Post-fundoplication dysphagia is resolved with no therapeutic intervention in the majority of cases but it can persist in 5.3% of children that undergo the procedure. Among the differential diagnoses, esophagogastric junction outflow obstruction (EGJOO) is a disorder that should be suspected if there is a persistence of dysphagia. The aim of our study was to describe the clinical characteristics, treatment, and follow-up in a case series of patients diagnosed with post-fundoplication EGJOO.
Materials and methodsThe clinical records of patients diagnosed with EGJOO at a tertiary care hospital within the time frame of September 2015 to September 2019 were reviewed, with respect to manometry, etiology, treatment, and clinical course of the disease.
ResultsOf the 213 high-resolution esophageal manometries performed, 4 patients met the criteria for post-fundoplication EGJOO. The primary symptom was dysphagia, presenting 15 days after the procedure. Esophageal dilations were carried out on all the patients but with no improvement. Symptoms related to the condition resolved spontaneously in three of the four patients.
ConclusionThe management of children with post-fundoplication EGJOO continues to be a challenge. Even though more than half of the cases resolve with no intervention, optimum management of the motility disorder is still limited, given the scant experience with the condition in the pediatric population.
La disfagia postfunduplicatura en la mayoría de los casos se resuelve sin intervención terapéutica, sin embargo, en algunas ocasiones esta puede persistir en 5.3% de los niños sometidos a este procedimiento. Dentro de los diagnósticos diferenciales, la obstrucción al tracto de salida de la unión esofagogástrica (OTSUEG) es un trastorno que se debe sospechar ante la persistencia de la disfagia. El objetivo de este estudio es describir las características clínicas, tratamiento y seguimiento de una serie de pacientes con diagnóstico de OTSUEG postfunduplicatura.
Material y métodosSe llevo a cabo la revisión de los expedientes clínicos con diagnóstico de OTSUEG en un hospital de tercer nivel durante el periodo de septiembre 2015 a septiembre 2019. En todos ellos se revisó la manometría, sintomatología, etiología, tratamiento y el curso clínico de la enfermedad.
ResultadosDel total de 213 manometrías esofágicas de alta resolución realizadas, 4 pacientes cumplían con los criterios de OTSUEG postfunduplicatura. El síntoma principal fue la disfagia, presentándose 15 días posteriores al procedimiento. En todos los pacientes se realizaron dilataciones esofágicas, con pobre respuesta al tratamiento tras procedimiento. Los síntomas relacionados con la condición se resolvieron en 3/4 de los pacientes de manera espontánea.
ConclusiónEl manejo de niños con OTSUEG postfunduplicatura continúa siendo un desafío, ya que, si bien mas de la mitad de ellos resuelven sin intervención alguna, aun existen limitaciones para definir un manejo óptimo de este trastorno de la motilidad dada la poca experiencia que existe en la población pediátrica.
Dysphagia is a frequent complication in patients that undergo fundoplication, and according to some authors, can present in up to 76% of cases, normally resolving within the first postoperative weeks. Dysphagia after said procedure is reported to present in adults at two years in 7.5% of cases and at five years in 5%.1 In the pediatric patient, severe persistent dysphagia can occur in 5.3% of cases.2 According to Sobrino-Cossio et al.,1 post-fundoplication dysphagia may be due to an undiagnosed pre-existing condition, such as insufficiently effective esophageal motility, esophageal aperistalsis, etcetera, or to a structural or functional alteration, such as the currently well-described esophagogastric junction outflow obstruction (EGJOO).
EGJOO is a motility disorder that generally presents as a consequence of fundoplication, and according to the Chicago v3.0 classification (CC V3.0), is defined as an elevated integrated relaxation pressure (IRP) with a conserved peristalsis pattern, thus not meeting the criteria for achalasia.3 Some authors refer to it as an early or incomplete manifestation of achalasia4–6 and others have associated it with mechanical disorders, such as eosinophilic esophagitis, hiatal hernia, stricture, Schatzki rings, tumors, or structural alterations derived from fundoplication or bariatric surgery. Therefore, those diagnostic possibilities should always be ruled out, and not be classified as a functional problem.7–11
Clinical presentation is varied and dependent on the cause. Dysphagia is the most common symptom in up to 57% of cases.8 Diagnosis is made through manometry (preferably high-resolution manometry). Likewise, imaging studies, such as esophagram, can be useful, as well as upper gastrointestinal endoscopy and transendoscopic ultrasound.7,8
Different studies report that up to 52% of patients have spontaneous symptom resolution, with no need for specific treatment.4
At present, there are no studies reporting the progression and treatment of pediatric patients with EJGOO. The aim of our study was to objectively describe the clinical and manometric characteristics, as well as the possibility of treatment, in children with that disorder.
Materials and methodsDesignA retrospective observational study was conducted that included all the patients referred to the Physiology and Motility Unit of the Gastroenterology and Pediatric Nutrition Department of the Instituto Nacional de Pediatría (Mexico City, Mexico). The data were collected from the clinical records of the patients that underwent high-resolution esophageal manometry (HREM), within the time frame of September 2015 and September 2019. The following aspects in the patients that met the criteria for EGJOO diagnosis, according to the Chicago 3.0 classification, were analyzed: a) etiology, b) upper gastrointestinal endoscopy, c) esophagram, d) treatment, and e) clinical progression of symptoms. Demographic information was also obtained and the associated symptomatology of dysphagia, chest pain, regurgitation, and gastroesophageal reflux was analyzed. All the study patients presented with dysphagia one or more months after having undergone fundoplication. Patients with neuromuscular diseases were excluded.
Study procedureIn all the children that had HREM, a 4.2 mm probe (Sandhill Scientific Inc., Highland Ranch, Colorado, USA) with 36 sensors separated by 1 cm intervals was used to identify the topographic pressures of the esophagus and sphincters. In all cases, an eight-hour fast was indicated, along with the suspension of all medications that could influence results, three days prior to the study. After calibrating the equipment and verifying its correct functioning, the HREM probe was placed transnasally, with the patient in the supine position. The distal end was positioned, observing the high-pressure zone in the lower esophageal sphincter (LES) and adjusted 2-3 cm above the diaphragm in the patients, when possible. Once an adequate position was corroborated, calibration of the reference points was performed for a minimum of 60 seconds, and 10 swallows of 5 mL of saline solution at 30-second intervals were then registered. The analysis and interpretation of the results were carried out according to the CC V3.0 classification. EGJOO was defined when the HREM revealed an IRP above 15 mmHg with conserved esophageal peristalsis, and the achalasia criteria according to the Chicago classification were not met.
Statistical analysisData processing and analysis were conducted utilizing the SPSS version 22.0 program. Central tendency tests, frequency distributions, and dispersion measures were applied for the univariate analysis. The distribution of simple frequencies and their percentages were applied to the qualitative variables of sex, esophageal symptoms, reflux symptoms, comorbidities, treatment, symptom resolution, and alterations in the esophagram and endoscopy. Central tendency (mean, median, mode) and dispersion measures (standard deviation) were applied to the quantitative variable of age. The graphs and tables were constructed using the Excel® 2013 program and the information was later transferred to Microsoft Word® 2013.
Ethical considerationsThe authors declare that all procedures followed conformed with the ethics regulations of the research and ethics committee of the Instituto Nacional de Pediatría, in accordance with the Declaration of Helsinki. The present research was approved by the institutional retrospective study committee.
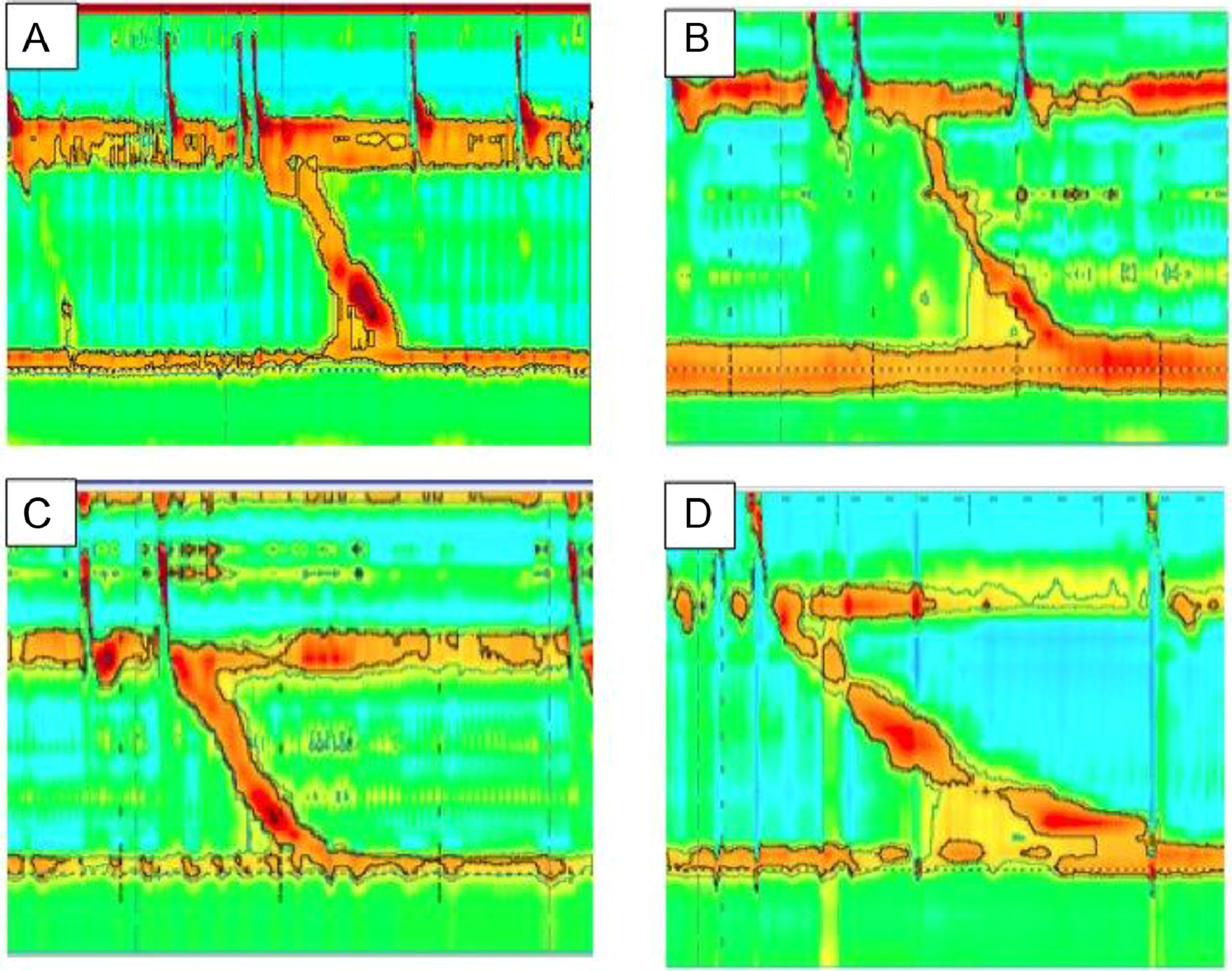
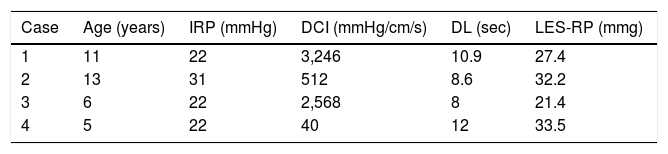
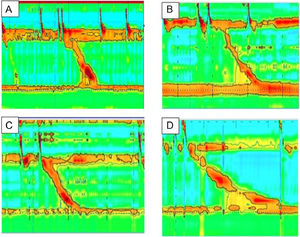
ResultsOf the total of 213 HREMs carried out within the period of September 2015 to September 2019 at the Physiology and Motility Unit of the Gastroenterology Service of the Instituto Nacional de Pediatría, four fit the diagnosis of EGJOO (CC v3.0), with a mean IRP of 24 (24.25 ± 3.90 mmHg) (Table 1) (Fig. 1A-D). Within that time frame, 143 fundoplications were performed by the pediatric surgery service. Nissen fundoplication was performed in three patients and one patient underwent Toupet fundoplication. All the fundoplications were open surgeries.
Manometric findings in children with esophagogastric junction outflow obstruction.
| Case | Age (years) | IRP (mmHg) | DCI (mmHg/cm/s) | DL (sec) | LES-RP (mmg) |
|---|---|---|---|---|---|
| 1 | 11 | 22 | 3,246 | 10.9 | 27.4 |
| 2 | 13 | 31 | 512 | 8.6 | 32.2 |
| 3 | 6 | 22 | 2,568 | 8 | 21.4 |
| 4 | 5 | 22 | 40 | 12 | 33.5 |
DCI: distal contractile integral; DL: distal latency; IRP: integrated relaxation pressure; LES-RP: lower esophageal sphincter resting pressure.
Esophageal manometry of the patients with esophagogastric junction outflow obstruction.
Patients with a history of post-fundoplication dysphagia. High-resolution manometry was consistent with esopgagogastric junction outflow obstruction. Mean relaxation pressure was 24 mmHg, peristalsis was normal in all cases.
Three of the study patients had a history of chronic pneumopathy and regurgitation symptoms. Given the persistence of the respiratory and digestive symptomatology, they underwent fundoplication. The fourth study patient underwent fundoplication during left diaphragmatic hernia correction. Mean patient age at diagnosis was 8 ± 3.3 years, and 3 of the patients were males.
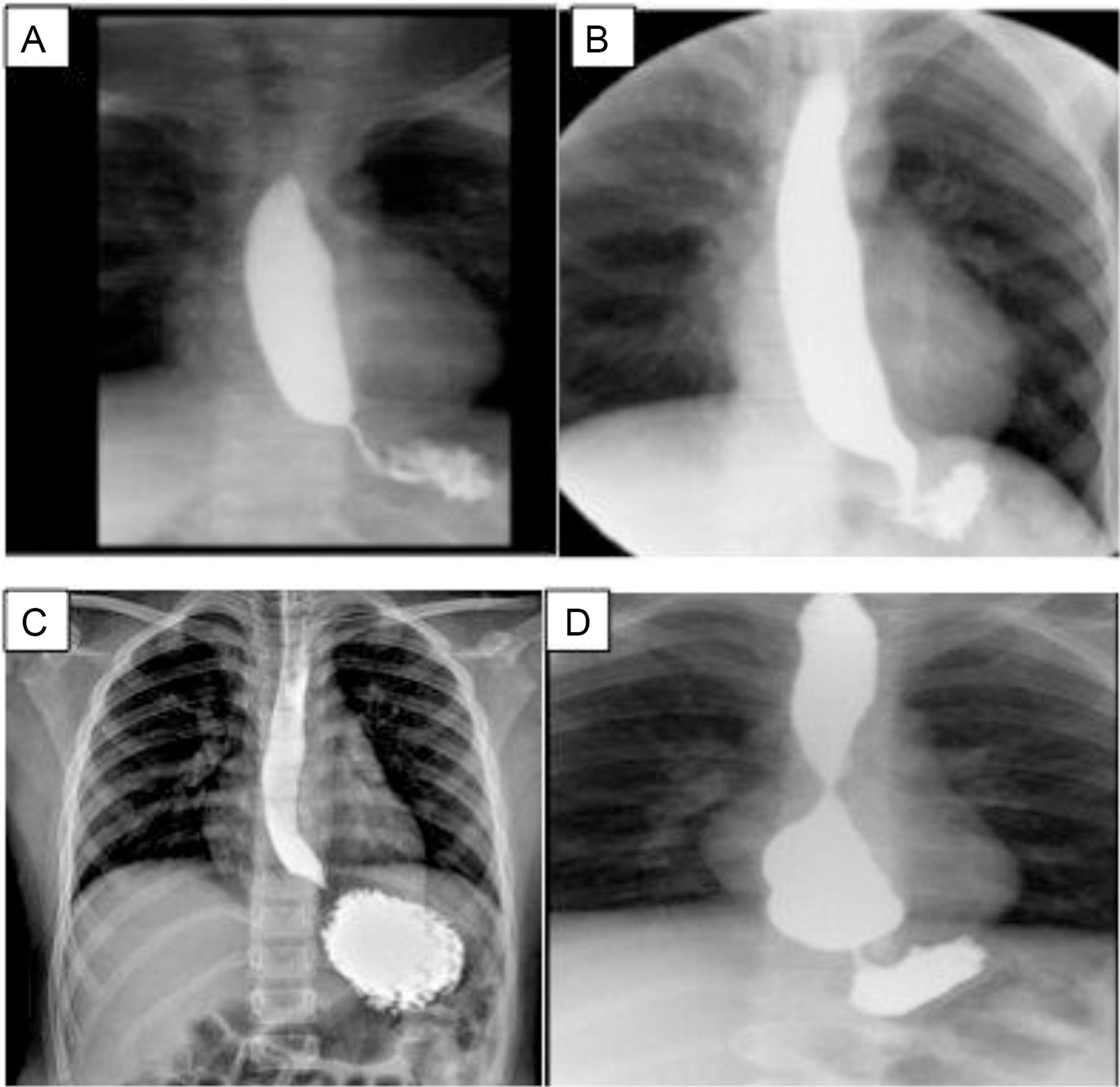
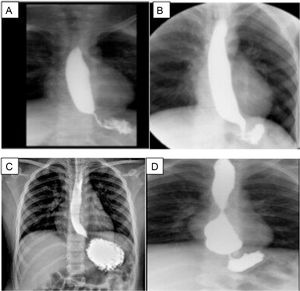
The four patients presented with dysphagia after the surgical procedure, at a mean of 2 weeks (2 ± 1.2 weeks). Therefore, the first diagnostic test carried out was an esophagram, which revealed stricture of the esophagogastric junction (EGJ) in all four cases (Fig. 2A-D). The patients then underwent endoscopy. In two patients, passage of the endoscope was difficult, there was angulation at the EGJ in one patient, and endoscopy was normal in one patient.
Esophagram of the patients after fundoplication.
A) Case 1, overdistension of the esophageal lumen upon the passage of barium. The esophagogastric junction (EGJ) is seen under the diaphragm; B) Case 2, narrowness of the EGJ; C) Case 3, the esophagus is slightly overdistended in its three thirds, with thinning of the EGJ; D) Case 4, esophagus with conserved caliber in the first two thirds, but greatly augmented in the distal third, blunt tip, and even a rounded image, and reduced caliber of the EGJ, probably overefficiency of the fundoplication.
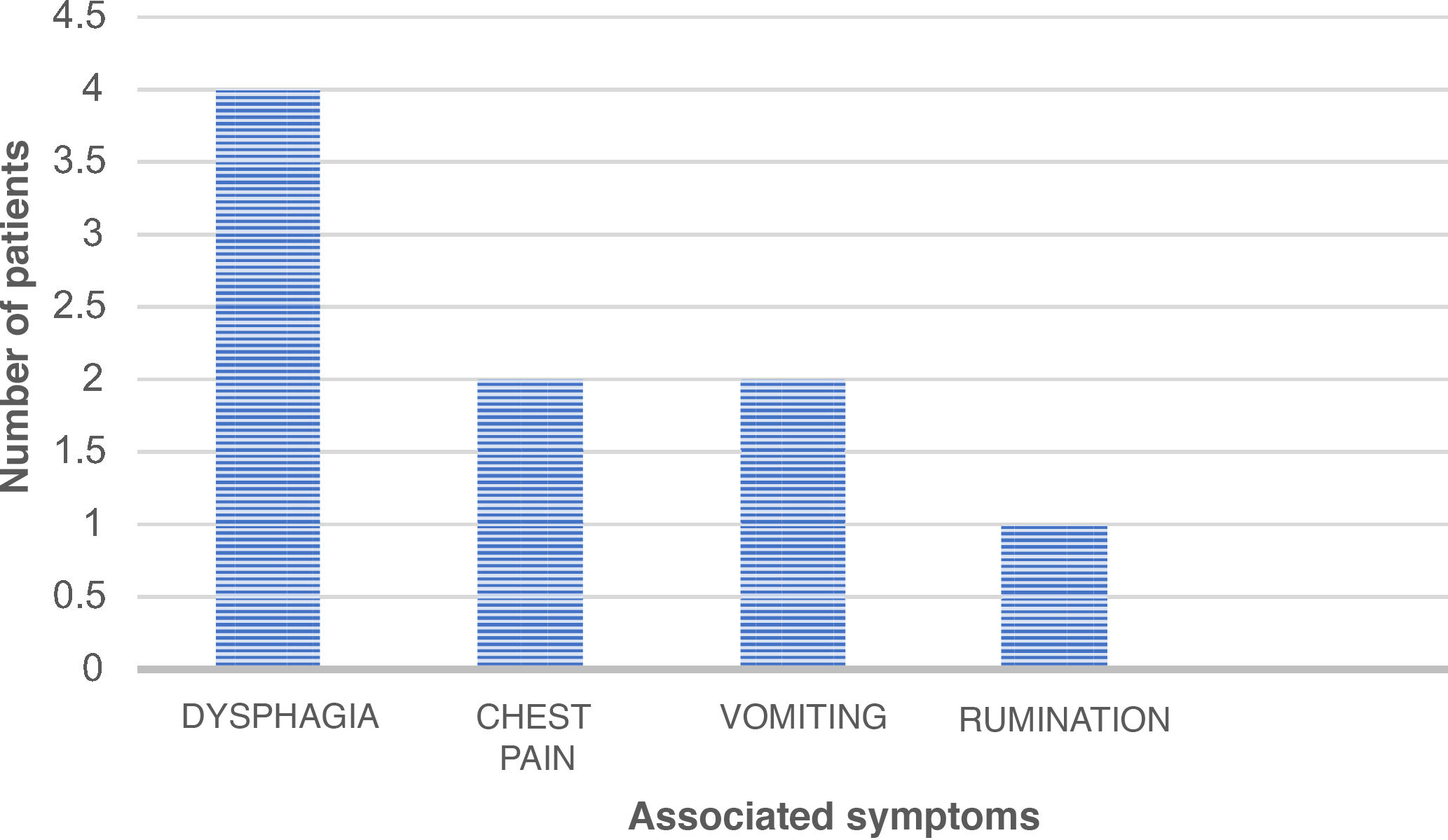
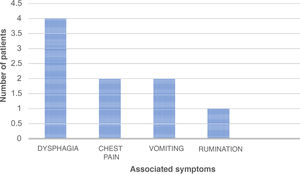
The primary symptom complaints were dysphagia, chest pain, and vomiting (Fig. 3). Initial treatment was dilation in the four patients. Balloon dilation was performed by the surgery service and endoscopic dilation (Savary-Miller) by the gastroenterology service in one patient, and in the remaining three cases, dilation was exclusively carried out with the Savary-Miller probe. None of the patients had improvement at 6 months after treatment. In the first patient, two series of dilations were carried out, followed by fundoplication repair with a Heller myotomy, with no improvement. In the second, third, and fourth patients, two, one, and four series of dilations were performed, respectively.
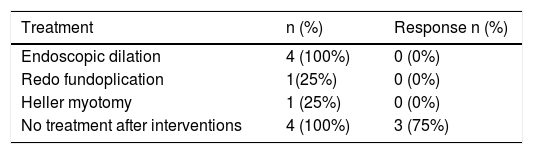
Given the persistence of the dysphagia, watchful management with prokinetics was decided upon, monitoring patient weight and height. Three of the patients had spontaneous symptom improvement but one patient remained symptomatic (Table 2). Mean favorable esophageal symptomatology response was 31 months (mean: 31 ± 8.48 months). Manometry was performed at a mean of 19 post-fundoplication months (mean: 19.45 ± 20 months). Control manometry was only possible in the patient that underwent fundoplication repair, and it showed LES relaxation, one year from the onset of clinical manifestations.
Treatment and response of patients with EGJOO.
| Treatment | n (%) | Response n (%) |
|---|---|---|
| Endoscopic dilation | 4 (100%) | 0 (0%) |
| Redo fundoplication | 1(25%) | 0 (0%) |
| Heller myotomy | 1 (25%) | 0 (0%) |
| No treatment after interventions | 4 (100%) | 3 (75%) |
All the patients underwent esophageal dilatations and one patient also had Heller myotomy plus redo fundoplication.
Since its description in 1956, fundoplication has been a therapeutic option in the management of medical treatment-refractory reflux.10 Given its complexity, secondary postoperative effects, such as dysphagia, can be a problem. Transitory dysphagia occurs within the first weeks in up to 76% of the cases, and severe or recurrent dysphagia can occur in up to 5.3% of pediatric cases.1,2 At our center, we found that 2.8% of patients developed post-fundoplication dysphagia but we do not know if all the patients with that symptomatology were referred to the motility unit for their evaluation. In our study, symptoms presented within the first two weeks after the procedure and persisted for more than four weeks. Studies on adults have reported that transitory dysphagia can occur up to the first six weeks after the procedure and is considered persistent, if it lasts for a longer period of time.12
EGJOO is a relatively new diagnosis,4 and according to the Chicago classification, is defined by an elevated IRP and conserved esophageal peristalsis.3,13–15 In an adult population, Wilshire et al.12 found that up to 64% of patients with post-fundoplication dysphagia had evidence of EGJOO that was demonstrated manometrically by elevated IRP. Very little is known about the pathology in pediatric patients and the published studies are limited to adult populations. Different authors have reported a prevalence of EGJOO that ranges from 3.3-14%, figures very close to ours (2%).16–18
In the present study, we identified four patients with EGJOO secondary to fundoplication, diagnosed utilizing HREM and finding elevated IRP (mean: 24.25 ± 3.90 mmHg). Mean patient age was eight years, with a male to female ratio of 3:1, unlike the adult population, in which two-thirds of the patients are women.13,19
As far as we could tell from our review of the literature, the most frequent manifestation is dysphagia (57-96%),8,20 usually associated with obstructive cases (42%), such as hiatal hernia, esophageal stricture, cancer, and having undergone surgery. Surgery is the associated event found in half of the patients with EGJOO.15
In our study, 75% of the patients had undergone Nissen fundoplication, but previous studies make no mention of an association between the type of fundoplication performed and the presence of the motility disorder.20–22
All the patients underwent an imaging study (esophagram) and upper gastrointestinal endoscopy, in the search for gastrointestinal symptom etiology. All cases presented with stricture at the level of the EGJ (one of the endoscopies was reported as normal), which is why dilation was performed as the initial treatment, but the response was unfavorable, given that the dysphagia persisted in the four patients. The success rates reported in the literature are varied. Okeke et al.8 found a favorable response in 12%, whereas Richter and Clayton reported response in 67% of the cases after pneumatic balloon dilation.11
The patient that underwent fundoplication repair plus Heller myotomy did not improve after the intervention, unlike that reported by Scherer et al. Those authors found symptom improvement in 75% of the patients that underwent fundoplication repair and response in 100%20,22 of the patients that had Heller myotomy. Peroral endoscopic myotomy (POEM) has recently been utilized in esophageal motility disorders, including EGJOO, with remission rates of 60%.23
On the other hand, 33-73% of patients have been described to have symptom resolution with no need for any type of intervention.4,13,16 Even though different procedures were carried out on our patients, no improvement was seen after six months of follow-up. Therefore, endoscopic or surgical management was not continued and 75% of the patients had spontaneous resolution at a mean of 31 months after EGJOO diagnosis.
The limitations of our study were the small number of cases and the lack of treatment homogeneity, given that it was dependent on the treating physician. Nevertheless, because there are very few reports in the international literature, we considered showing the experience at our hospital to be important.
ConclusionEGJOO is a manometric finding that is described very little in the pediatric population and should be suspected in all patients that present with post-fundoplication dysphagia. Unfortunately, treatment continues to be a challenge. Even though half of the cases resolve with no need for any intervention, there are still important limitations to defining optimum treatment of this motility disorder.
FundingThere was no source of funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Godoy-Salgado DC, Toro-Monjaraz EM, Padilla-Cortés T, Cadena-León JF, Zárate-Mondragón F, Loredo-Mayer A, et al. Obstrucción del tracto de salida de la union esofagogástrica en el diagnóstico diferencial de disfagia posfunduplicatura en niños. Revista de Gastroenterología de México. 2021;86:253–258.