The neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and C-reactive protein (CRP) level are simple laboratory test parameters that can provide us with information on the inflammatory status of the organism. CRP has been shown to be a predictor of postoperative complications, whereas NLR and PLR have shown greater usefulness in the prognosis of oncologic pathologies.
AimTo evaluate the associations of NLR and PLR with postoperative complications following gastric oncologic surgery and compare them with CRP.
Materials and methodsA prospective study was conducted on 66 patients that underwent oncologic gastric surgery, within the time frame of January 2014 and March 2019. The variables analyzed were sociodemographic data, surgical technique, tumor extension, and NLR, PLR, and CRP levels from the first day after surgery, as well as postoperative complications.
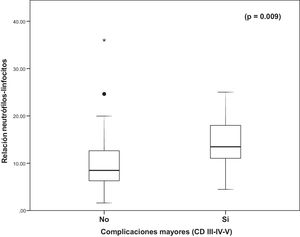
ResultsSeventeen patients (25.8%) presented with grade III-V complications, utilizing the Clavien-Dindo classification system. Mean NLR value was 11.30 and was associated with the appearance of major complications, with statistical significance (p = 0.009). Mean PLR was266.05 and was not significantly associated with complications (p = 0.149). Fifty-four patients had a mean CRP level of 143.24 and it was not related to the appearance of major complications (p = 0.164).
ConclusionsThe NLR is a simple and inexpensive parameter, which measured on postoperative day one, predicted the appearance of major postoperative complications in our study sample and appears to be a better predictive parameter than CRP for said complications. Further studies to confirm that trend need to be carried out.
La Relación Neutrófilo-Linfocito (NLR, por sus siglas en inglés “Neutrophil-to-Lymphocyte Ratio”), la Relación Plaqueta-Linfocito (PLR, por sus siglas en inglés “Platelet-to-Lymphocyte Ratio”) y la Proteína C Reactiva (PCR) son parámetros analíticos sencillos que pueden informarnos sobre el estado inflamatorio del organismo. La PCR ha mostrado ser predictor de complicaciones postoperatorias, mientras la NLR y la PLR han mostrado mayor utilidad en el pronóstico de patologías oncológicas.
ObjetivoEvaluar la asociación de NLR y PLR con las complicaciones postoperatorias tras cirugía oncológica gástrica y compararlo con la PCR.
Material y métodosSe realizó un estudio prospectivo sobre 66 pacientes sometidos a cirugía gástrica oncológica entre enero de 2014 y marzo de 2019. Se tomaron variables sociodemográficas, técnica quirúrgica, extensión tumoral, NLR, PLR y PCR del primer día postcirugía y complicaciones postoperatorias.
Resultados17 pacientes (25.8%) presentaron complicaciones grado III-V de la Clasificación de Clavien-Dindo. El valor NLR medio fue 11.30 y se asoció de forma estadísticamente significativa con la aparición de complicaciones mayores (p = 0.009). El PLR medio fue 266.05 y no se asoció de forma significativa con las complicaciones (p = 0.149). La PCR media de 54 pacientes fue 143.24 y no se relacionó con la aparición de complicaciones mayores (p = 0.164).
ConclusiónEl NLR es un parámetro sencillo y barato, y en nuestra muestra, predice la aparición de complicaciones mayores postoperatorias desde el primer día. En comparación con la PCR precoz, parece ser un mejor parámetro predictor de las mismas. Se deben realizar estudios más amplios para confirmar esta tendencia.
The neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR) are laboratory test parameters that show the inflammatory status of the organism. Because they are parameters that are easily obtained, there is scientific evidence on their utility in predicting cardiovascular mortality risk,1 different types of cancer,2 and the severity of infectious pathologies, such as acute appendicitis.3
In addition, a relation to postoperative complications of specific surgical diseases, such as gastric cancer4 or rectal cancer,5 has been found.
C-reactive protein (CRP) is another parameter that has been shown to be a predictor of postoperative complications. Although stronger in relation to colorectal disease,6,7 it has also been described in gastric surgery8 and pancreatic surgery,9 among others.
The aim of our study was to evaluate the relation of postoperative-day-one NLR and PLR to complications following gastric oncologic surgery and compare them with postoperative-day-one CRP.
Materials and methodsA prospective and observational study was conducted on 66 consecutive patients that underwent gastrectomy within the time frame of January 2014 and March 2019. The study was carried out at a referral hospital that serves a population of approximately 400,000 inhabitants and was authorized by the Clinical Research and Ethics Committee of the hospital center.
The variables included the demographic data of age and sex, as well as comorbidities and oncologic data (gastric tumor type and extension). Type of gastric tumor was divided into adenocarcinoma and other types of tumor. The TNM system (Eighth edition)10 was used to describe tumor extension. Neoadjuvant chemotherapy was indicated for patients with preoperative tumor stages II-III.
All the patients were preoperatively evaluated by a surgeon and an anesthesiologist. The indication for gastrectomy was usually based on the results of upper endoscopy and biopsy. After a complete laboratory work-up, and according to the underlying disease, a series of complementary studies were requested, that included chest x-ray, electrocardiogram, and chest and abdominal computed tomography.
To perform the gastrectomy, both the open surgery and laparoscopic approaches were carried out via the abdominal cavity. Once the abdominal cavity was examined, the two curvatures were freed, usually with the accompanying omentum, from the esophagogastric junction to 2 cm below the pylorus for total gastrectomies and from 4-5 cm below the cardia to the pylorus for subtotal gastrectomies. Sectioning and reconstruction, through esophagojejunostomy or Billroth II gastrojejunostomy, were carried out with automated suturing devices. D2 lymph node dissection was performed in cases with neoplastic processes.
On postoperative day one, a complete blood count was ordered in all patients to determine the NLR and PLR. CRP levels (mg/l) were quantified in all patients with a preoperative diagnosis of adenocarcinoma.
The postoperative complications were ranked utilizing the Clavien-Dindo classification system,11 which stratifies patients into six groups, according to severity, in which 0 signifies no complication and 5 is the death of the patient (Table 1).
Postoperative complications according to the Clavien-Dindo classification system.
| Grade | Definition |
|---|---|
| I | Any deviation from the normal postoperative course that does not require surgical, endoscopic, or radiologic intervention. Grade I includes the need for certain drugs (antiemetics, antipyretics, analgesics, diuretics, and electrolytes), treatment with physical therapy, and wound infections that are opened at the bedside. |
| II | Complications requiring drug treatments different from those described in grade I. Grade II includes blood or blood-derivative transfusions and parenteral nutrition |
| III | Complications requiring surgical, endoscopic, or radiologic intervention |
| IIIa | Intervention not under general anesthesia |
| IIIb | Intervention under general anesthesia |
| IV | Life-threatening complications that require treatment in the intermediate or intensive care units |
| IVa | Single organ dysfunction (including dialysis) |
| IVb | Multiorgan dysfunction |
| V | Death of the patient |
For the analysis, complications were categorized into minor complications (grades I-II) and major complications (grades III, IV, and V). The study sample was divided into the following two groups: patients with major complications and patients with minor complications or no complications.
Surgical mortality was defined as any death that occurred within the first 30 days of the postoperative period or during the same hospitalization, if it was directly related to the procedure.
Statistical analysisThe data were analyzed using the SPSS Statistics v. 26 for Windows (IBM Corp, Armonk, NY, USA) software. A descriptive analysis of the sample was first carried out, utilizing frequency and percentage for the qualitative variables and mean (±standard deviation) or median (interquartile range) for the continuous variables. A univariate analysis was then performed between the independent variables described above, including the NLR, PLR, and CRP levels from the immediate postoperative period, and the presentation of major complications. The categorical variables were expressed through the chi-square test or the Fisher’s exact test and the numerical variables were expressed through the Student’s t test or the Mann-Whitney U test, based on whether or not they had a normal distribution. Statistical significance was set at a p < 0.05. Likewise, based on the area of the curve, ROC curves were constructed to define which of the specific markers (NLR, PLR, CRP) better predicted the presentation of postoperative major complications. Finally, the Youden index was calculated to establish the best cutoff point of the continuous variable for making said prediction.
Ethical considerationsInformed consent to participate in the research described above was requested of the patients. The present study met the current bioethics research regulations and was approved by our hospital’s provincial ethics committee. No data or images that could identify any of the patients were included, preserving patient anonymity at all times.
ResultsOf the total of 66 patients, 52 were men (79%) and 14 were women (21%). Mean patient age was 69.5 years. The indications for gastrectomy were adenocarcinoma, which presented in 54 patients (81.2%); gastrointestinal stromal tumors (GISTs), presenting in 6 patients (9.8%); neuroendocrine tumor, in one patient (1.5%); schwannoma, in one patient (1.5%); squamous cell carcinoma, in one patient (1.5%); and adenomatous polyps with dysplasia, in 3 patients (4.5%). Of those cases, 20 patients (30%) underwent total gastrectomy and 46 (70%) underwent subtotal gastrectomy. The approach was laparoscopic in 38 patients (58%). Twenty patients were diagnosed with stage I disease, 31 with stage II, 11 with stage III, and 4 with stage IV. Twenty-two patients (33.3%) received neoadjuvant therapy.
Mean NLR was 11.30 (SD ± 6.44), mean PLR was 266.05 (SD ± 195.36), and mean CRP was 143.24 (SD ± 104.75).
Complications presented in 31 patients (47%), the majority of which were minor. Major complications presented in 17 patients (25.8%), in the following grades: IIIa, in four patients (6.4%); IIIb in seven patients (10.6%); IVa in one patient (1.5%), and grade V in five patients (7.5%).
Regarding the type of complication, two patients (3%) presented with intra-abdominal collections that were treated with percutaneous drainage; five patients (8%) had gastrojejunal anastomosis leakage, four of whom required surgery; two patients (3%) presented with dehiscence of the duodenal stump that was treated with percutaneous drainage; one patient (1.5%) was reoperated on for hemoperitoneum; one patient (1.5%) was reoperated on for ischemia of the gastric remnant; one patient (1.5%) presented with pleural empyema that required surgical thoracic drainage; and five patients (7.5%) died.
The individual causes of surgical mortality in the five patients were: severe acute pancreatitis, duodenal stump leakage, gastrojejunal anastomosis leakage, decompensated cirrhosis of the liver, and hospital-acquired pneumonia with respiratory insufficiency.
The variables of age (p = 0.556), sex (p = 0.676), laparoscopic approach (p = 0.322), type of gastrectomy (p = 0.481), tumor histology (p = 0.709), tumor stage (p = 0.225), and neoadjuvant therapy (p = 0.842) were not related to the presentation of major complications.
The postoperative-day-one NLR had a statistically significant association with the appearance of major complications (p = 0.009) (Fig. 1), but neither the postoperative-day-one PLR (p = 0.149) nor postoperative-day-one CRP level (p = 0.164) were associated with the presentation of complications.
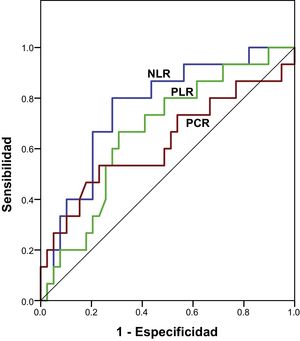
Fig. 2 shows the comparison of the different ROC curves of the NLR, PLR, and CRP parameters and Table 2 shows the areas under the curve. The NLR had greater predictive strength in relation to severe complications (AUC: 0.712; p = 0.009) than the PLR (AUC: 0.618; p = 0.079) and CRP (AUC: 0.623; p = 0.164). Table 3 shows the cutoff point with the highest sensitivity and specificity, according to the Youden index.
Area under the curve of postoperative-day-one neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and CRP, related to the appearance of major complications after gastrectomy due to cancer.
| Variable | Area under the curve | Standard error | p | 95% CI of the area under the curve |
|---|---|---|---|---|
| NLR | 0.76 | 0.07 | 0.003 | 0.62 - 0.90 |
| PLR | 0.67 | 0.08 | 0.061 | 0.51 - 0.82 |
| CRP | 0.62 | 0.09 | 0.164 | 0.44 - 0.80 |
Results of the univariate analysis between the different parameters studied (NLR, PLR, and CRP) and the presentation of major complications after categorizing the variables according to the cutoff point obtained using the Youden Index, in relation to maximum sensitivity and specificity.
| Youden index | Cutoff point | p | OR (95% CI) | |
|---|---|---|---|---|
| NLR | 0.343 | 12.81 | 0.01 | 4.41 (1.37 – 14.12) |
| PLR | 0.321 | 230.29 | 0.0021 | 3.78 (1.19 – 12.06) |
| CRP | 0.303 | 183.50 | 0.032 | 3.81 (1.08 – 13.41) |
Upon categorizing the postoperative-day-one NLR variable according to the cutoff point, a value > 12.8 showed a statistically significant association with postoperative complications (p = 0.01; OR: 4.41; 95% CI: 1.37-14.12), with 4.4-times more possibility of developing major complications than with a value below the cutoff point. The categorized postoperative-day-one PLR value (< 230.3 vs > 230.3) was also related to the presentation of postoperative complications (p = 0.021; OR: 3.78; 95% CI: 1.19-12.06), as was the categorized postoperative-day-one CRP value (< 183.5 vs > 183.5) (p = 0.032; OR: 3.81; 95% CI: 1.08-13.41).
DiscussionThe surgical act is an aggression associated with an acute inflammatory reaction in the organism. That response can be the expected reaction or can be the first manifestation of the appearance of complications derived from the surgery.12
The postoperative inflammatory response can be monitored through different laboratory test parameters throughout the perioperative period. CRP and procalcitonin are two acute phase reactants that are widely studied as predictors of postoperative complications.13
The determination of NLR and PLR has become relevant in recent years, with a growing interest in their roles in predicting oncologic outcomes in different types of cancers (breast, colorectal, gastric, urologic, etc.)14,15 Those parameters are determined upon diagnosis and treatment completion,16 or to restage disease after neoadjuvant treatment.17 Their elevated values have been related to worse treatment response, and in turn, to worse survival rate.18 Those results are explained by the systemic inflammation response of the individual as a theory of the development and progression of the cancer.19
Likewise, those parameters can also be employed to predict postoperative complications. The systemic inflammatory response resulting from a surgical intervention produces alterations in the complete blood count (platelets, neutrophils, and lymphocytes) of patients, and consequently in the NLR and PLR. There are few studies on the determination of those two parameters in the postoperative period after major surgery and their relation to postoperative complications.20
In a case series on 404 patients, Mohri et al.4 found that the variables they analyzed were significantly associated with the appearance of postoperative complications. The patients that presented with an elevated preoperative NLR had a significantly higher risk for developing a postoperative complication after gastric surgery.
Those same results were described by Caputo et al.5, who concluded that an elevated NLR after neoadjuvant therapy, and prior to surgery, was a predictive factor for poor response to oncologic treatment and was a predictor of postoperative complications, as well.
In our study, we determined the NLR on postoperative day one. Joose et al.21 concluded that NLR determination on the first day of the postoperative period could be a confounding factor due to immune system activation, but in 2007, Cook et al.22 were among the first authors to report that postoperative-day-one NLR was useful for predicting postoperative complications.
Even though we could not verify that postoperative-day-one PLR was a useful parameter for predicting postoperative complications, Inaoka et al.23 conducted a case series of 312 patients that underwent oncologic gastric surgery for T2-4 tumors and found that elevated preoperative PLR was a predictor for postoperative complications.
With respect to CRP, its value in predicting postoperative complications has been widely reported in the medical literature, especially in relation to colorectal surgery and the prediction of anastomotic dehiscence.6,7
Few studies have compared the utility of CRP as a predictor of postoperative complications with that of NLR in the postoperative period.
Mik et al.24 established that CRP determined on postoperative day 4 had greater strength for predicting anastomotic dehiscence in colorectal surgery than the NLR, albeit both were useful.
Upon analyzing CRP, NLR, and PLR on postoperative days 1, 3, and 5, Çetin et al.25 concluded that CRP determined on postoperative days 3 and 5 and the NLR determined on postoperative day 5 were good predictors for postoperative complications, whereas the rest of the determinations were not statistically significant.
In our case series, postoperative-day-one CRP determination was not significantly associated with the appearance of postoperative complications. In the comparison of CRP with NLR, the latter showed greater strength in predicting those complications, resulting in its having a higher predictive value in the immediate postoperative period than CRP. We did not compare the CRP and NLR values on the successive postoperative days to determine whether CRP could progressively acquire predictive value, as is reported in the literature.
Our having included several types of gastric tumors in the present case series is an aspect that could have induced different inflammatory responses in the postoperative period and conditioned the technique employed. Nevertheless, we found no such references in the literature we consulted, and our results showed that neither the type of gastrectomy nor the type of tumor were related to the presentation of major complications.
Study limitationsLimitations of the present analysis were the fact that our study was conducted at a single center on a relatively small number of patients and that we did not evaluate the study parameters on postoperative days 3 and 4. However, we believe that our results can be extrapolated to populations that have undergone gastrectomy in our environment, and they showed that a simple parameter (NLR) determined on postoperative day one could predict, with acceptable certainty, the appearance of major complications after said surgery. On the other hand, other possible predictive factors for complications, such as preoperative albumin levels, were not considered.
None of the independent variables, except NLR, were related to the presentation of major complications, which was why we did not perform a multivariate analysis. The lack of statistically significant association could have been due to the small sample size of our analysis. Further studies with larger numbers of patients should be conducted to determine the existence of other possible confounding factors.
ConclusionsThe laboratory test determination of acute phase reactants, complete blood count, and the calculation of the NLR and PLR, are simple and inexpensive measures that, together with the clinical manifestations of the patient, can condition the suspicion of postoperative complications.
In our study sample, postoperative-day-one NLR predicted the appearance of major postoperative complications. Compared with postoperative-day-one CRP, NLR appears to be a better early parameter for predicting those complications. Larger and more homogeneous studies should be conducted to confirm the trend we found.
Financial disclosureNo financial support was received in relation to the present study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ortiz-López D, Acosta-Mérida MA, Casimiro-Pérez JA, Silvestre-Rodríguez J, Marchena-Gómez J. Valor del Ratio Neutrófilo-Linfocito, Ratio Plaqueta-Linfocito y Proteína C Reactiva del primer día como predictores de complicaciones postoperatorias tras cirugía oncológica gástrica. Rev Gastroenterol Méx. 2022;87:142–148.