Colorectal cancer is among the three most common cancers worldwide. Knowledge and identification of suboptimal outcome-associated factors enable comprehensive patient management. The aim of the present study was to present the results of the surgical management of colorectal cancer at a quaternary care university hospital.
Materials and methodsAn observational, analytic, cross-sectional study was conducted. Information was collected on a retrospective cohort of patients diagnosed with colorectal cancer from 2013 to 2017 at the Hospital Universitario Mayor Méderi, Bogotá, Colombia.
ResultsData on 452 patients, within the study period, were collected. A total of 48.5% of the patients were men, the overall complication rate was 24%, the surgical site infection (SSI) rate was 15.38%, anastomotic dehiscence occurred in 4.18% of the patients, bleeding required reoperation in 1.32%, and the intrahospital mortality rate was 7.47%.
ConclusionColorectal cancer management at a university hospital was as beneficial as that provided by other types of hospitals, showing a direct association with complete R0 dissections; low complication rates, according to international reports; and reduced overall morbidity.
El cáncer colorrectal se encuentra dentro de los 3 primeros cánceres a nivel mundial, el conocimiento e identificación de los factores asociados a los desenlaces no óptimos permiten realizar un manejo integral del paciente. El objetivo de este estudio es presentar los resultados del manejo quirúrgico de enfermedad oncológica colo-rectal en un hospital universitario de cuarto nivel.
Materiales y métodosSe realizó un estudio observacional, analítico de corte transversal, se recolectó la información de una cohorte retrospectiva de pacientes con diagnóstico de cáncer colorrectal entre el año 2013 al año 2017 en el Hospital Universitario Mayor Méderi, Bogotá, Colombia.
ResultadosSe recolectaron 452 pacientes durante el periodo de estudio, de estos el 48.5% fueron varones. El porcentaje global de complicaciones fue del 24%, infección del sitio operatorio (ISO) en el 15.38%, dehiscencia de la anastomosis en el 4.18%, sangrado que origina reintervención en el 1.32% y mortalidad intrahospitalaria en el 7.47%.
ConclusiónEl manejo del cáncer colorrectal en un hospital universitario mostró beneficios y resultados similares y comparables con otros tipos de hospitales con manejo frecuente de esta enfermedad, mostrando una asociación directa en disecciones completas R0, con bajas tasas de complicaciones según lo reportado a nivel mundial y disminución de morbilidad global.
Colorectal cancer is one of the most frequent tumors worldwide1. Dietary habits, and certain genetic, occupational, and lifestyle aspects influence its incidence1–3. The risk for developing colorectal cancer throughout life in the general population is calculated at around 5%4. Recent studies indicate that nutritional supplements rich in probiotics and prebiotics can function as chemopreventive agents, and play an important role in removing mutagenic and carcinogenic agents produced by specific bacteria of the gastrointestinal tract. They also aid in the prevention of colon cancer, through their role in reducing intestinal pH and their immunomodulatory effects3.
The histopathology in the majority of cases of colorectal cancer is adenocarcinoma. It is generally preceded by an adenoma (accepted as occurring in 95% of cases) that progresses to carcinoma5,6. When more than one primary tumor is simultaneously diagnosed at the time of initial presentation, it is known as synchronous colorrectal cancer and its incidence ranges from 1 to 7%; metachronous disease is when a second primary tumor is diagnosed during follow-up4. The anatomic distribution of colorectal cancer corresponds to 30% in the rectum, 20% in the sigmoid colon, 20% in the right colon, and 10% in the left colon or the transverse colon5. Better quality screening has contributed to more efficient detection of precursor lesions and early tumors. The treatment of choice is curative, as well as palliative, surgery5. Optimal patient selection and adequate surgical intervention impact the final surgical result and the 5-year survival rates.
Laparoscopy is the most frequent approach and has become standard care, given that it is shown to be safe and provide good short-term results. Among its advantages are less blood loss, shorter hospital stay, and faster bowel function recovery7. The open technique is the second-place approach and the transnasal technique is the third-place approach. The choice of approach should be based on the principles of oncologic surgery5. The most common procedure-related complications are anastomosis dehiscence and surgical site infection; organized fistulas and contiguous organ lesions, among others, are less frequent8.
Adjuvant therapy is offered after surgery to reduce the possibility of disease recurrence and to increase survival. Candidates for that management are patients with stage II and stage III disease, that have follow-up utilizing clinical, pathologic, and molecular biomarkers1.
Outcomes can be conditioned by the preoperative characteristics of the patient, including disease involvement, comorbidities, nutritional status, and others9. There is scant knowledge about the risk factors for morbidity and mortality after right oncologic colectomy for colon cancer. Such information would be useful for developing prevention and intensive follow-up strategies for at-risk patients9.
Knowing the outcome-related factors is decisive in terms of complications, morbidity, and mortality in patients that undergo colorectal cancer surgery in the local context and encompasses the specific characteristics of the Colombian population. Close to 100 colectomies are performed annually at the institution described in the present study, providing important data.
MethodsPopulationAn observational cross-sectional study was conducted, with retrospective data collection. The study population was made up of patients that underwent surgery for colorectal cancer at the coloproctology service of the Hospital de Méderi, in Bogotá Colombia, from 2013 to 2017.
Data collectionData from the 5-year study period were collected on patients that were surgically managed for colorectal cancer. The patients were above 18 years of age, had a histopathologic diagnosis of colorectal cancer, and were operated on at our health institution. Patients that had been treated or followed at another institution were excluded. All the study patients received multidisciplinary management by the general surgery (colorrectal surgery) service and were operated on by a colorectal surgeon.
The information collected included the sociodemographic variables of age and sex, as well as body mass index (BMI), preoperative nutritional evaluation, comorbidities, and the American Society of Anesthesiologists (ASA) classification. The tumor-related aspects analyzed were primary site, histology, final tumor staging, and regional lymph node classification. The procedure-related variables were procedure intention, surgical approach, blood loss volume, number of resected lymph nodes, compromised organs, resection margins, need for postoperative drain, need for endoanal tube, and hospital stay duration. Regarding the follow-up, the variables of adjuvant therapy and relapse were analyzed. Complications and outcomes were reviewed.
Statistical analysisThe statistical analysis was carried out, utilizing the SPSS® v22 program, under the license of the Universidad del Rosario. In the univariate analysis, the qualitative variables were expressed as percentages and absolute frequencies and the quantitative variables as measures of central tendency and dispersion. The bivariate analysis utilized the Pearson chi-square test as a hypothesis test, and statistical significance was set at a p ≤ 0.05. The present study is considered a no-risk analysis, according to Resolution 8430 of 1993.
Ethical considerationsThis study was approved by the ethics committee of our institution. The protocol was carried out, according to the guidelines of the World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects, adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, and revised in Tokyo 2004.
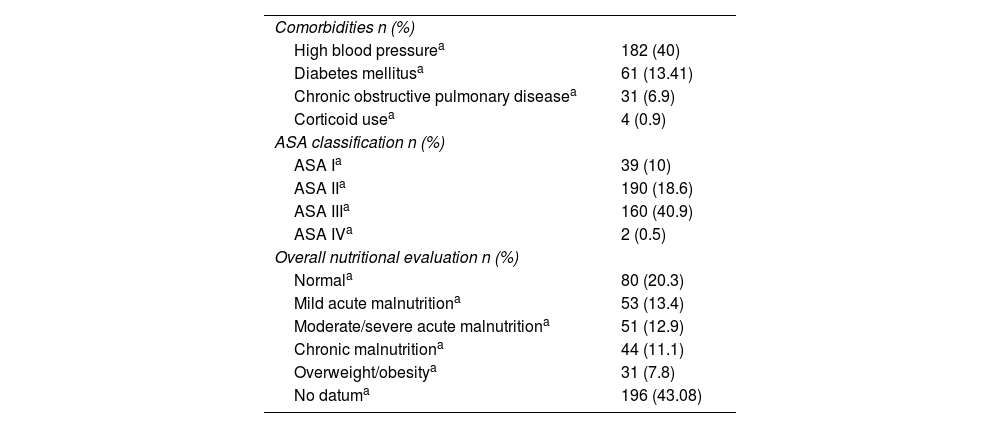
ResultsData from January 2013 to December 2017 were collected, resulting in 452 patients, of whom 48.5% were men and 51.5% were women. The mean patient age was 67 years (SD of 12.5 years). A specialized nutritional evaluation was carried out on 282 patients and showed that 52% had some grade of malnutrition. Table 1 shows the comorbidities, ASA classification, and nutritional status of the patients.
Preoperative characteristics n = 452.
| Comorbidities n (%) | |
| High blood pressurea | 182 (40) |
| Diabetes mellitusa | 61 (13.41) |
| Chronic obstructive pulmonary diseasea | 31 (6.9) |
| Corticoid usea | 4 (0.9) |
| ASA classification n (%) | |
| ASA Ia | 39 (10) |
| ASA IIa | 190 (18.6) |
| ASA IIIa | 160 (40.9) |
| ASA IVa | 2 (0.5) |
| Overall nutritional evaluation n (%) | |
| Normala | 80 (20.3) |
| Mild acute malnutritiona | 53 (13.4) |
| Moderate/severe acute malnutritiona | 51 (12.9) |
| Chronic malnutritiona | 44 (11.1) |
| Overweight/obesitya | 31 (7.8) |
| No datuma | 196 (43.08) |
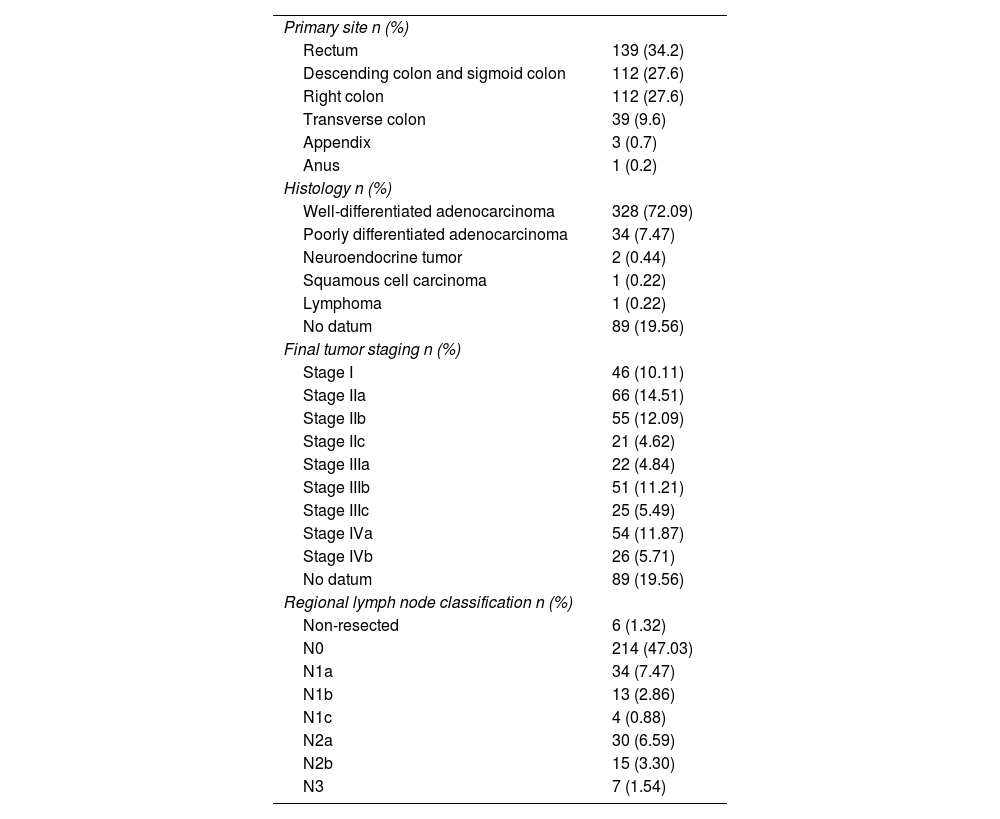
Preoperative staging could be verified in 77.58% (n = 353) of the patients and lymph node classification in 71%. Table 2 describes the tumor characteristics.
Tumor characteristics n = 452.
| Primary site n (%) | |
| Rectum | 139 (34.2) |
| Descending colon and sigmoid colon | 112 (27.6) |
| Right colon | 112 (27.6) |
| Transverse colon | 39 (9.6) |
| Appendix | 3 (0.7) |
| Anus | 1 (0.2) |
| Histology n (%) | |
| Well-differentiated adenocarcinoma | 328 (72.09) |
| Poorly differentiated adenocarcinoma | 34 (7.47) |
| Neuroendocrine tumor | 2 (0.44) |
| Squamous cell carcinoma | 1 (0.22) |
| Lymphoma | 1 (0.22) |
| No datum | 89 (19.56) |
| Final tumor staging n (%) | |
| Stage I | 46 (10.11) |
| Stage IIa | 66 (14.51) |
| Stage IIb | 55 (12.09) |
| Stage IIc | 21 (4.62) |
| Stage IIIa | 22 (4.84) |
| Stage IIIb | 51 (11.21) |
| Stage IIIc | 25 (5.49) |
| Stage IVa | 54 (11.87) |
| Stage IVb | 26 (5.71) |
| No datum | 89 (19.56) |
| Regional lymph node classification n (%) | |
| Non-resected | 6 (1.32) |
| N0 | 214 (47.03) |
| N1a | 34 (7.47) |
| N1b | 13 (2.86) |
| N1c | 4 (0.88) |
| N2a | 30 (6.59) |
| N2b | 15 (3.30) |
| N3 | 7 (1.54) |
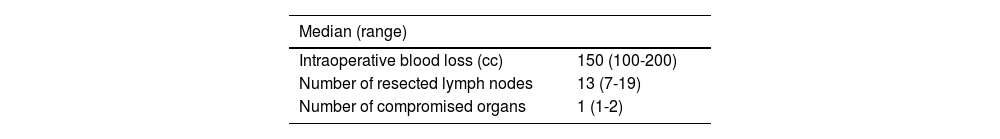
Regarding the procedure, curative-intent treatment was carried out in the majority of patients (74.5%) (n = 339), median hospital stay was 5 days (minimum of one day and maximum of 353 days), and the laparoscopic approach was the most widely utilized (75% versus 25% with the open approach). Table 3 shows the variables related to the procedure.
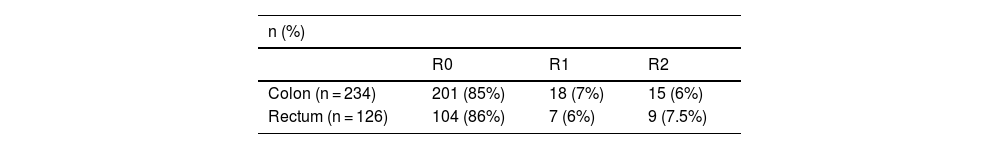
The resection margins were analyzed, according to tumor location, in the colon or in the rectum (Table 4).
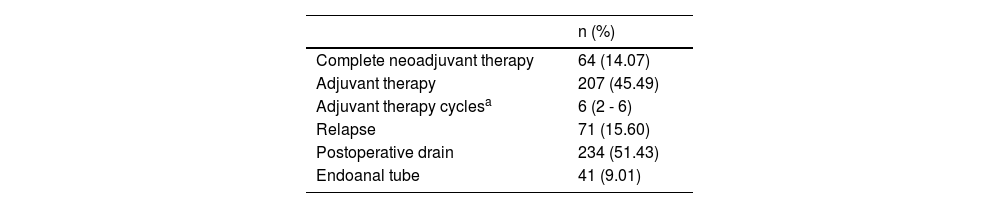
In reference to follow-up, 80 patients received neoadjuvant therapy and 64 received complete neoadjuvant therapy, depending on the criterion of the treating surgeon (Table 5).
Treatment (n = 452).
| n (%) | |
|---|---|
| Complete neoadjuvant therapy | 64 (14.07) |
| Adjuvant therapy | 207 (45.49) |
| Adjuvant therapy cyclesa | 6 (2 - 6) |
| Relapse | 71 (15.60) |
| Postoperative drain | 234 (51.43) |
| Endoanal tube | 41 (9.01) |
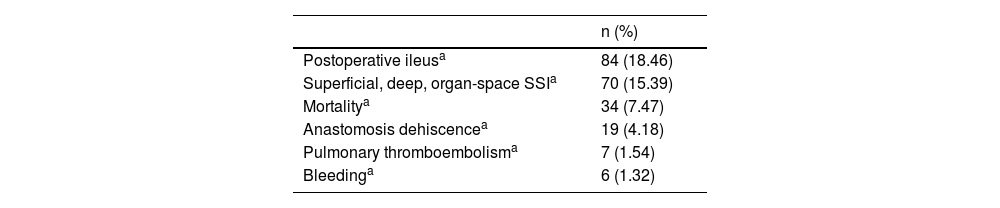
Twenty-four percent (n = 108) of the patients presented with complications, which are described in Table 6.
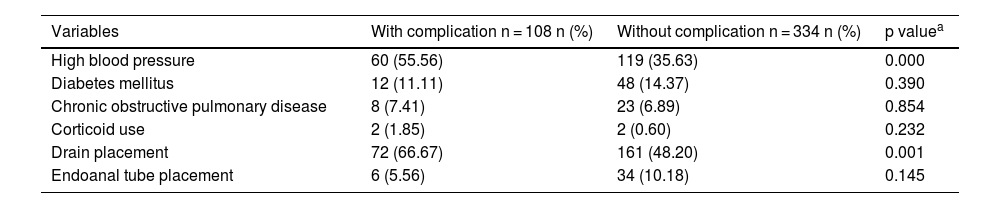
According to the bivariate analysis, the postoperative complications were high blood pressure and the need for drain placement (Table 7).
Procedure comorbidities and characteristics versus complications.
| Variables | With complication n = 108 n (%) | Without complication n = 334 n (%) | p valuea |
|---|---|---|---|
| High blood pressure | 60 (55.56) | 119 (35.63) | 0.000 |
| Diabetes mellitus | 12 (11.11) | 48 (14.37) | 0.390 |
| Chronic obstructive pulmonary disease | 8 (7.41) | 23 (6.89) | 0.854 |
| Corticoid use | 2 (1.85) | 2 (0.60) | 0.232 |
| Drain placement | 72 (66.67) | 161 (48.20) | 0.001 |
| Endoanal tube placement | 6 (5.56) | 34 (10.18) | 0.145 |
In the Western world, colorectal cancer is one of the most common cancers, in order of frequency, and is a disease that has a determining influence on lifestyle habits. Early detection through the screening of precursor lesions, in this case, adenomas, is possible1,6,10. Colorectal cancer is 2-times more frequent in men than in women and presents with associated inflammatory bowel diseases and polypoid lesions3. The risk of developing or progressing to colorectal cancer is associated with genetic, socioenvironmental, and exposure factors, leading to the decision to carry out interdisciplinary management of the tumor1,6.
According to the figures from the international agency for the study of cancer, there was an estimated 9.7% prevalence of colorectal cancer in 2015 worldwide, among all cancer cases1, whereas according to data from the 2012 GLOBOCAN project, incidence varied widely, from 3-4/100,000 inhabitants in the African Northeast to 40/100,000 inhabitants in European studies, with better screening systems3,11. Recently, a decrease in the number of expected cases in adults over 50 years of age has been calculated. Nevertheless, an increase of said incidence is expected for 20303. Surgery is the therapeutic intervention with the possibility of cure in patients with stages I, II, and III of the disease, and must adhere to the principles of oncologic surgery, conserving wide resection margins in both the laparoscopic and the open techniques10. A retrospective cohort of patients that underwent colorectal surgery was analyzed in the present study, showing the characteristics and outcomes at an important health institution in Colombia.
Unlike that described in the international literature, we found a slightly higher number of women that were operated on, congruent with the results of Agudelo et al., who reported that 57% of the procedures were performed on women8. However, the incidence of colorectal cancer worldwide is higher in men1,9. In their study, Frasson et al. found that 60% of the patients undergoing colorectal surgery were men and 40% were women. Forty percent of the patients had a risk for ASA III, similar to that reported in other studies12.
The most prevalent comorbidity in the patients with colon cancer was high blood pressure, at 40%, similar to that reported by Pellino et al., who documented it in 52.8% of the patients included in their study13.
In the study by Frasson et al., they included 3,193 patients from 52 European hospitals. The location of the tumors was similar, with around 30% involving the right colon and less than 10% involving the transverse colon12. Thirty-four percent of the tumors were located in the rectum.
In the statistics previously reported by Agudelo et al., those authors found a frequency of operated patients with stage IV, disease of 26.2% in 20128, compared with 11.7% in the present study. That could reflect improved screening strategies in Colombia, is relevant, given the different studies that describe a decrease of up to 67%, with respect to the colorectal cancer mortality rate, through adequate screening systems14–16. Nevertheless, in international studies, the surgery rate for patients in stagehas been reported from 8.5 to 10.5%9,12.
In addition, there has been an increase in the performance of laparoscopic interventions. In 2014, it was used in 60% of cases8, and in our study, rose to 75%. Numerous studies support the lower complication rate, thanks to the less invasive nature of the laparoscopic procedure7, as concluded by Bedrikovetski et al., in their comparative study on the open technique versus the minimally invasive technique in colorectal cancer surgery17.
With respect to intervention outcomes, we found that the main complication was postoperative ileus, followed by surgical site infection, in 15.39% of the patients, which was higher than the 13.4% described in the prospective ANACO study in 2015. The most dreaded complication in the context of surgical treatment of colon cancer is dehiscence18, whose rate was 4.18%. Local researchers have reported dehiscence rates of 4.6%8, whereas the ANACO researchers reported a rate of 8.4% and found obesity, intraoperative complications, low preoperative serum protein levels, and male sex to be associated factors.
The ANACO study group brought together the prospective data of 52 countries, with a sample of 3,193 patients. They characterized the patients that underwent cancer-related resection of the colon and analyzed the risk factors for dehiscence. They documented a 3% mortality rate, which was low, compared with our mortality rate of 7.47%12. The overall complication rate in our study was 23.7%, which was lower than the 27% established worldwide at centers of excellence in multicenter studies9.
Evaluating the nutritional condition of patients is an aspect that needs to be improved, given that only 61% of the patients from the entire cohort had such an assessment, and it was carried out more rigorously and frequently during the last years of the study period. An ever-increasing number of reports are supporting the importance of adequate nutritional status for obtaining better perioperative outcomes12,13.
Achieving complete R0 dissections is associated with a reduction in overall morbidity and recurrence rates. In our study, the recurrence rate decreased in direct proportion to the number of dissected lymph nodes. Importantly, the mean for lymph node dissection (13 lymph nodes) at our institution is higher than the number established in the literature as the minimum for favoring an increase in survival rates9.
The main limitation of our study was the fact that it is a comparative observational study with no randomization, and thus, is subject to selection bias.
The results of the present study provide valuable information on the characteristics of the Colombian population operated on for colon cancer, for detecting strengths and aspects to improve, as well as for consolidating information to make comparisons, with both national and international references.
ConclusionsThe sociodemographic characteristics of the patients operated on for colon cancer at our health institution were similar to those of the worldwide population.
Our hospital has a low dehiscence rate and overall complication rate, compared with international statistics. Complete R0 dissection decreased the morbidity and mortality of the hospitalized patient. It is important to evaluate the causes of overall mortality, which should be done through prospective studies, so that the associated factors can be more deeply explored, resulting in opportunities for improvement.
The preoperative evaluation of nutritional condition should be a sine qua non to aid in having better results, during and after the intervention.
According to the results of the present study, special caution should be exercised, regarding patients with high blood pressure and those with intraoperative drains, given that they are aspects associated with complications, which should be analyzed in depth, through prospective studies.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Romo JA, Aguilera PA, López A, Pedraza M, Figueroa C. Experiencia en cirugía colorrectal en un hospital de cuarto nivel de complejidad en Bogotá, Colombia. Rev Gastroenterol Méx. 2023;88:214–219.