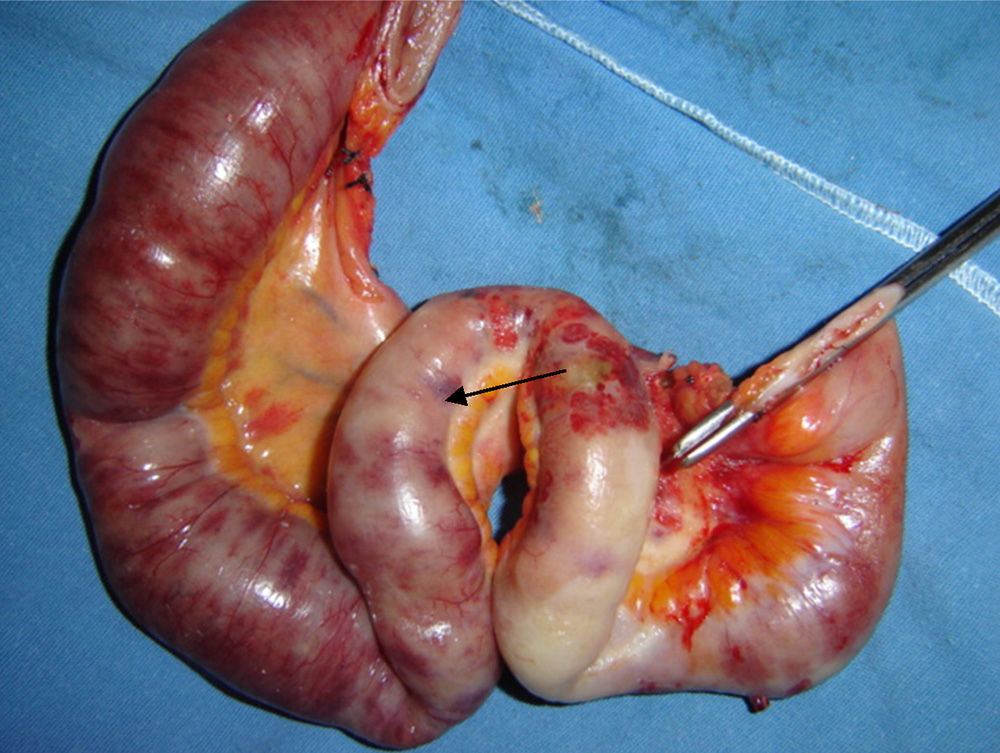
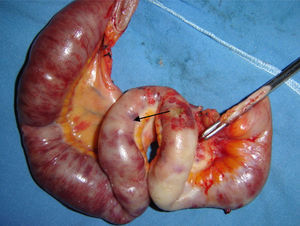
The patient did not improve, so an exploratory laparotomy was performed, revealing, at 20cm from the ileocecal valve, a zone of the terminal ileum of approximately 30cm in length that had a firm consistency and was edematous, with clear signs of ischemia, whitish, with areas of serous necrosis, and an obvious reduction in the size of the intestinal lumen (fig. 2). Given the situation, the affected segment was resected and distal closure and terminal ileostomy were carried out. The patient had adequate progression and was released from the hospital on the third postoperative day. The surgical specimen study reported changes due to radiation enteritis. Bowel reconnection with a right hemicolectomy and a latero-lateral ileotransverse anastomosis were performed 4 months later.
Radiation enteritis is a complication that is secondary to the use of radiotherapy in the treatment of pelvic tumors, more frequently affecting the small bowel (primarily the ileum) and the colon.4
The acute phase of radiation exposure lasts for hours or days with vomiting and diarrhea and is generally self-limited after the radiotherapy is finished.1 The appearance of the chronic phase can vary and is estimated to occur mainly during the first 5 years, but there have been reports of its presentation spanning from 2 months to up to 25 years after radiotherapy. 5–6
Incidence and severity depend on the dose of radiotherapy, the size of the lesion to be radiated, treatment frequency, the type of radiation, and the length of follow-up.1–3 Risk factors include age, smoking, previous surgery, pre-existing pelvic inflammatory disease, and joint chemotherapy administration.1,7 An established determining factor in cell response to radiation is the stage of the cell cycle; the G2 and M phases are the periods that are most sensitive to radiation.2,8 Radiotherapy affects all the layers of the intestinal wall, but the damage is more severe in the mucosa, due to its rapid cell proliferation that induces a rupture in the cell cycle with the subsequent atrophy of the villi, acute inflammation, and fibrosis.9 Progressive obliterating vasculitis induces ischemia through vascular thrombosis with intestinal wall fibrosis and necrosis.2,8,10
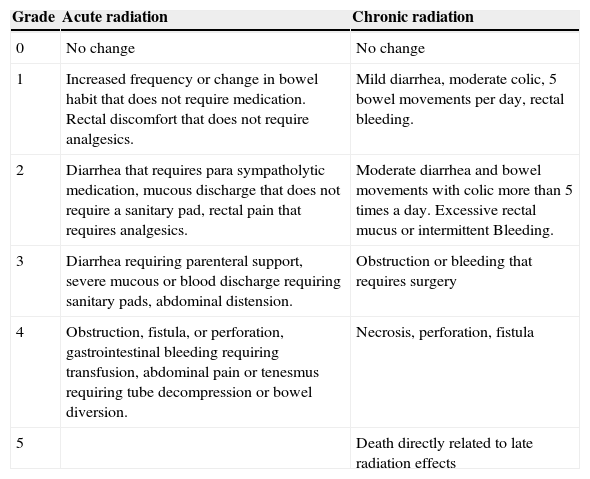
Only 20% of the patients are referred for gastroenterologic evaluation because symptoms are either underestimated or not recognized.3 The Radiotherapy Oncology Group of Philadelphia has proposed a way to stage lesion grade (Table 1).
Scoring criteria for acute and chronic radiation morbidity.
| Grade | Acute radiation | Chronic radiation |
|---|---|---|
| 0 | No change | No change |
| 1 | Increased frequency or change in bowel habit that does not require medication. Rectal discomfort that does not require analgesics. | Mild diarrhea, moderate colic, 5 bowel movements per day, rectal bleeding. |
| 2 | Diarrhea that requires para sympatholytic medication, mucous discharge that does not require a sanitary pad, rectal pain that requires analgesics. | Moderate diarrhea and bowel movements with colic more than 5 times a day. Excessive rectal mucus or intermittent Bleeding. |
| 3 | Diarrhea requiring parenteral support, severe mucous or blood discharge requiring sanitary pads, abdominal distension. | Obstruction or bleeding that requires surgery |
| 4 | Obstruction, fistula, or perforation, gastrointestinal bleeding requiring transfusion, abdominal pain or tenesmus requiring tube decompression or bowel diversion. | Necrosis, perforation, fistula |
| 5 | Death directly related to late radiation effects |
Taken from Turina et al.1 Reproduction authorized by the Radiotherapy Oncology Group (RTOG).
Radiation enteritis should initially be managed conservatively, but surgery is indicated when complications present.4 Some of the conservative treatment modalities of intestinal lesions due to radiation are the administration of topical anti-inflammatory agents, such as mesalazine or steroids (budesonide), glutamine, or the endoscopic application of formalin (in the large bowel) when there is bleeding.1,10
And finally, surgery should be evaluated in patients with complications from chronic radiation enteritis, given that it is related to a high morbidity rate, prolonged hospital stay, and the possibility of reoperation.10
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Martínez Hernández Magro P. Oclusión intestinal secundaria a enteritis por radiación. Reporte de caso. Revista de Gastroenterología de México. 2015;80:111–113.