Eosinophilic cholecystitis is a rare entity that was first described in 1949 and is clinically indistinguishable from calculous cholecystitis. Histologically, there is transmural inflammatory infiltration of the gallbladder wall, more than 90% of which is composed of eosinophils. The aim of the present article was to review the prevalence of eosinophilic cholecystitis and analyze the clinical and surgical characteristics of patients diagnosed with the disease that were operated on at our hospital.
Materials and methodsA retrospective study was conducted on patients that underwent cholecystectomy and whose postoperative histopathologic diagnosis was eosinophilic cholecystitis, within the time frame of January 2000 and August 2014. The demographic, clinical, paraclinical, surgical, and histopathologic variables were described.
ResultsOver a period of 14 years, a total of 7,494 patients underwent cholecystectomy. Of those patients, 12 had a postoperative histologic diagnosis of eosinophilic cholecystitis. Mean patient age for disease presentation was 39 years (±11 years), and female sex was predominant, with 7 cases. All the patients had concomitant gallstones and 10 patients presented with acute cholecystitis that required urgent cholecystectomy. All the cases were considered idiopathic. We found a prevalence of 0.16%, corresponding to 1 case for every 625 cholecystectomies performed at our hospital.
ConclusionWe found a low prevalence of eosinophilic cholecystitis (0.16%) in our study population. The clinical manifestations were similar to those of calculous cholecystitis. Cholecystectomy is adequate treatment in patients with idiopathic disease.
La colecistitis eosinofílica es una entidad rara que se describió por primera vez en 1949 y es clínicamente indistinguible de la colecistitis litiásica. Histológicamente, hay infiltración inflamatoria transmural de la pared de la vesícula biliar con más del 90% de eosinófilos. El objetivo del presente trabajo es revisar la prevalencia y analizar las características clínico-quirúrgicas de los pacientes con diagnóstico de colecistitis eosinofílica operados en nuestro hospital.
Materiales y métodosSe trata de un estudio retrospectivo (de enero del 2000 a agosto del 2014) en el que se incluyeron pacientes postoperados de colecistectomía con diagnóstico histopatológico de colecistitis eosinofílica. Se describen variables demográficas, clínicas, paraclínicas, quirúrgicas e histopatológicas.
ResultadosSe encontraron un total de 7,494 pacientes postoperados de colecistectomía en un período de 14 años, de los cuales 12 pacientes tuvieron el diagnóstico postoperatorio histopatológico de colecistitis eosinofílica. La edad media de presentación fue de 39 años (±11 años), y predominó el sexo femenino con 7 casos. Todos los pacientes tenían colelitiasis concomitante y 10 de ellos se presentaron con colecistitis aguda, que requirió colecistectomía de urgencia. Todos los casos se consideraron idiopáticos. Encontramos una prevalencia del 0.16%, que corresponde a un caso por cada 625 colecistectomías llevadas a cabo en nuestra institución.
ConclusiónEncontramos una prevalencia baja de colecistitis eosinofílica (0.16%) en nuestra población de estudio. Las manifestaciones clínicas se asemejan a las que se presentan en colecistitis litiásica. La colecistectomía es el tratamiento adecuado en pacientes con esta entidad de etiología idiopática.
Eosinophilic cholecystitis (EC) is a rare entity that was first described in 1949 and is clinically indistinguishable from calculous cholecystitis.1–3 Histologically, there is transmural inflammatory infiltration of the gallbladder, 90% of which is composed of eosinophils. Diagnosis of acute cholecystitis is currently made through the clinical history, ultrasound findings, and physical examination (the Tokyo criteria).4,5 Some common characteristics in patients diagnosed with EC or acute cholecystitis are: a positive Murphy sign, pain in the right upper abdominal quadrant, and systemic manifestations of inflammation.5
There are numerous reports of CE in the literature, but its incidence is low and disease etiology is unknown and not widely studied. An association of EC with hypersensitivity to antibiotics, the use of alternative herbal medicine, parasitic infections, autoimmune diseases, and a relation between eosinophilic gastroenteritis and eosinophilic pancreatitis has been suggested in studies.3,6–8
The treatment of choice for EC is cholecystectomy and its results are generally favorable.9–11 When EC is secondary to another pathology, each underlying disease should be specifically treated.10
The aim of the present study was to review the prevalence of EC in patients diagnosed with that disease and operated on at our hospital and analyze their clinical and surgical characteristics.
Materials and methodsA retrospective, cross-sectional, descriptive study was conducted that included all patients with a histopathologic diagnosis of EC that underwent cholecystectomy at the Hospital General “Dr. Manuel Gea González” in Mexico City. The case records of patients that had undergone cholecystectomy over a 14-year period from January 2000 to August 2014 were retrieved from the hospital database. The study was approved by the hospital's ethics and research committee.
The variables analyzed were divided into general demographic variables (age, sex, and comorbidities), preoperative clinical and paraclinical variables (the Murphy sign, total leukocytes, eosinophils, abdominal ultrasound results), and postoperative variables (histopathologic diagnosis, complications, and mortality). Patients with incomplete case records were excluded from the study.
Statistical analysisThe data were captured and stored in a database (Microsoft Excel® 2010). The variables were analyzed through descriptive statistics. EC prevalence in our study population was calculated and the results were plotted on a graph. The SPSS Statistics Version 20.0 software (IBM Corp, Armonk, NY, USA) was employed to perform the statistical analysis.
ResultsOver a 14-year period, 7,494 patients underwent cholecystectomy. Twelve of those patients had the postoperative, histopathologic diagnosis of EC and met the histopathologic criteria for diagnosis, defined as an inflammatory infiltrate composed of more than 90% eosinophils. None of those 12 patients were excluded or eliminated from the study.
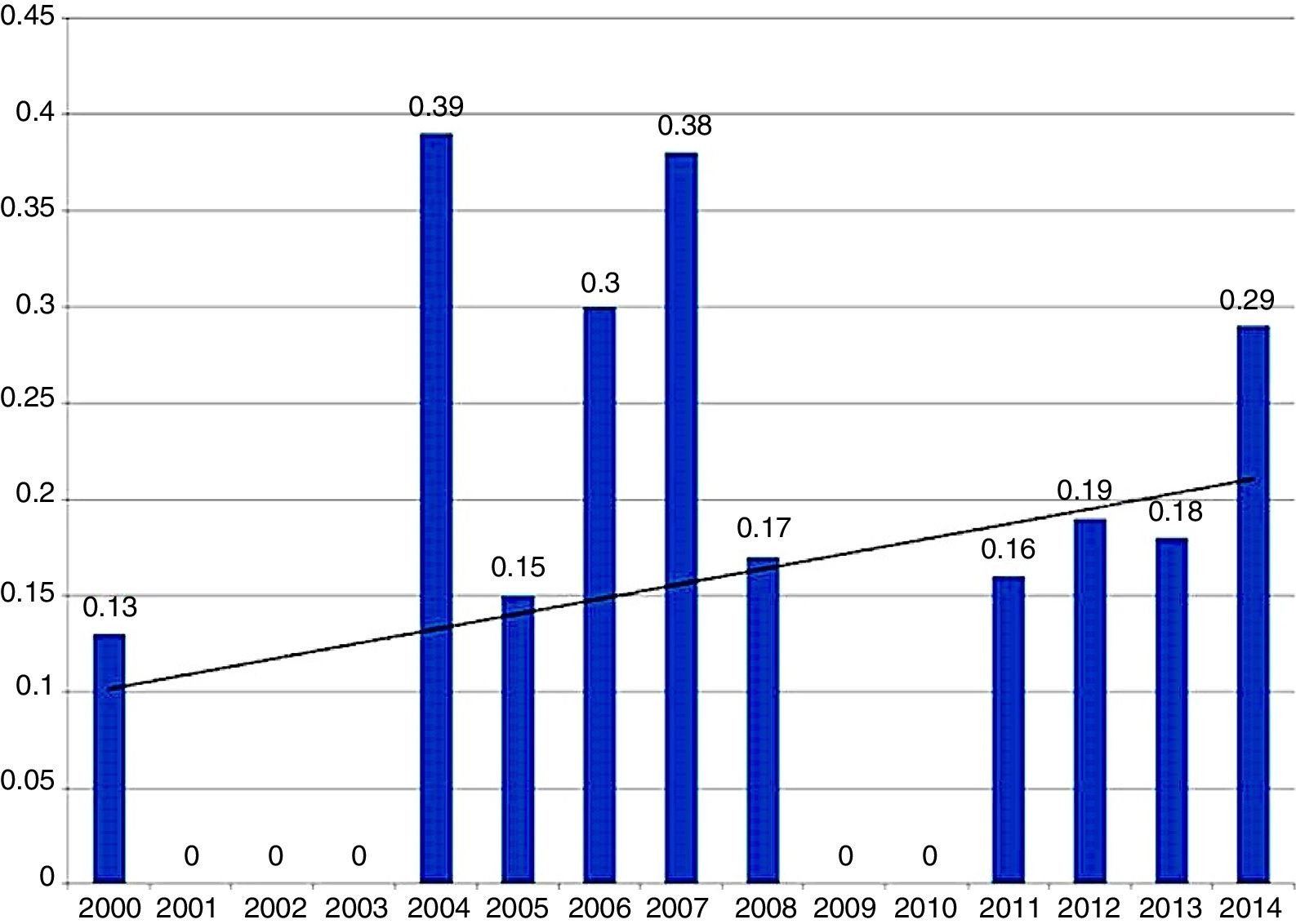
We found a disease prevalence of 0.16%, corresponding to one case of EC for every 625 laparoscopic cholecystectomies performed at our hospital (fig. 1).
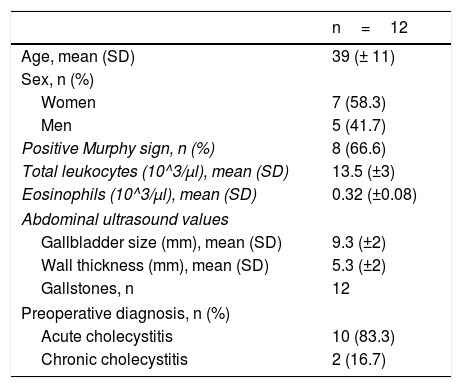
Of the 12 patients, 7 were women and 5 were men (Table 1). The mean patient age at disease presentation was 39 years (± 11). Three female patients, 44, 64, and 49 years of age, had a history of kidney stones that required nephrectomy, dyslipidemia under treatment with pravastatin, and multiple transfusions, respectively. The rest of the patients had no pathologic history.
Characteristics of the patients diagnosed with eosinophilic cholecystitis after laparoscopic cholecystectomy.
| n=12 | |
|---|---|
| Age, mean (SD) | 39 (± 11) |
| Sex, n (%) | |
| Women | 7 (58.3) |
| Men | 5 (41.7) |
| Positive Murphy sign, n (%) | 8 (66.6) |
| Total leukocytes (10^3/μl), mean (SD) | 13.5 (±3) |
| Eosinophils (10^3/μl), mean (SD) | 0.32 (±0.08) |
| Abdominal ultrasound values | |
| Gallbladder size (mm), mean (SD) | 9.3 (±2) |
| Wall thickness (mm), mean (SD) | 5.3 (±2) |
| Gallstones, n | 12 |
| Preoperative diagnosis, n (%) | |
| Acute cholecystitis | 10 (83.3) |
| Chronic cholecystitis | 2 (16.7) |
SD: Standard deviation
Ten of the 12 patients were admitted to the emergency room of the hospital due to acute abdominal pain. The other 2 patients had a history of recurring episodes of biliary colic and were admitted to the hospital for elective cholecystectomy. The 10 patients that came to the emergency room presented with abdominal pain one to 7 days prior to their emergency room admission. Eight patients had a positive Murphy sign and leukocytosis (with no eosinophilia).
Gallstones were identified in all the patients through abdominal ultrasound imaging. The gallbladder was enlarged in 9 (75%) patients (mean of 9.44cm, SD: 1.21), with thickening of the wall (mean of 5.84mm, SD: 1.58).
Ten patients were admitted to the hospital with the diagnosis of acute calculous cholecystitis and 2 patients with chronic calculous cholecystitis. Cholecystectomy was performed on the 12 patients, with no postoperative complications recorded. Hospital stay was between 24 and 48h.
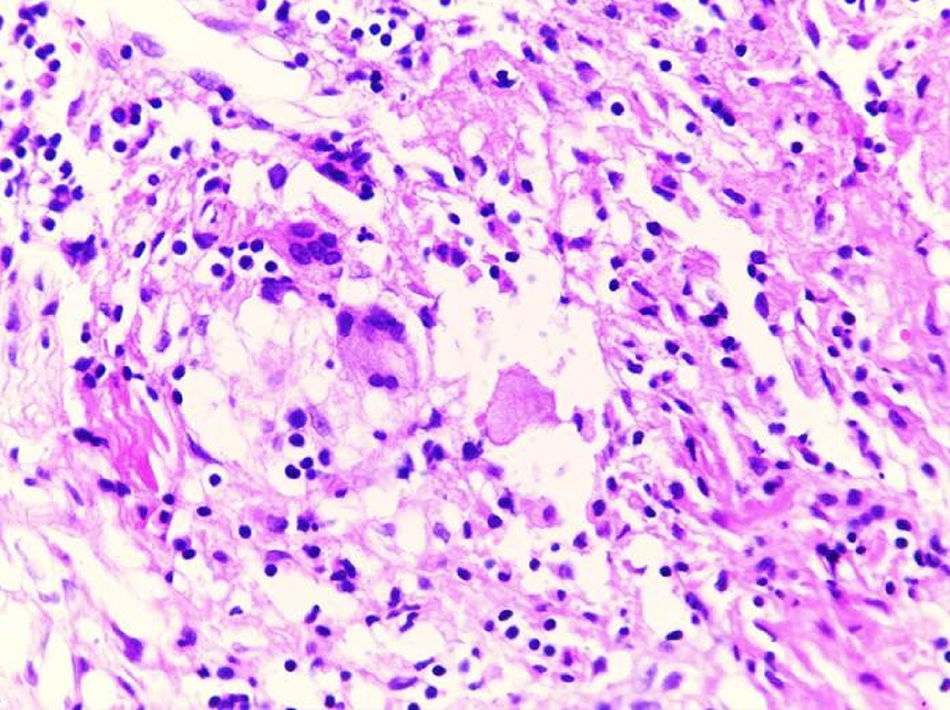
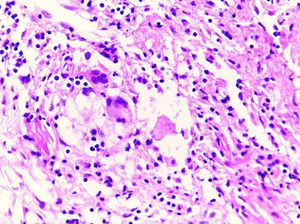
The histopathologic result in all the patients was: EC with concomitant gallstones. Two cases also presented with transmural necrosis, thickening of the wall due to fibrosis, and cholesterolosis (fig. 2). The inflammatory infiltrate composed of eosinophils was limited to the gallbladder wall in all the cases and there was no sign of extension to the cystic duct.
None of the 12 patients presented with hypereosinophilia in their initial studies, nor did they have clinical data comparable with parasitosis or any hypereosinophilic syndrome. All the diagnoses were reported by the pathology service in the postoperative follow-up. The 12 patients had a thorough clinical check-up during their outpatient follow-up. The most frequent pathologies and risk factors were ruled out (parasitic disease, hypereosinophilia, herbal medicine or alternative medicine use, medications taken). Given the absence of risk factors or underlying pathologies, all the cases were catalogued as having idiopathic etiology. There were no postoperative complications and no disease-associated deaths were reported at the one-year follow-up in any of the patients.
Discussion and conclusionsGallstone disease is the main cause worldwide of cholecystitis and biliary colic. It has a prevalence in the population of 11 to 35%, of which 1-4% of the cases will develop biliary colic and 20% will present with acute cholecystitis. However, many cases of acute cholecystitis (acalculous) are due to other factors: ischemia, motility disorders, infections (bacterial and parasitic), collagen disorders, allergic reactions, etc.12,13 It should be mentioned that EC is 3 times more frequent in patients with acalculous cholecystitis than in patients with gallstone disease,14 differing from the results in our patients.
As stated above, EC is a rare and little-studied disease of the gallbladder. Its frequency is reported at below 1% in the majority of case series on cholecystectomy.4 In our study, prevalence was 0.16%, similar to that reported in other analyses.4,11,15
EC is an inflammatory pathology in which eosinophils predominate in the infiltrate (> 90%). Cases in which the eosinophilic composition of the infiltrate is less than 90% are known as lymphoeosinophilic cholecystitis or cholecystitis with a mixed infiltrate.4,14–16
Eosinophilic infiltration (< 90%) into the gallbladder is not an uncommon finding. In that context, the inflammatory infiltrates are mixed, meaning they additionally contain other types of cell strains.15,16 Previous studies have reported the presence of eosinophils in 22% of gallbladders (48 out of 217 patients). In a British study that included 625 cholecystectomies, eosinophilic infiltrates were found in 16 gallbladders,17 but the majority did not have more than 50% eosinophils, and only 3 of the 16 infiltrates were composed purely of eosinophils (> 90%).
EC etiology has been associated with multiple pathophysiologic processes, but the cause of the disease has not been precisely defined. It has been associated with: parasitic diseases, allergies, drugs and herbal medicine, myalgia-eosinophilia syndrome, Crohn's disease, and sarcoidosis, to name a few.4,16
Hypereosinophilic syndrome (with the invasion of eosinophils into various systemic organs) contrasts with the limited invasion of eosinophils into the gastrointestinal system (eosinophilic gastroenteritis) and invasion that only includes the biliary tract and/or the gallbladder (eosinophilic cholangiopathy). EC can be found in those 3 contexts. Some studies point to a local immunologic reaction due to an antigen in the bile.4
The database searches (MEDLINE/PubMed, Google Scholar) with the Spanish and English search terms “colecistitis eosinofílica” and “eosinophilic cholecystitis” produced a majority of case reports.
The most recent report found (2016) was that by Mehanna et al.15 They described a case of eosinophilic cholecystitis associated with bile duct stricture in a 36-year-old woman. The patient had a history of massive pulmonary thromboembolism, repeated episodes of abdominal pain, and previous treatment with mebendazole, due to the suspicion of Toxocara canis. She required laparoscopic cholecystectomy, choledocotomy, and a T stent, as well as treatment with steroids.
In 2015, Del Moral et al.4 reported on the case of a 24-year-old woman, with an unremarkable past medical history, who was diagnosed with acute acalculous cholecystitis and required laparoscopic cholecystectomy. The histopathologic study reported a transmural eosinophilic infiltrate.
In 2002, Adusumilli et al.7 described the case of a 35-year-old man with a history of asthma, who presented with pain in the right hypochondrium and with peripheral eosinophilia. Laparoscopic cholecystectomy with liver biopsy was performed. The histopathologic finding was transmural eosinophilic infiltration. The patient had a past medical history of taking herbal supplements with L-tryptophan to enhance muscle anabolism.
Kaji et al.18 reported on the case of a 28-year-old woman with acute eosinophilic cholecystitis and pericarditis, with peripheral eosinophilia and high titers of antibodies against Ascaris lumbricoides. She only required treatment with albendazole. Kim et al.1 described 2 cases of EC associated with Clonorchis sinensis.
There are review articles, such as the one in which Shakov et al.11 found a total of 24 case reports of EC since 1949. The mean age of those 24 patients was 39.3 years (17-65), half of the sample was women, and EC was associated with gallstone disease in 6 of the patients. The majority of subjects in those case reports (15 out of 24) were Korean. Mean age and sex distribution were similar to those of our study, but all of our patients had concomitant gallstone disease.
Diagnosis is postoperative in the majority of the cases because patients present with nonspecific clinical and imaging study results that are similar to those of acute calculous cholecystitis.11,15–17
An important association in patients with EC is the presence of peripheral eosinophilia.11 Most of patients in our study had leukocytosis, but a predominance of peripheral eosinophils was not documented. Peripheral eosinophilia has been found more frequently in hypereosinophilic syndromes or when there are parasitic diseases.
The imaging studies of ultrasound and tomography identify cholecystitis data, such as wall thickening, gallbladder distension, perivesicular fluid, and on occasion, stones.16 All the patients in our study had gallstone disease and the majority presented with vesicular distension and wall thickening.
Cholecystectomy is the treatment for EC.15–17 The pathology is clinically indistinguishable from the clinical symptoms of acute cholecystitis due to other more frequent causes. When some other underlying cause is identified, it should be treated in a specific manner: with antiparasitic agents or steroids (hypereosinophilic syndrome or eosinophilic cholangitis). Laparoscopic cholecystectomy was the only treatment of the disease required in our study population.
In conclusion, we found a low prevalence of EC (0.16%) in our study population, which was similar to the low frequency reported worldwide. The clinical presentation in those patients resembles the clinical symptoms of calculous cholecystitis. Cholecystectomy is adequate treatment for the patients with primary or idiopathic eosinophilic cholecystitis, whereas patients in whom the disease is secondary to another pathology should receive treatment in accordance with the underlying disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank the entire surgical team at the Hospital General “Dr. Manuel Gea González”.
Please cite this article as: Gutiérrez-Moreno LI, Trejo-Avila ME, Díaz-Flores A, Dávila-Zenteno MR, Montoya-Fuentes IM, Cárdenas-Lailson LE. Colecistitis eosinofílica: estudio retrospectivo de 14 años. Revista de Gastroenterología de México. 2018;83:405–409.