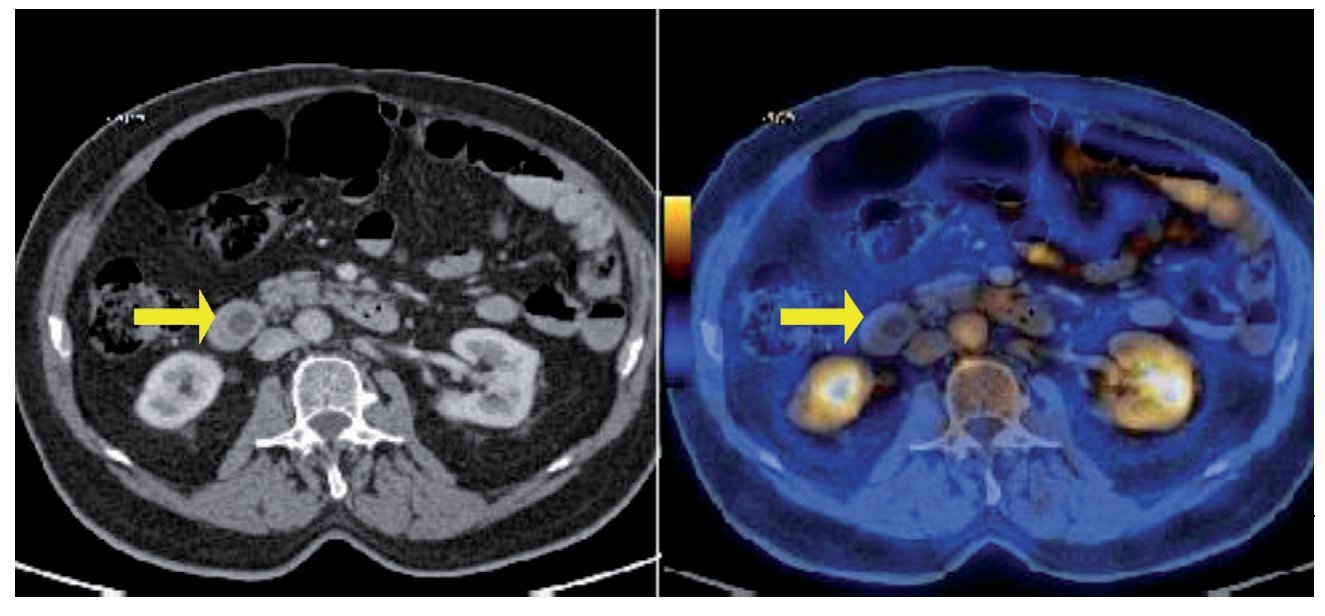
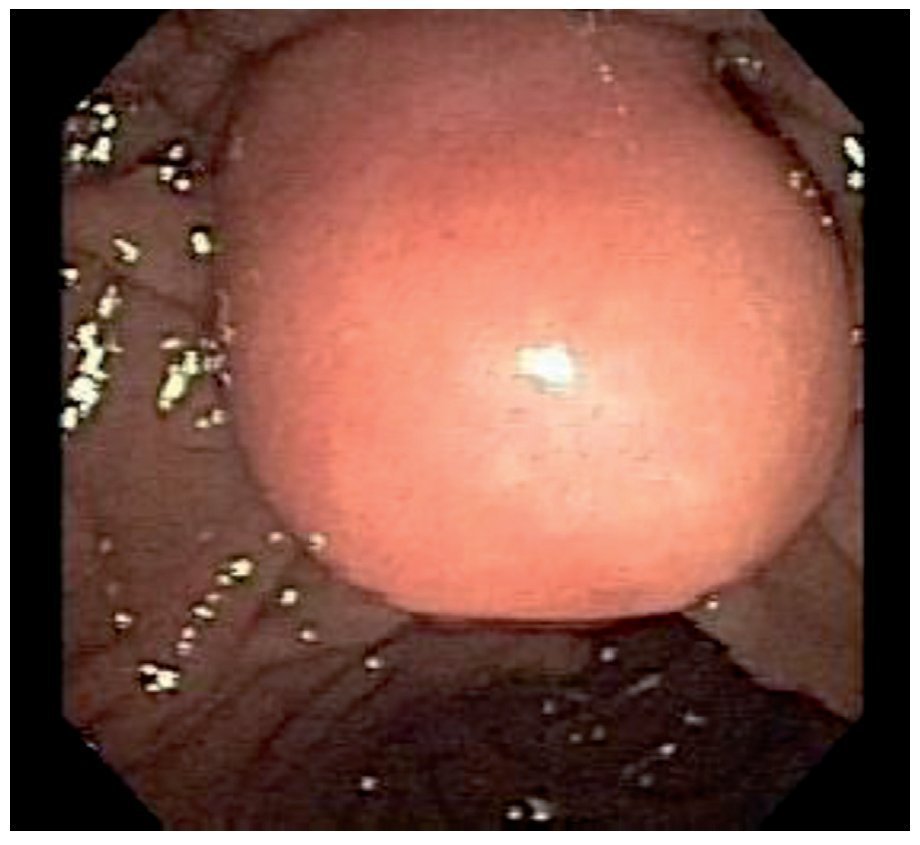
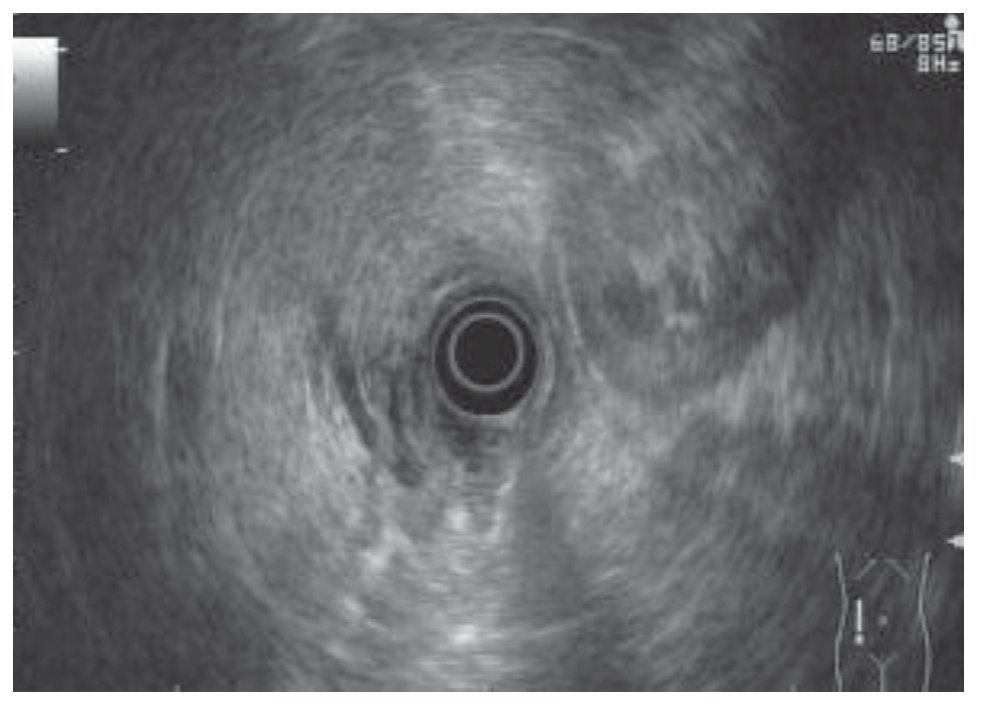
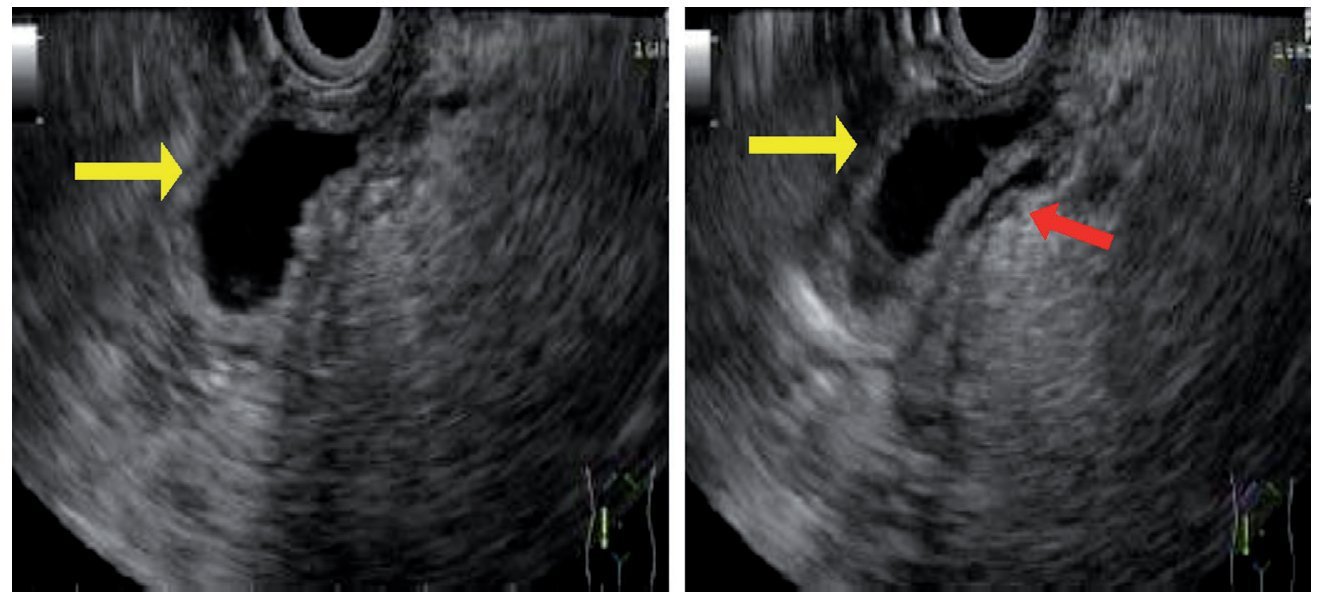
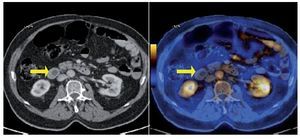
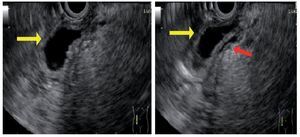
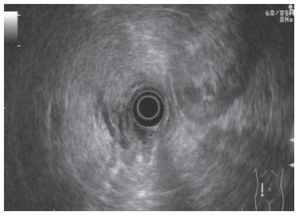
A 77-year-old man had a past medical history of cancer of the prostate and colon for which he underwent prostatectomy and right hemicolectomy, respectively, 5 years before, with no coadjuvant treatment. A follow-up positron emission tomography-computed tomography (PET-CT) scan was carried out to evaluate tumor recurrence. The patient was asymptomatic, physical examination was unremarkable, and tumor markers showed no alterations. Dilatation of the common bile duct from its point of origin to its outlet (12.4 to 13.9 mm) was identified in the PET-CT scan, with no apparent tumor activity (Fig. 1). Based on these findings, cholangiopancreatography by magnetic resonance was done. Dilatation of the intra and extrahepatic biliary tract, as well as the main pancreatic duct, was identified but its etiology could not be defined and so a biliary-pancreatic endoscopic ultrasound (EUS) study was performed. Endoscopic vision in the second portion of the duodenum revealed a bulging ampulla of Vater with normal mucosa and a spontaneous exit of bile (Fig. 2). During the endosonography, intra and extrahepatic biliary tract dilatation was observed and the common bile duct was 11 mm in diameter. There was a 14 mm saccular dilatation at the level of the ampulla of Vater of anechoic content. The echostructure of the walls was conserved, consistent with choledochocele (Figs. 3 and 4). No abnormalities were observed in the diameter and along the course of the main pancreatic duct.
Figure 1. Positron emission tomography-computed tomography (PET/CT) scan.
Figure 2. Endoscopic ultrasound, endoscopic vision.
Figure 3. Endoscopic ultrasound (EUS) image.
Figure 4. Endoscopic ultrasound (EUS) image.
Choledochocele, a variant of the bile duct cysts, is a cystic dilatation of the common bile duct within the duodenal wall. It makes up 3 to 4% of all bile duct cysts. In 1977, Todani et al. classified 5 types of bile duct cysts. Type 1 (75 to 85%) refers to a dilatation of the extrahepatic bile ducts. Type 2 (3 to 4%) forms a saccular diverticulum in the common bile duct. Type 3 corresponds to a choledochocele. Type 4 (10 to 40%) refers to the presence of multiple cysts (type 4A is characterized by intra and extrahepatic bile duct cysts and type 4B by multiple cysts exclusively in the extrahepatic biliary tract). Type 5 cysts (< 1%) affect the intrahepatic bile ducts, and are generally multiple (Caroli disease). Four anatomic types of choledochocele were defined by Sarris and Tsang: A1, the common bile duct and the duct of Wirsung have a common opening into the cyst; A2, the common bile duct and the duct of Wirsung have separate openings into the cyst; A3, similar to A2, but with a cyst, especially an intramural one, that protrudes slightly into the duodenum and is usually collapsed. Finally, in the choledochocele subtype B, the opening of the papilla is normal and the cyst is very protruding and only communicates with the common bile duct. Choledochocele is usually suspected first through computerized tomography data. Cholangiopancreatography through magnetic resonance is the ideal method for a noninvasive imaging study; however, when it is not available, as was the case with our patient, EUS is a precise diagnostic imaging modality with an overall sensitivity of 86%. Choledochocele diagnosis through EUS can be established by revealing an anechoic, protruding lesion covered with intact mucosa directly adjacent to the papilla of Vater and showing a communication between this lesion and the common bile duct. EUS should be done on patients with a dilated biliary tract whose cause cannot be demonstrated by other imaging methods. Choledochoceles are rare and their approach is transduodenal. Endoscopic sphincterotomy can be the treatment for some patients that present with smaller cysts and no duodenal obstruction; in the rest of the cases there should be transduodenal extirpation with sphincteroplasty or duct reimplantation.
Financial disclosure
No financial support was received in relation to this article.
Conflict of interests
The authors declare that there is no conflict of interest.
* Corresponding author at:
Unidad de Endoscopia Avanzada, Centro Médico ABC.
Observatorio, Sur 136, Número 116, Colonia Las Américas, Mexico City.
Tel.: +5272 49-19.
E-mail address:carlossalceda@yahoo.com (J.C. Salceda-Otero).