The frequency of gastric ischemia is low due to the rich blood supply of the stomach. It can be caused by vascular insufficiency, thrombosis, vasculitis, etc1. Factors, such as advanced age, smoking, and diabetes, can reduce gastric and splenic circulation1,2. The most common symptoms are abdominal pain, bleeding, and altered mental status1 and laboratory tests tend to report leukocytosis and elevated C-reactive protein and liver enzymes3. Pneumatosis is characterized by the presence of gas vesicles in the intestinal wall4. In a meta-analysis of studies conducted over the past 5 years, a frequency of just 500 cases was found, with 30% of cases reported in the United States and 1.14% in Latin America5. Its pathophysiology is unclear, albeit there are 2 important theories: the mechanical theory suggests that the increase in intraluminal pressure forces the entrance of air into the gastrointestinal wall through defects in the mucosa, and the bacterial theory states that it is the result of the accumulation of gas produced by bacteria after their translocation6. Its manifestations and imaging study results are generally not conclusive, making exploratory surgery necessary for making the diagnosis2. Pneumatosis of the gastric wall is suggestive of ischemia and implies compromised circulation, despite the rich vascular supply of the stomach. In addition, the distribution of gas becomes important, given that a bullous pattern is related to benign conditions, whereas a linear pattern is related to more dangerous entities4,5.
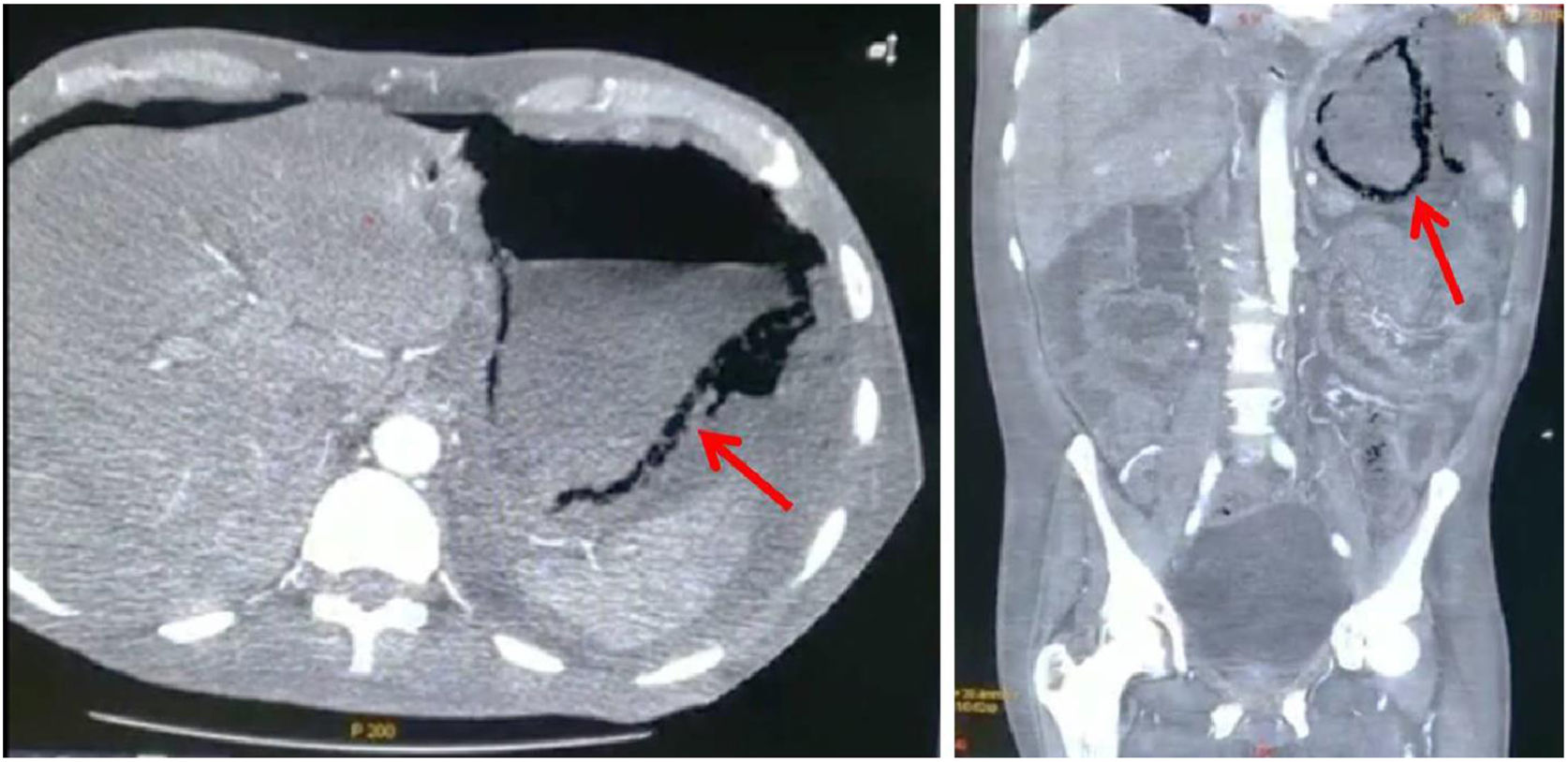
A 57-year-old man with diabetes and high blood pressure, who quit smoking, was admitted to the hospital due to changes in the color of the toes on his right foot, prolonged capillary refill time, local hypothermia, and necrotic zones with no signs of infection. Diabetic foot (PEDIS classification grade 4) and chronic kidney disease were diagnosed. During hospitalization, the patient presented with absence of metabolic control and he developed acidosis. Peritoneal dialysis was begun, with the percutaneous placement of a Tenckhoff catheter. Due to drainage of turbid fluid, antibiotic therapy with ceftriaxone and clindamycin was administered. The patient presented with abdominal pain, a positive rebound sign, reduced peristalsis, and hypotension. Given the suspicion of intestinal infection, the drug regimen was changed to meropenem, fungal prophylaxis, and metronidazole. A computed tomography scan identified emphysematous gastritis and free air in the cavity (Fig. 1). Laboratory tests were ordered (Table 1) and an exploratory laparotomy was performed. During the event, purulent fluid was drained from the abdominal cavity. Multiple adhesions were observed in the cardia and removed. Areas of necrosis were also identified from the pylorus to the esophagus. An orogastric tube was placed and the gastric content was aspirated, partially improving perfusion. The washout was continued with warm solutions. Due to the critical status of the patient that persisted with hypotension and hypoglycemia, the decision was made to end the surgical act for maximum benefit. However, the patient continued to present with shock and lack of metabolic control, and voluntary discharge by family request was granted.
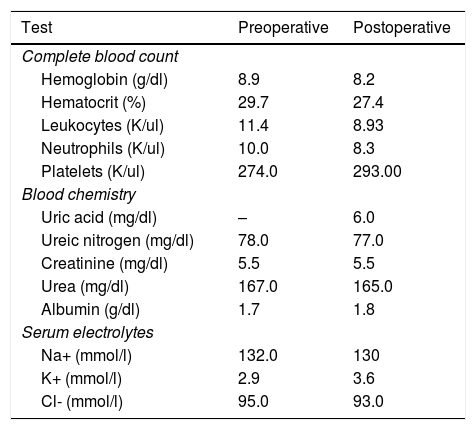
Laboratory tests before and after the exploratory laparotomy.
| Test | Preoperative | Postoperative |
|---|---|---|
| Complete blood count | ||
| Hemoglobin (g/dl) | 8.9 | 8.2 |
| Hematocrit (%) | 29.7 | 27.4 |
| Leukocytes (K/ul) | 11.4 | 8.93 |
| Neutrophils (K/ul) | 10.0 | 8.3 |
| Platelets (K/ul) | 274.0 | 293.00 |
| Blood chemistry | ||
| Uric acid (mg/dl) | – | 6.0 |
| Ureic nitrogen (mg/dl) | 78.0 | 77.0 |
| Creatinine (mg/dl) | 5.5 | 5.5 |
| Urea (mg/dl) | 167.0 | 165.0 |
| Albumin (g/dl) | 1.7 | 1.8 |
| Serum electrolytes | ||
| Na+ (mmol/l) | 132.0 | 130 |
| K+ (mmol/l) | 2.9 | 3.6 |
| Cl- (mmol/l) | 95.0 | 93.0 |
The finding of emphysematous gastritis was conclusive for diagnosing gastric ischemia caused by celiac trunk thrombosis in our patient, who was diabetic and had high blood pressure. He also presented with grade 5 chronic kidney disease, which produces a hypercoagulable state. There are factors in intestinal necrosis that provide information that increases the probability of making the correct diagnosis and defining the management to be carried out and they include arterial hypertension, dyslipidemia, a history of myocardial ischemia or ischemia of the extremities, organ failure, leukocytosis, elevated serum lactate, alterations in intestinal wall thickness, and intestinal segment dilation. Those factors increase the probability of death, which reaches up to 40% when 3 of said factors are present2,4,7. Drucker et al. reported that pneumatosis can be associated with ischemia and it can be accompanied by the tomographic identification of air in the portal vein8, which is a datum that should be consciously looked for. Unfortunately, our patient did not present with it2,4, and the pneumatosis had a linear distribution that was not of much help in determining the management to follow, given that it presented in the stomach9. Treatment can be surgical or conservative, with the correction of any fluid and electrolyte imbalance. Drucker et al. presented a case in which hydrating the patient and placing a nasogastric tube was the preferred treatment10, albeit surgical intervention can also be an option. In the study by Spektor et al., they found that gastric pneumatosis plus elevated serum creatinine and lactic acid levels were associated with higher mortality, and so those elements should be taken into account in the management decision3,9. Nevertheless, it is necessary to evaluate the status of each patient and be aware that the extension of the ischemia, risk factors, and tomographic findings play a role in deciding on the treatment to be followed2,3,9.
FundingThere was no source of funding.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: González-Palacio CL, Venegas-Yáñez CE, Enríquez-Sánchez LB, Carrillo-Gorena MJ, Aguirre-Baca A. Reporte de caso: hallazgo de neumatosis gástrica en tomografía axial computarizada como signo de isquemia gástrica secundaria a probable trombosis en paciente con enfermedad renal crónica. Revista de Gastroenterología de México. 2021;86:443–445.